Cory:
Unlock Your AI Assistant Now!
Environmental concerns related to global warming impact all sectors of society, with healthcare contributing approximately 5% of global greenhouse gas (GHG) emissions – making it the 5th largest emitting entity on the planet. Annually, around 5 million cardiac catheterisation procedures are performed worldwide. Despite this, the healthcare sector is lagging in efforts to reduce GHG emissions, and there is a lack of detailed studies that accurately estimate the emissions generated by specific procedures1. Ditac et al reported that atrial fibrillation catheter ablation results in an average of 76.9 kg of carbon dioxide (CO2)-equivalent (CO2e) emissions, amounting to 125 tonnes of CO2e released daily2. Unfortunately, no studies have evaluated the carbon footprint of coronary angiography procedures. This work aims to estimate the overall and detailed carbon footprint of a coronary angiography procedure, with the goal of raising awareness among healthcare professionals and industry partners to reduce the GHG emissions associated with these procedures.
To conduct this study, we exhaustively catalogued all the equipment and treatments used during a standardised diagnostic coronary angiography procedure at our centre. After this, we analysed each product, detailing its manufacturing material, country of origin, and primary packaging, while also measuring the weight of each item. We also considered the type of waste disposal (hazardous medical waste or general waste). The same process was applied to the treatments. Once the inventory was completed, all data were integrated into different calculators, which allowed us to establish the carbon footprint of each product. For medical devices, the calculator used was provided by the French Agency for Ecological Transition (ADEME) website. This calculator includes the entire lifecycle of a medical device, from the origin of all raw materials to the end-of-life of the device, including all transportation between different stages. We only considered the device and its primary packaging. For medications, the calculator used was provided by Ecovamed, which considers all stages of a medication’s lifecycle (active ingredient, primary and secondary packaging, and end of life). The emission factor of the active ingredient was calculated based on the price of the active ingredient per kilogram, which was then multiplied by an economic emission factor depending on the country of production (EXIOBASE).
The total carbon footprint associated with the products used during a diagnostic coronary angiography procedure amounts to 8 kg of CO2e. The total carbon waste for the treatment process, which includes the disposal and management of used materials, contributes an additional 4.48 kg of CO2e (~35%) (Supplementary Table 1). Energy consumption during a single procedure is estimated at 1.3 kWh, which corresponds to approximately 0.078 kg of CO2e in France, where electricity generation is largely based on nuclear energy. Each intervention generates 2.869 kg of waste (621 g of packaging and 2,248 g of medical devices). An analysis of each procedural category reveals that most emissions arise from single-use consumables (31%) and surgical drapes/covers (40%), while medications, disinfection, and energy consumption play a comparatively smaller role (Table 1).
The total carbon impact of a coronary angiography procedure is estimated to be 12.56 kg of CO2e. This highlights the significant environmental impact of such routine medical practices and underscores the importance of considering sustainability in healthcare procedures3. One area for improvement is the composition of the angiography kit provided. It would be beneficial to review the kit’s contents to eliminate surplus devices that do not add value to the procedure but contribute significantly to the carbon footprint. Regarding iodine, using larger-volume vials that can be shared among multiple patients would not only reduce the carbon footprint but also provide an economic benefit to healthcare facilities. Attention must be given to the end-of-life management of all medications and medical devices. Establishing recycling pathways and collaborating with specialised waste management companies could significantly improve the environmental footprint. In addition to material and waste reduction, emerging strategies such as remote diagnostic approaches may further reduce the carbon footprint of cardiovascular procedures and warrant future investigation. Finally, regulatory and institutional frameworks – such as green procurement policies, sustainability-linked accreditation criteria, and reimbursement incentives – could play a pivotal role in encouraging hospitals to adopt low-carbon practices in procedural care.
This study presents some limitations. The calculations do not take into account the exact formulation or manufacturing processes for the medications, including factors such as yield or energy consumption in the production facilities. These data are not provided by pharmaceutical laboratories, making it impossible to incorporate them into the analysis. Similarly, for medical devices, the manufacturing process is not considered, as these details are subject to industrial confidentiality and are therefore unavailable for inclusion in the calculation. Some data were not available or not shared by the manufacturers. We chose not to include emissions from transportation and broader hospital logistics due to the significant variability of these factors depending on patient origin, staff travel modes, and institutional supply chains, which are often difficult to generalise across settings
The carbon footprint of a diagnostic coronary angiography procedure is estimated at 12.56 kg of CO2e. This value is derived from various sources, including the use of medical materials, energy consumption and waste management. Several areas for improvement are identified, which could significantly reduce the carbon footprint of such cardiac procedures.
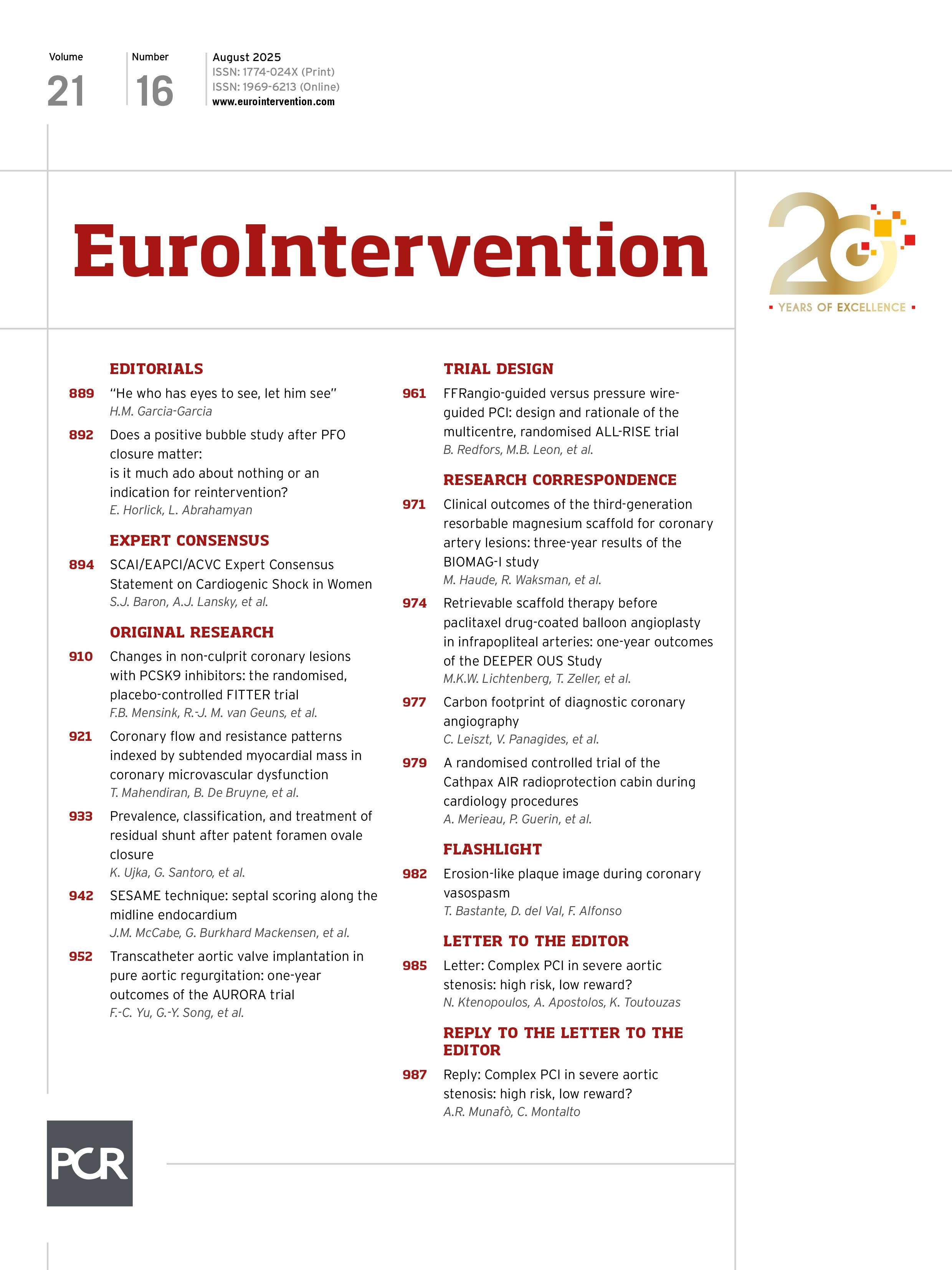
Table 1. Carbon footprint summary by procedural category.
| Category | Total carbon footprint (kg of CO2e) |
Waste management carbon footprint (kg of CO2e) |
% of total | Key reduction opportunity | |
|---|---|---|---|---|---|
| Medications & anaesthesia | 3.10 | 0.03 | ~25% | Simplify agents | Policy, accreditation standards, and financial incentives |
| Consumables/tools | 3.93 | 1.44 | ~31% | Switch to reusables or low-impact materials | |
| Disinfection | 0.41 | 0.17 | ~3.3% | Use refillable packaging, low-impact agents | |
| Drapes & covers | 5.04 | 2.84 | ~40% | Reduce drape use; bundle smarter packs | |
| Facility energy consumption | 0.078 | ~0.6% | Energy efficient devices/sustainable energy management/reduce procedure duration | ||
| Total | 12.56 | 4.48 | |||
Conflict of interest statement
V. Panagides has received institutional research grants from Medtronic, Boston Scientific, and MicroPort. The other authors have no conflict of interest.
Supplementary data
To read the full content of this article, please download the PDF.