Cory:
Unlock Your AI Assistant Now!
Several pharmacological agents can induce transient maximal hyperaemia, but most suffer from shortcomings that limit their clinical usage. Nicardipine, a dihydropyridine calcium channel blocker, has been proposed as an alternative coronary hyperaemic agent1. In the present study, we compared intracoronary (IC) nicardipine with IC papaverine for the measurement of fractional flow reserve (FFR) and pullback pressure gradient (PPG)2.
From February 2022 to March 2023, we prospectively enrolled 107 patients presenting with stable coronary artery disease and having an indication for invasive functional assessment. FFR and PPG measurements were performed consecutively with a standard pressure/temperature wire (PressureWire X [Abbott]) connected to CoroFlow software, version 3.5 (Coroventis Research). Following the induction of maximal hyperaemia by papaverine (12 mg for the left coronary artery [LCA] or 8 mg for the right coronary artery [RCA]), FFR, PPG and the duration of the hyperaemic plateau were assessed. Upon return to the resting state, measurements were repeated using IC nicardipine (400 μg for the LCA or 300 μg for the RCA) (Figure 1A).
FFR was measured in 108 vessels. The FFR values obtained with nicardipine and papaverine exhibited an excellent correlation (r=0.95, 95% confidence interval [CI]: 0.92 to 0.96; p<0.001) with a mean difference of 0.02 FFR units (limits of agreement [LOA]: –0.04 to 0.09). PPG was measured in 27 vessels and also exhibited a strong correlation (r=0.86, 95% CI: 0.71 to 0.93; p<0.001) with a mean difference of 0.01 PPG units (LOA: –0.14 to 0.17) (Figure 1B, Figure 1C). Of note, nicardipine induced a significantly longer hyperaemic plateau than papaverine (41.1±30.5 seconds vs 25.1±12.9 seconds; p=0.036). However, no clinically meaningful differences were observed between nicardipine and papaverine with regard to changes in blood pressure (decrease by 4.3% vs 3.7%) and heart rate (increase by 2.1% vs 3.3%). Finally, no complications were observed with either medication, including no arrhythmias nor conduction disturbances.
The present data indicate that, similar to papaverine, nicardipine induces maximal, steady-state hyperaemia, permitting the reliable measurement of both FFR and PPG, but with nicardipine offering a significantly longer hyperaemic plateau.
FFR and PPG are complementary metrics of epicardial resistance3. Whilst FFR can be considered a static measurement expressing the impact of total epicardial resistance proximal to the pressure sensor on coronary flow, PPG is obtained from a 20-30 second pullback manoeuvre and expresses the distribution of epicardial resistance along the length of the vessel. Crucially, both indices require maximal, steady-state hyperaemia for accurate measurements.
The most commonly used vasodilator of the resistive arteries is adenosine. However, due to its extremely short half-life, steady-state hyperaemia cannot be achieved with the IC bolus administration of adenosine. Instead, the intravenous infusion of adenosine can be used, although this is often hampered by large fluctuations in the Pd/Pa ratio, making PPG measurements less reliable. Papaverine is sometimes considered the “ideal coronary vasodilator”4, as it is easy to administer and induces 20-40 seconds of maximal hyperaemia5. However, it is not available in all countries and induces ventricular arrhythmias (QT prolongation and ventricular tachycardia) in approximately 1% of patients.
Compared to these hyperaemic agents, IC nicardipine is well tolerated1, is not associated with increased risk of malignant ventricular arrhythmias, and produces maximal hyperaemia which permits highly reliable FFR measurements. In addition, the duration of the hyperaemic plateau is ~40 seconds, allowing for the 20-30 second pullback manoeuvre to assess PPG immediately after FFR measurement. Additionally, nicardipine is widely available as it is frequently used to prevent radial arterial spasm. Since one vial of nicardipine contains 10 mg and only 6 mg are used for the “radial cocktail”, the same vial can also be used for coronary vasodilation.
In conclusion, FFR and PPG values obtained after nicardipine administration showed excellent agreement with those obtained using papaverine. Given its efficacy, long hyperaemic plateau, favourable safety profile, and very low cost, nicardipine can be considered the optimal vasodilator for the physiological assessment of coronary artery disease.
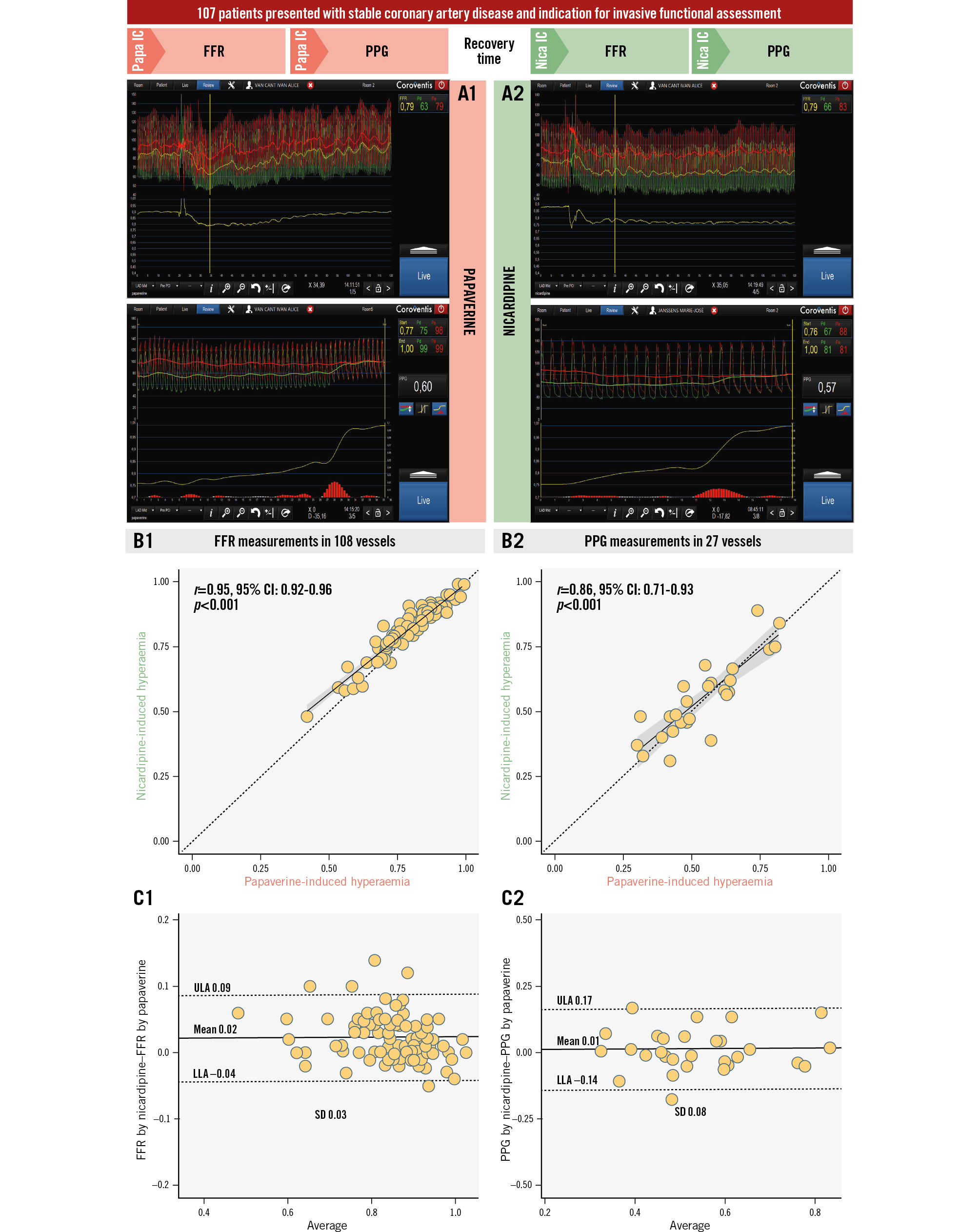
Figure 1. Agreement of FFR and PPG between the use of papaverine and nicardipine for inducing hyperaemia. A) Pressure tracings of FFR and PPG by papaverine (A1) and nicardipine (A2). B) Linear correlation of FFR (B1) and PPG (B2) by nicardipine and papaverine. C) Bland-Altman plots with the mean difference between FFR (C1) and PPG (C2) by papaverine and nicardipine. CI: confidence interval; FFR: fractional flow reserve; IC: intracoronary; Nica: nicardipine; LLA: lower limit of agreement; Papa: papaverine; PPG: pullback pressure gradient; SD: standard deviation; ULA: upper limit of agreement
Conflict of interest statement
M.M. Viscusi, A. Leone, D.T. Bertolone, and M. Belmonte are supported by a research grant from the CardioPaTh PhD programme, University of Naples Federico II, Naples, Italy. T. Mahendiran is supported by a research grant from the Swiss National Science Foundation (SNSF). B. De Bruyne reports receiving consultancy fees from Boston Scientific and Abbott; research grants from Coroventis Research, Pie Medical Imaging, CathWorks, Boston Scientific, Siemens Healthineers, HeartFlow, and Abbott; and owning equity in Siemens Healthineers, GE HealthCare, Philips, HeartFlow, Edwards Lifesciences, Bayer, Sanofi, and Celiad. C. Collet reports receiving research grants from Biosensors, Coroventis Research, Medis Medical Imaging, Pie Medical Imaging, CathWorks, Boston Scientific, Siemens Healthineers, HeartFlow, and Abbott; and consultancy fees from HeartFlow, OpSens, Abbott, and Philips Volcano. The other authors have no conflicts of interest to declare.

