Cory:
Unlock Your AI Assistant Now!
Abstract
Editorial note: On 28 May 2025, the manufacturer announced the global discontinuation of sales of its ACURATE neo2 and ACURATE Prime aortic valve systems. The following correspondence, submitted and accepted prior to the market withdrawal, discusses clinical experience with this device. Though no longer relevant for current practice, the Editorial Board believes it is important to document these findings in the interest of transparency and completeness of the scientific record. Accordingly, we are publishing this work as a Research Correspondence, with acknowledgement of the device’s discontinued status.
As transcatheter aortic valve implantation (TAVI) is now performed in patients with longer life expectancy, the need for a second aortic valve procedure is expected to increase. Balloon-expandable short-frame SAPIEN 3/Ultra transcatheter heart valves (THVs; Edwards Lifesciences) are frequently selected for younger patients undergoing TAVI due to their lower likelihood of impairing coronary access and a design that may facilitate future redo-TAVI procedures1. Consequently, a consistent proportion of reinterventions is anticipated to involve degenerated short-frame THVs. While redo-TAVI with a same-sized SAPIEN 3/Ultra THV is usually feasible, recent bench studies indicate that the ACURATE platform (neo2/Prime [Boston Scientific]) might offer more favourable haemodynamic performance and minimal pinwheeling, particularly in smaller valve sizes2. Furthermore, the large-cell design of the ACURATE THV may more easily facilitate future coronary access compared to other supra-annular closed-cell THVs3. This paper is the first to provide practical guidance for performing redo-TAVI with the ACURATE THV in failing short-frame THVs, based on initial real-world clinical experience.
Preprocedural planning
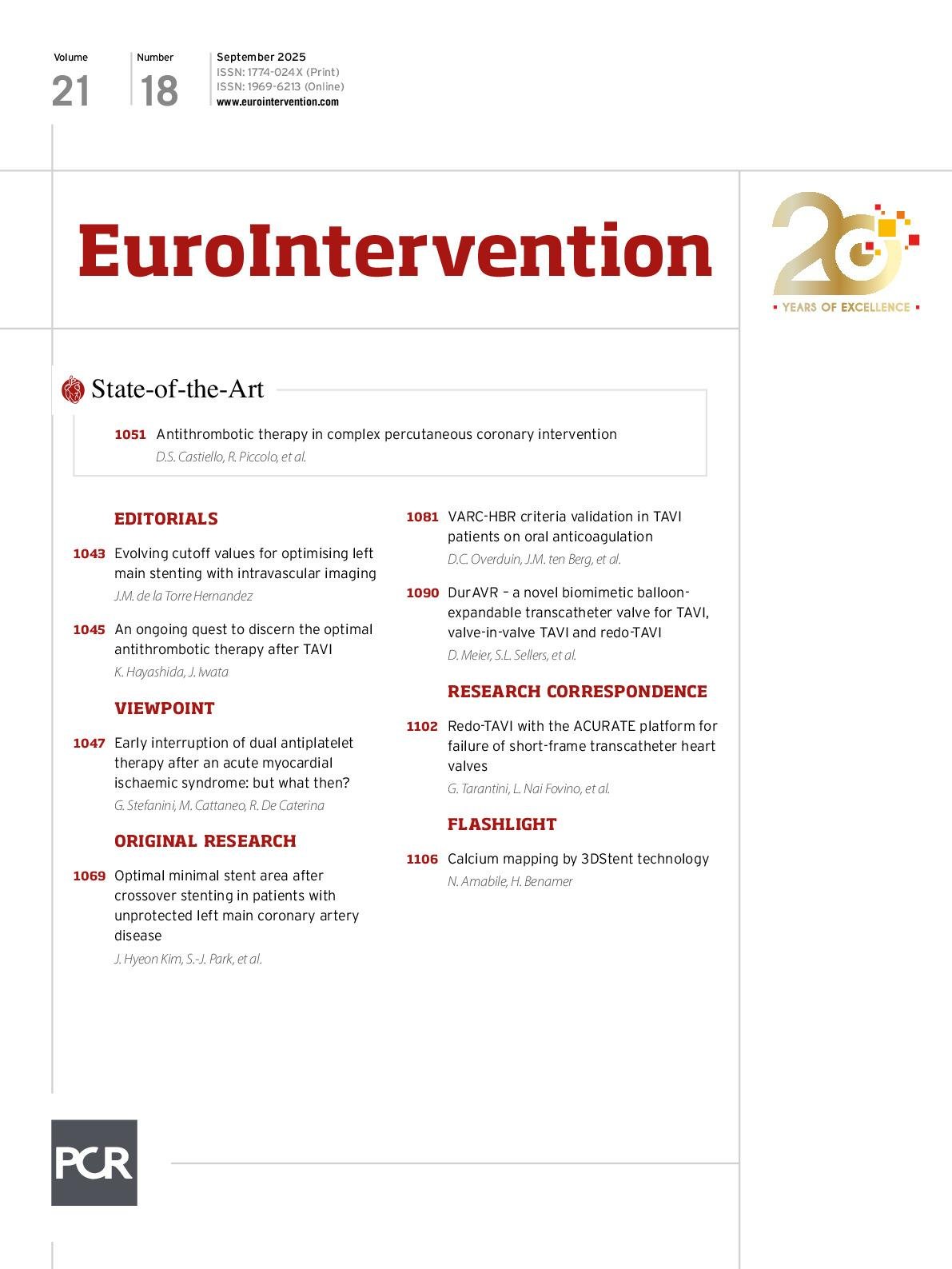
As with all redo-TAVI cases, assessing neoskirt height, coronary ostia height, valve-to-coronary (VTC), and valve-to-aorta (VTA) distances is critical to evaluate the risk of coronary flow impairment and feasibility of the procedure4. In this particular configuration – placement of a tall-frame THV within a short-frame THV – the leaflets of the degenerated valve are anticipated to be completely displaced upward following deployment of the second valve. The latest ACURATE platforms feature an outer sealing skirt that extends to the lower edge of the upper crown that typically caps the native leaflets (14-17 mm from S to XL). These upper crowns are designed to prevent ventricular movement and create space for coronary access, projecting 2.5 mm beyond the nominal valve size at 3 locations in between the commissures. Complete ACURATE THV expansion requires positioning the upper crown above the SAPIEN THV’s outflow, resulting in a neoskirt higher than the stent frame of the failing valve. Consequently, preprocedural computed tomography (CT) should measure the VTC and VTA distances relative to the predicted neoskirt height, considering the risk of sinus sequestration (Figure 1A). In general, when the coronary ostia are located below the level of the neoskirt, a VTC or VTA distance of less than 4 mm should prompt consideration of coronary protection strategies, including the potential use of chimney stenting. Even if a higher neoskirt does not impair coronary perfusion, upper crowns in smaller aortic root anatomies could complicate selective coronary engagement (Figure 1B).
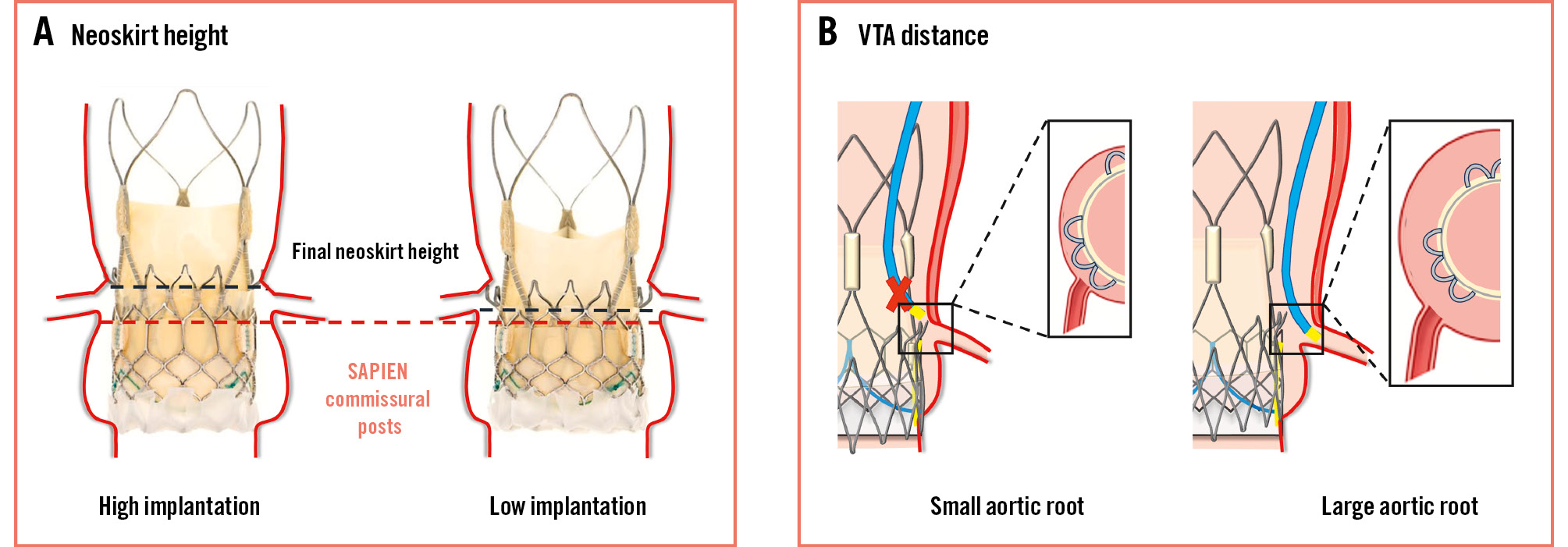
Figure 1. Preprocedural assessment of the risk of coronary obstruction and coronary access impairment with ACURATE-in-SAPIEN redo-TAVI. A) Neoskirt height and risk of sinus sequestration with low versus high ACURATE THV implantation. B) Possible coronary access impairment despite preserved coronary artery perfusion in patients with small versus large aortic root anatomies. TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve; VTA: valve-to-aorta
Sizing and positioning
Based on bench data, ACURATE neo2/Prime sizing recommendations for the treatment of SAPIEN 3/Ultra failure are reported in Supplementary Table 1. When the original THV is appropriately sized and expanded, haemodynamic performance after redo-TAVI is minimally influenced by the native annular dimensions2. However, the expansion of the SAPIEN THV should also be carefully assessed on CT imaging, as the measured true internal diameter and area directly impact the sizing of the ACURATE THV.
As previously explained, to ensure full expansion of the ACURATE THV, its upper crown must be positioned above the SAPIEN THV outflow. Higher implantation (upper crowns approximately 3 mm above the SAPIEN 3 stent frame) has demonstrated slightly lower (<3 mmHg) anterograde gradients in vitro, especially in the 20 mm and 23 mm short-frame THVs2. The clinical impact of this haemodynamic variation requires further real-world studies. The potential benefits of a higher implantation must be weighed against the increased risk of sinus sequestration, especially in patients with a narrow sinotubular junction.
Procedural considerations
The first case series of redo-TAVI using the ACURATE platform in a short-frame THV is reported in Supplementary Figure 1-Supplementary Figure 2-Supplementary Figure 3-Supplementary Figure 4-Supplementary Figure 5-Supplementary Figure 6-Supplementary Figure 7. Based on this initial clinical experience, the key procedural recommendations include the following:
1) Predilatation: strongly consider predilatating the failed THV to ensure optimal ACURATE THV expansion, particularly when the failure mechanism is stenosis.
2) Commissural alignment: this should always be pursued to facilitate future coronary access. Notably, the cusp-overlap projection should be calculated based on the native aortic root CT scan (if available) or on the coronary position at the pre-redo-TAVI CT scan (i.e., “coronary overlap view”) (Figure 2A). Alignment of the failing short-frame valve is of little importance, given the futility of bioprosthetic or native aortic scallop intentional laceration to prevent iatrogenic coronary artery obstruction (BASILICA) during TAVI in this type of redo-TAVI combination. Implantation techniques to achieve commissural alignment should be performed as previously reported in TAVI for native aortic stenosis5.
3) Eliminating parallax: before deployment, ensure no parallax on the SAPIEN THV in both the 3-cusp and cusp-overlap views.
4) Deployment strategy: start ACURATE deployment (Figure 2B) only after confirming that the upper crown hooks will open just above the SAPIEN 3 outflow. Ignore the annular radiopaque marker and focus on the upper crown’s position relative to the SAPIEN frame. If the upper crown has been opened within the stent frame of the SAPIEN frame, it might be possible to reposition the upper crown above the outflow part by careful wire manipulation, especially if only one side of the upper crown is hooked inside the SAPIEN frame. Final positioning (low vs high implant) can be adapted once the opening of knob 1 has been completed, based on preprocedural considerations about sinotubular junction dimensions and the risk of coronary flow impairment. However, the last movement of the delivery catheter before opening knob 2 should always be forward.
5) Delivery system removal: centralise the system by retracting the wire loop to ensure safe removal.
6) Evaluate outcomes: always evaluate valve expansion at fluoroscopy (both in the 3-cusp and cusp-overlap views) and measure invasive gradients to verify haemodynamic results and decide on post-dilatation. Given the presence of the protruding upper crowns, the possible risk of aortic root injury with post-dilatation should always be considered, particularly in smaller aortic root anatomies (Supplementary Figure 8). The upper crown extends maximally 2.5 mm beyond the ACURATE valve waist in each sinus; there may be less protrusion if the degenerated SAPIEN leaflets are bulky/calcified and thus prevent the ACURATE frame fully extending to the edge of the SAPIEN valve.
Figure 2. Procedural considerations during ACURATE-in-SAPIEN redo-TAVI. A) Commissural alignment of the ACURATE THV. The cusp-overlap view should be calculated based on native aortic valve anatomy, disregarding the position of the SAPIEN THV commissural posts. B) Step-by-step deployment of an ACURATE neo2 valve in a degenerated SAPIEN 3 (left) and SAPIEN XT (right) THV. The operator needs to check that the upper crown is positioned above the short-frame THV outflow to ensure the complete expansion of the ACURATE THV. TAVI: transcatheter aortic valve implantation; THV: transcatheter heart valve
Conclusions
The use of supra-annular THVs with a large-cell design for failing short-frame THVs offers theoretical advantages in haemodynamic performance and future coronary access. Understanding the specific preprocedural and procedural considerations of this redo-TAVI combination is vital to mitigate risks and optimise outcomes. Our initial clinical experience underscores the necessity for larger studies to validate the safety and long-term effectiveness of this approach.
Conflict of interest statement
G. Tarantini reports honoraria for lectures/consulting from Medtronic, Edwards Lifesciences, Boston Scientific, Abbott, and SMT. W.-K. Kim reports personal fees from Abbott, Boston Scientific, Edwards Lifesciences, JenaValve, and Meril Life Sciences; and institutional fees from Boston Scientific. N. Mangner received research and an educational grant from Abiomed to his institution, outside the submitted work; an educational grant from Boston Scientific to his institution, outside the submitted work; received personal fees from Edwards Lifesciences, Medtronic, Biotronik, Novartis, Sanofi Genzyme, AstraZeneca, Pfizer, Daiichi Sankyo, Abbott, Abiomed, B. Braun, and Boston Scientific, outside the submitted work. R. Parma reports honoraria for lectures from Edwards Lifesciences. L. Nai Fovino reports honoraria for lectures/consulting from Edwards Lifesciences; and a research grant from Medtronic. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.