Cory:
Unlock Your AI Assistant Now!
Coronary dominance patterns are associated with the prevalence and severity of obstructive coronary artery disease (CAD), as well as with prognosis following percutaneous coronary intervention (PCI)1. The left main (LM) coronary artery supplies 75% to 100% of the left ventricular myocardium, placing the left ventricle at considerable risk in cases of significant LM stenosis, particularly in patients with left dominance2. Studies have indicated that left coronary dominance is associated with worse outcomes compared to right dominance in CAD populations; however, these studies are either outdated or lack sufficient statistical power3. Current clinical guidelines for LM PCI focus on assessment of the lesion complexity and intravascular imaging guidance to optimise stent implantation4, without explicitly considering coronary dominance as an independent factor. This study aims to evaluate the influence of coronary dominance on long-term prognosis among a large cohort of LM PCI patients.
We analysed the relationship between coronary dominance and outcomes in consecutive patients with obstructive LM disease who underwent PCI between January 2004 and December 2016 at Fuwai Hospital, Beijing, China. The primary endpoint was 3-year major adverse cardiac events (MACE), a composite of cardiac death, myocardial infarction (MI), and target vessel revascularisation (TVR). Statistical analyses were carried out using SPSS Statistics, version 26.0 (IBM), and a two-sided p-value<0.05 was considered statistically significant.
Among 4,625 LM PCI patients, 166 (3.6%) had left dominance (Figure 1A). These patients had a lower prevalence of hypertension and prior PCI and a higher incidence of isolated LM lesions, a shorter lesion length, a larger reference vessel diameter, and lower SYNTAX scores (Supplementary Table 1, Supplementary Table 2). Multivariable Cox regression analyses demonstrated that age, left dominance, and incomplete revascularisation were associated with an increased risk of MACE, whereas successful lesion revascularisation was associated with a reduced risk. Additionally, left dominance and diabetes mellitus were linked to a higher risk of TVR, while successful lesion revascularisation was associated with a lower risk (Figure 1B). After propensity score matching, the 3-year incidence of MACE was higher in patients with left coronary dominance compared to those without (adjusted hazard ratio [HR] 1.73; 95% confidence interval [CI]: 1.01-2.95; p=0.04), primarily driven by a higher rate of TVR (adjusted HR 3.25; 95% CI: 1.53-6.90; p=0.001) (Figure 1C). The rates of all-cause death, cardiac death, and MI were comparable between the two groups (Supplementary Table 3). After accounting for the competing risk of non-cardiac death, the risk of MACE in the left dominance group remained higher than that in the non-left dominance group, but the difference did not reach statistical significance (Supplementary Figure 1). According to the subgroup analysis of MACE, the higher risk associated with left dominance was more significant among patients with LM bifurcation lesions and those with a residual SYNTAX score>0 (Figure 1D).
Our findings demonstrate that (1) the proportion of left dominance among patients undergoing LM PCI is low, and these patients generally present with lower anatomical complexity; (2) left dominance in LM PCI patients is associated with a higher risk of long-term adverse events – particularly TVR – compared to non-left dominance patients; and (3) this increased risk may be more pronounced in patients with higher lesion complexity or incomplete revascularisation.
In this study, the prevalence of left dominance among patients undergoing LM PCI was slightly lower than the previously reported 8% to 12% in CAD patients undergoing coronary angiography5. Additionally, patients with left dominance in the present LM PCI cohort demonstrated less complex demographic and anatomical characteristics compared with non-left dominance patients. This observation likely reflects the influence of patient selection in real-world clinical practices. Given the extensive myocardial territory supplied by the LM artery in left-dominant patients, interventional cardiologists tend to avoid PCI in patients with more complex anatomy within this high-risk group.
According to this observational study, the data highlight two critical aspects: first, compared with non-left-dominant patients, those with left dominance exhibited a greater need for sustained blood flow restoration and experienced a higher rate of repeat revascularisation; and second, the risk of acute ischaemic damage was comparable between the two groups once adequate blood flow was restored. Notably, the risk in left-dominant patients was not significant among those with lower anatomical complexity, such as low SYNTAX scores or absence of LM bifurcation. Moreover, achieving complete revascularisation is particularly important, as the relatively small size and limited perfusion capacity of the right coronary artery make the maintenance of a non-stenotic left coronary artery essential. In summary, careful patient selection, optimal treatment strategies, and the achievement of satisfactory acute outcomes are crucial for effective PCI management in this population.
This study has several limitations. First, as a retrospective, single-centre analysis including only Chinese patients, it is susceptible to selection bias. Second, intravascular imaging was not mandatory during the study period, leading to limited utilisation, which might have influenced long-term outcomes. Third, variations in operator experience and technique had the potential to impact outcomes. Future large-scale, prospective studies are needed to further elucidate the influence of coronary artery dominance on the long-term prognosis of LM patients.
In this large-scale retrospective study, LM patients with left dominance undergoing PCI were associated with a significantly higher risk of long-term adverse events, particularly for TVR. Among patients with a higher lesion complexity and incomplete revascularisation, this risk may be further increased.
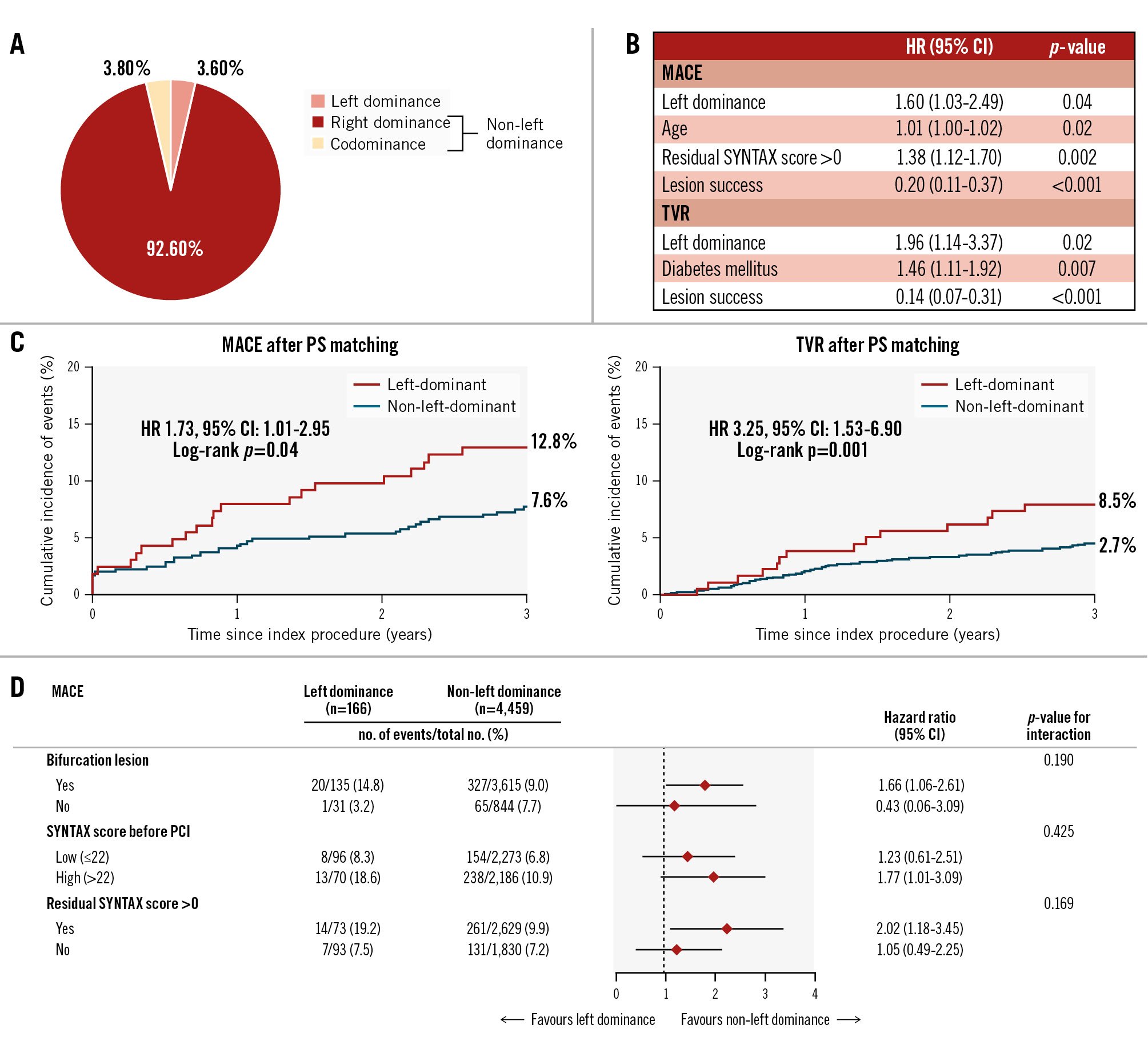
Figure 1. Coronary dominance distribution and clinical outcomes in left main patients. A) Coronary dominance distribution; (B) multivariable Cox regression models for MACE and TVR; (C) propensity score matching-adjusted Kaplan-Meier cumulative event curves for MACE and TVR; (D) subgroup analyses of 3-year MACE. MACE was defined as a composite of cardiac death, MI, and TVR. Propensity score matching variables: age, sex, hypertension, hyperlipidaemia, diabetes mellitus, family history of CAD, creatinine clearance rate before PCI, prior PCI, prior MI, ACS, LVEF, isolated left main, LM lesion length, residual SYNTAX score. ACS: acute coronary syndrome; CAD: coronary artery disease; CI: confidence interval; HR: hazard ratio; IVUS: intravascular ultrasound; LM: left main; LVEF: left ventricular ejection fraction; MACE: major adverse cardiac events; MI: myocardial infarction; PCI: percutaneous coronary intervention; PS: propensity score; TVR: target vessel revascularisation
Acknowledgements
The authors thank the staff in the Interventional Cardiovascular Imaging Core Laboratory, the National Centre for Cardiovascular Diseases, and Fuwai Hospital for their research contributions.
Funding
The present study was supported by research grants from the National High Level Hospital Clinical Research Funding (2022-GSP-GG-20, 2023-GSP-GG-3), the Capital’s Funds for Health Improvement and Research (2022-2-4033), the Chinese Academy of Medical Sciences (No. 2022-I2M-C&T-A-009), and the Non-communicable Chronic Diseases National Science and Technology Major Project (Grant Number: 2023ZD0504003).
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.