Cory:
Unlock Your AI Assistant Now!
A 58-year-old male with hypertension, diabetes mellitus, and a history of smoking was admitted following a four-week history of oppressive chest pain at rest, with episodes lasting up to 20 minutes. His electrocardiogram and serial cardiac biomarkers were within normal limits. However, transthoracic echocardiography revealed hypokinesia in the basal septal and inferior wall regions. Coronary angiography showed mild atheromatosis in the left coronary artery without significant lesions. The right coronary artery (RCA) (Figure 1A, Moving image 1) demonstrated mild irregularities, along with a moderate lesion in the distal segment. Optical coherence tomography (OCT) revealed a fibrolipidic plaque without evidence of rupture or thrombus formation but with macrophage infiltration and images suggestive of layered plaque (Figure 1B, Figure 1C, Moving image 1). A vasospasm test with acetylcholine was subsequently performed. Following the administration of 20 μg of intracoronary acetylcholine, the patient experienced angina with ST-segment elevation, accompanied by the development of a significant stenosis in the distal RCA and an intermediate stenosis in the proximal segment (Figure 1D, Moving image 2). OCT of the proximal RCA during vasospasm confirmed a reduced intraluminal area and revealed an irregular endothelial surface with dorsal shadowing that was suggestive of thrombus, resembling the appearance of plaque erosion (Figure 1E, Figure 1F). Symptoms and ST-segment changes resolved completely after intracoronary nitroglycerine administration. A repeat coronary angiogram and OCT evaluation showed findings identical to the baseline (Moving image 3). The patient was treated with aspirin, ticagrelor and calcium-channel blockers, with an uneventful clinical course.
The typical OCT findings during coronary vasospasm include medial thickening and a “bumping” appearance of the intimal layer caused by muscular contraction of the media1. Intracoronary thrombus is a relatively common finding when evaluating coronary vasospasm sites with OCT2. Furthermore, laminar thrombus layered on the intima has been described in cases of recurrent coronary vasospasm3 and is proposed as the mechanism underlying the higher frequency of layered healing plaques observed in coronary arteries with positive vasospasm tests4.
In this case, the findings can be explained by a combination of these phenomena: a pre-existing layered thrombus adherent to the intima, resulting from recurrent vasospasm episodes, that was then externally compressed by medial contraction during a subsequent vasospastic event. The most intriguing aspect is the erosion-like image observed on OCT, which was transient and resolved after nitroglycerine administration. To the best of our knowledge, this phenomenon has not been previously reported and could have significant implications for intracoronary imaging interpretation and diagnosis.
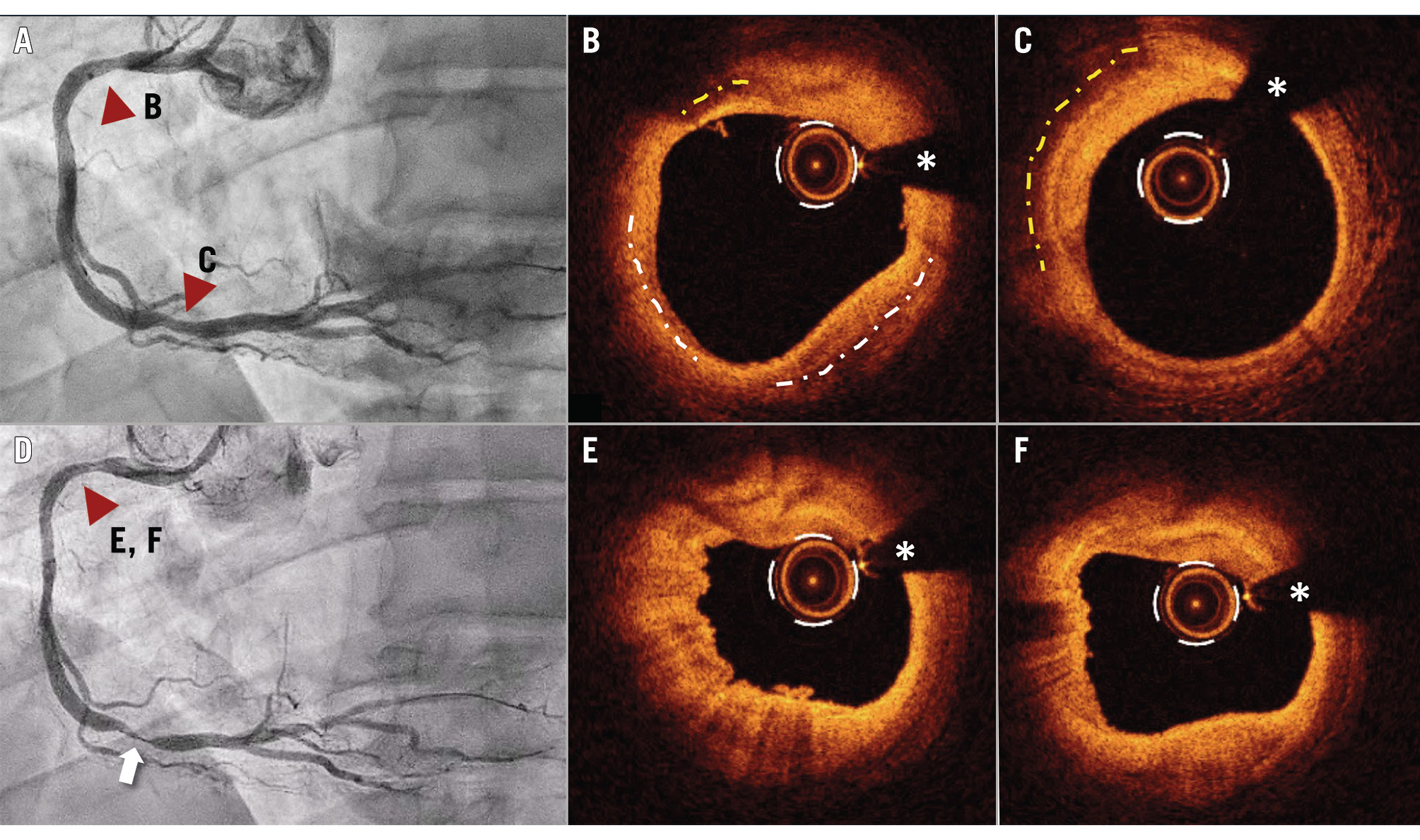
Figure 1. Coronary angiography and OCT images A) Coronary angiography of the baseline RCA shows no significant lesions in the proximal or distal segments (red arrowheads) B,C) OCT images of the proximal and distal segments demonstrate fibrolipidic plaques with macrophage infiltration (yellow dotted line) and no evidence of rupture or thrombus but findings suggestive of layered plaque (white dotted line). D) Coronary angiography after intracoronary acetylcholine administration reveals the development of a severe lesion in the distal segment (white arrow) and moderate obstruction in the proximal segment (red arrowhead). E,F) OCT images of the proximal segment show features resembling a typical erosion image during coronary vasospasm. White asterisks denote wire artefacts. OCT: optical coherence tomography; RCA: right coronary artery
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Baseline co-registration angio and optical coherence tomography images.
Moving image 2. After acetylcholine administration: coregistration angio and optical coherence tomography images.
Moving image 3. After nitroglycerine administration: coregistration angio and optical coherence tomography images.