An 80-year-old patient with a history of transcatheter aortic valve implantation (TAVI) using a self-expanding valve, ACURATE neo2 M (Boston Scientific), 29 days earlier, presented to the emergency department with lateral ST-segment elevation myocardial infarction (STEMI). It is noteworthy that the coronary angiography performed as part of the pre-TAVI work-up showed no significant stenosis (Moving image 1), and the pre-TAVI CT analysis (Figure 1A-Figure 1B-Figure 1C-Figure 1D) revealed a virtual transcatheter heart valve (THV)-to-left coronary ostial distance of 5.8 mm (Figure 1D), indicating a low risk of coronary obstruction. Additionally, aortography performed after TAVI demonstrated the absence of any coronary obstruction (Moving image 2).
Urgent coronary angiography revealed an acute occlusion at the level of the proximal left circumflex artery (Figure 1E, Moving image 3). The door-to-wire time was 23 minutes. Thrombectomy with the Indigo System CAT RX catheter (Penumbra) was performed with two aspiration passages across the occlusion (Moving image 4), resulting in the immediate restoration of a distal Thrombolysis in Myocardial Infarction grade 3 flow without any residual stenosis (Figure 1F, Moving image 5). The patient became symptom-free immediately, with complete ST-segment elevation regression, without the need for stent placement.
The extracted material, on macroscopic analysis, consisted of a 2.5x1.6 mm mass that was irregular in shape with a rough texture and a nodular appearance. The surface of the embolus was predominantly white, reflecting its high calcium content (Figure 1G). Histopathological examination confirmed the diagnosis of a calcified embolus, including fibres of collagen, compatible with a calcified embolus originating from the native aortic valve (Figure 1H-Figure 1I).
To date, this is the first case confirmed by histopathological examination of a tardive coronary embolisation occurring more than 20 days after TAVI. Most cases of acute myocardial infarction post-TAVI are related to mechanical obstruction of the coronary ostia during the procedure1. Coronary embolisation after TAVI is rare, with most cases occurring within the first 60 minutes1. The available data do not clearly demonstrate whether certain types of TAVI valves are more associated with this rare complication1. In our case, the STEMI presentation was highly suggestive of a proximal complete coronary occlusion, but coronary embolisation may remain underdiagnosed and be involved in post-TAVI myocardial injury2.
According to the European Society of Cardiology Guidelines for the management of acute coronary syndromes, thrombus aspiration should not be performed routinely, only in selected cases3. The Indigo System CAT RX catheter is a latest-generation device designed to provide higher and more consistent aspiration power4. In most reported cases, post-TAVI coronary embolisation was managed by coronary stenting without associated thrombectomy1. This case highlights that in instances where STEMI is suspected to have a different aetiology – such as type 2 myocardial infarction clearly related to coronary embolisation – thrombectomy may be considered an effective strategy to retrieve large, highly calcified emboli, restore coronary flow, and avoid unnecessary stenting. In our case, single antiplatelet therapy with aspirin 80 mg was maintained. A previously reported case also illustrates that the off-label use of a stent retriever system, such as the enVast system (Vesalio), is another option to consider in the management of post-TAVI coronary embolisation5.
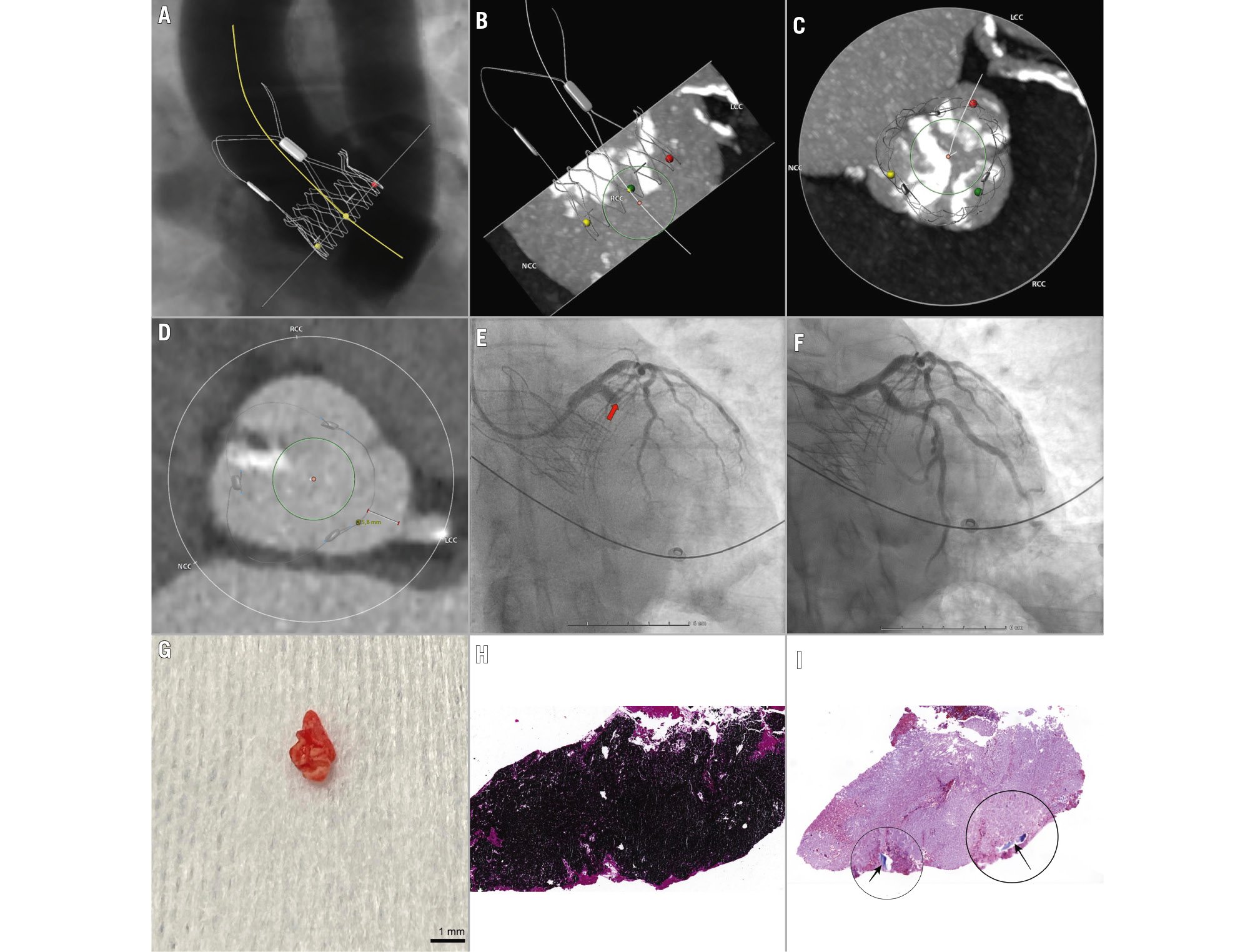
Figure 1. Late coronary embolisation after transcatheter aortic valve implantation: an imaging and pathological overview. A) The 3D virtual placement of the transcatheter aortic valve within the aortic root highlights the spatial relationship with the NCC (yellow marker), LCC (red marker), and RCC (green marker), as well as with the right and left coronary ostia. B) CT analysis with the 3D virtual valve placement. Severe calcifications are observed in the RCC. C) A different angle view, showing the alignment of the valve with the three cusps. D) Measurement of the virtual THV-to-left coronary ostial distance: 5.8 mm. E) Coronary angiography revealing an acute occlusion in the proximal LCx (red arrow). F) Restoration of distal flow in the LCx following thromboaspiration. G) Image of the extracted embolic material. H) Pathological examination stained with von Kossa, revealing large dark regions corresponding to areas of calcification. I) Pathological examination stained with Masson’s trichrome, showing a large purple calcium mass and two highlighted areas (black circles) of blue-coloured regions indicating collagen fibres (black arrows). 3D: three-dimensional; CT: computed tomography; LCC: left coronary cusp; LCx: left circumflex artery; NCC: non-coronary cusp; RCC: right coronary cusp; THV: transcatheter heart valve
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Diagnostic coronary angiography performed pre-TAVI showing a proximal left circumflex artery without stenosis.
Moving image 2. Aortography performed pre- and posttranscatheter aortic valve implantation demonstrated the absence of coronary obstruction.
Moving image 3. Urgent coronary angiography revealed an acute occlusion of the proximal left circumflex artery.
Moving image 4. Passing the Indigo System CAT RX catheter at the level of the proximal left circumflex artery.
Moving image 5. Complete restoration of distal TIMI 3 flow in the left circumflex artery.