Cory:
Unlock Your AI Assistant Now!
Coronary stents have revolutionised the treatment of coronary artery disease through three major technological advancements, each addressing a critical challenge. Initially, early iterations focused on improving safety by preventing abrupt vessel closure and reducing the need for emergency surgery. Subsequently, the emphasis shifted to improving efficacy by mitigating restenosis. Finally, efforts centred on optimising long-term safety, particularly by reducing the risk of stent thrombosis. Unlike the rapid evolution of transcatheter heart valves, which progressed at an unprecedented pace, advancements in coronary stent technology unfolded over three decades. This prolonged development, marked by inevitable setbacks, may explain why the impact of drug-eluting stents (DES) appears to have been underappreciated within interventional cardiology. Now, a decade after European guidelines endorsed new-generation DES for all patients undergoing percutaneous coronary intervention (PCI), regardless of clinical context or lesion complexity, the landscape continues to evolve. The new-generation DES family has branched into three major categories: permanent (or durable)-polymer DES, biodegradable-polymer DES, and polymer-free DES. The latter two emerged in response to concerns about permanent polymers, particularly their potential to induce local vascular inflammation. While these complications were documented with early-generation devices, there is no definitive evidence that the more biocompatible permanent polymers used in new-generation DES share similar risks. Biodegradable-polymer DES have been designed to facilitate temporary drug delivery, with the polymer degrading into water and carbon dioxide within months. In contrast, polymer-free DES eliminate polymers entirely, relying on alternative drug-release mechanisms. These refinements reflect an ongoing pursuit of the ideal stent – one that maximises efficacy while minimising long-term vascular complications.
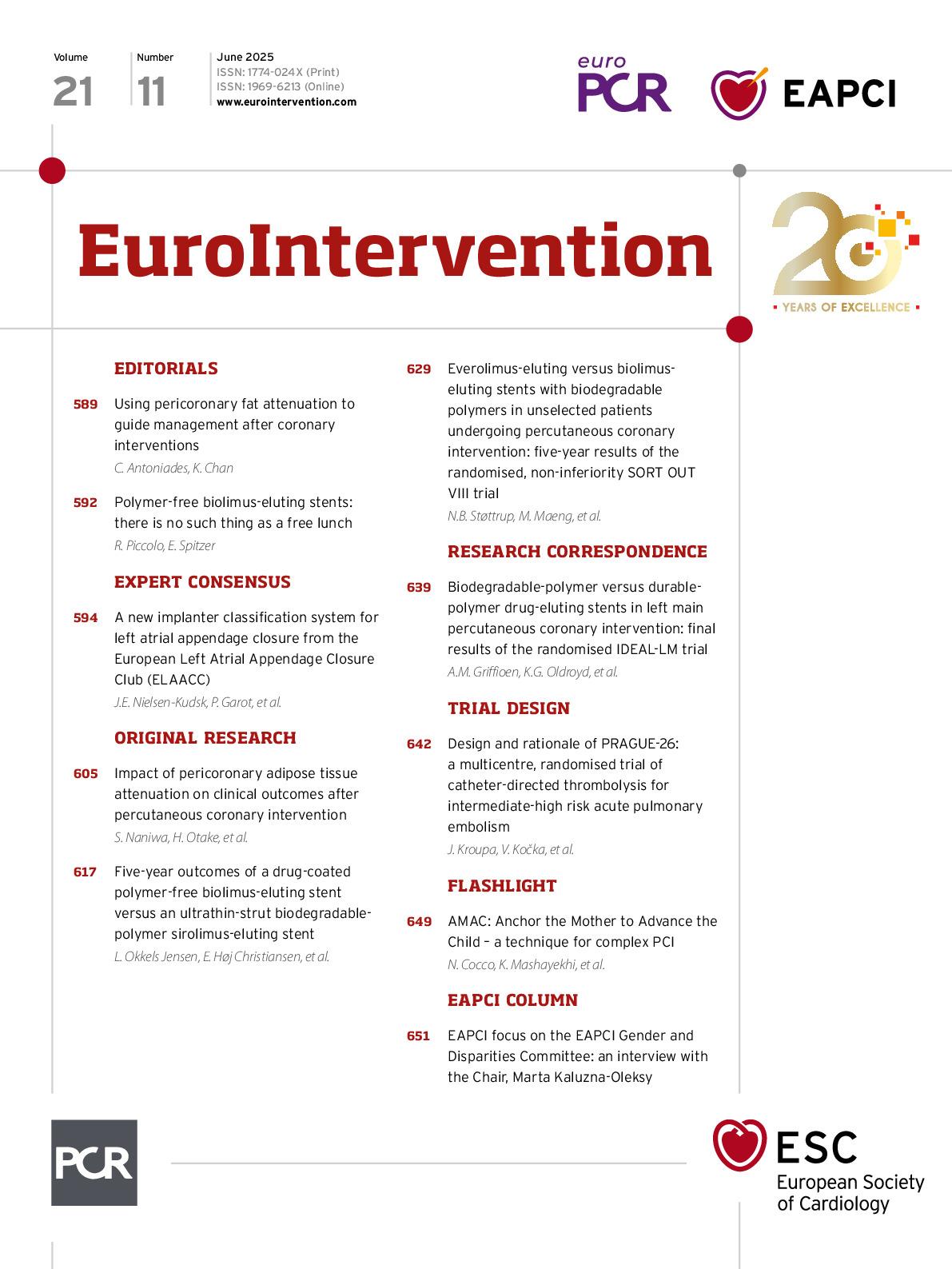
In this issue of EuroIntervention, Okkels Jensen and colleagues report the 5-year follow-up of the SORT OUT IX randomised trial, which compared the polymer-free, biolimus-eluting stent (BioFreedom [Biosensors]) with the biodegradable-polymer, sirolimus-eluting stent (Orsiro [Biotronik]) among 3,151 all-comer patients undergoing PCI1. The primary endpoint of target lesion failure − a composite of cardiac death, target lesion myocardial infarction, or target lesion revascularisation − occurred in 14.1% of patients randomised to BioFreedom and in 12.0% of patients randomised to Orsiro. In the landmark analysis at 1-year follow-up, most of the differences in clinical outcomes occurred between 0 and 1 year, whereas risk estimates for both safety and efficacy outcomes were somewhat similar between 1 and 5 years.
How should we interpret the findings of the SORT OUT IX trial? It is important to first analyse the data in the context of the 1-year follow-up. The study was designed with a non-inferiority hypothesis, which was rejected because the upper limit of the 1-sided 95% confidence interval for the absolute risk difference was 2.50% – a threshold higher than the predetermined non-inferiority margin of 2.1%. Although the non-inferiority hypothesis cannot be formally tested at 5-year follow-up, the 95% confidence interval (0.97-1.44) around the point estimate for the primary outcome (rate ratio 1.19) indicates that BioFreedom stents were unlikely to be beneficial. While there were clearly no differences in either cardiac death or target lesion myocardial infarction, the risk of target lesion revascularisation was increased by more than 50% in patients randomised to BioFreedom. This latter effect was mostly observed during the first year after stenting (rate ratio 2.76), with no significant difference between the 1- and 5-year follow-up (rate ratio 1.13). These results are consistent with the 2-year results of the ONYX trial, in which there was an excess of target vessel revascularisations in patients randomised to BioFreedom in comparison to permanent-polymer zotarolimus-eluting stents2. Thus, while the SORT OUT IX trial confirms the safety of BioFreedom (i.e., comparable results on cardiac death, target vessel myocardial infarction, and definite stent thrombosis), its efficacy profile, with a higher risk of repeated revascularisation procedures during the first year, emerges as a potential drawback of this technology. Because approximately 90% of the antiproliferative drug is eluted during the first 48 hours after implantation, it is possible that such overly rapid release results in a suboptimal suppression of neointimal hyperplasia. It is worth noting that a similar amount of the drug (~80-90%) is typically released in about 30 days with other new-generation DES. Although the stainless-steel platform used in the BioFreedom stent has been questioned for potentially increasing neointimal proliferation, a randomised trial comparing the same BioFreedom stent to a stainless steel (112-120 μm) or a cobalt-chromium platform (84-88 μm) revealed a similar degree of late lumen loss for both devices3. As a final note, a class effect for polymer-free DES should not be assumed. In the PARTHENOPE trial, a polymer-free amphilimus-eluting stent demonstrated similar efficacy to a biodegradable-polymer everolimus-eluting stent4. Additionally, the ISAR-TEST-5 trial showed the long-term efficacy of a probucol-based, polymer-free sirolimus-eluting stent at 10-year follow-up5.
In conclusion, we should be grateful to the SORT-OUT investigators for providing continuous evidence on coronary stents over the past two decades. Their work has, for the first time, provided a comprehensive, long-term comparison of polymer-free versus biodegradable-polymer DES.
Conflict of interest statement
E. Spitzer declares institutional contracts/grants for which he receives no direct compensation from Abbott, Biosensors Europe SA, Boston Scientific, Edwards Lifesciences, Medtronic, Mixin Medtech (Suzhou) Co., Ltd., Shanghai Microport Medical Co., Ltd., NVT GmbH, Philips Healthcare, Pie Medical Imaging, Shanghai Shenqi Medical Technologies Co., Ltd., and Siemens Healthineers; he also declares being a board member of Cardialysis, European Cardiovascular Research Institute, EU-MDR Cardiovascular Collaboratory, and Academic Research Consortium. R. Piccolo has no conflicts of interest to declare.