Cory:
Unlock Your AI Assistant Now!
In retrograde chronic total occlusion (CTO) percutaneous coronary intervention (PCI), when the retrograde microcatheter (MC) fails to traverse the occlusion, precluding conventional guidewire externalisation, tip-in techniques have emerged as effective bailout strategies1. In cases where even this approach fails – specifically when the anterograde MC can cannulate the retrograde guidewire but cannot advance through the occlusion – external cap crush or switching to a last-resort rotablation wire may be considered, despite the risk of losing the established guidewire connection. This approach relies on the likelihood that the rotablation guidewire will successfully navigate through the created microchannel, a difficult task in long occlusions.
We present the case of a 60-year-old male patient undergoing right coronary artery CTO PCI, where retrograde wire escalation and tip-in techniques were performed. However, both MCs became lodged at a significant distance from each other (Figure 1A, Supplementary Figure 1) (antegrade MC: Corsair Pro 135 mm [Asahi Intecc]; retrograde MC: Turnpike LP 150 mm, [Teleflex]); additionally, due to length constraints (having only 100 cm catheters), the retrograde MC end reached the Y-connector – precluding retrograde balloon inflation. Support had already been maximised with an Amplatz left (AL) 1.0 7 Fr guiding catheter (inside which we also trapped the retrograde guidewire with a balloon), leading us to suspect that MC fatigue might be contributing to the issue. Consequently, a second tip-in attempt was performed using a new Turnpike Spiral 135 mm MC (Teleflex); however, this MC also became stuck at the same location. The “facilitated tip-in technique” was also ineffective2. As a last resort, an antegrade 2.0 mm coronary balloon was advanced over a tipped-in retrograde guidewire3, encountering the same obstruction. With no other options available, the balloon was intentionally burst (“grenadoplasty”) in an attempt to modify the CTO calcium (Figure 1B). This manoeuvre proved effective, as a fourth tip-in allowed the same antegrade MC to traverse the occlusion, finally converting the procedure into a purely antegrade PCI. Intravascular ultrasound clearly demonstrated an intraplaque course of the guidewire and 360° circumferential calcium at the uncrossable segment (Moving image 1).
The antegrade tip-in balloon technique over the retrograde guidewire is a straightforward and feasible approach, easily reproducible on the outer curves of the antegrade guiding catheter. The technique offers a valuable, specific reinterpretation of the broader category of “portal” techniques1, as it enables angioplasty and “grenadoplasty” in challenging CTO lesions that are otherwise uncrossable, facilitating the subsequent readvancement of the antegrade MC and allowing for the continuation of the procedure. We acknowledge that intentional extraplaque tracking (using balloon-assisted subintimal entry [BASE], external cap crush, etc.) could have been a viable alternative to facilitate CTO crossing, given that the intraplaque position of the guidewire hindered successful passage in our case. To optimise procedural planning, the use of 90 cm guiding catheters and an antegrade guide extension should be standardised. Finally, caution should be exercised to avoid this technique in cases of extensive plaque tracking with knuckle wires, as it increases the risk of significant extraplaque barotrauma and perforation. The balloon size should be limited to 1.5 mm, or at most 2.0 mm, to minimise this risk.
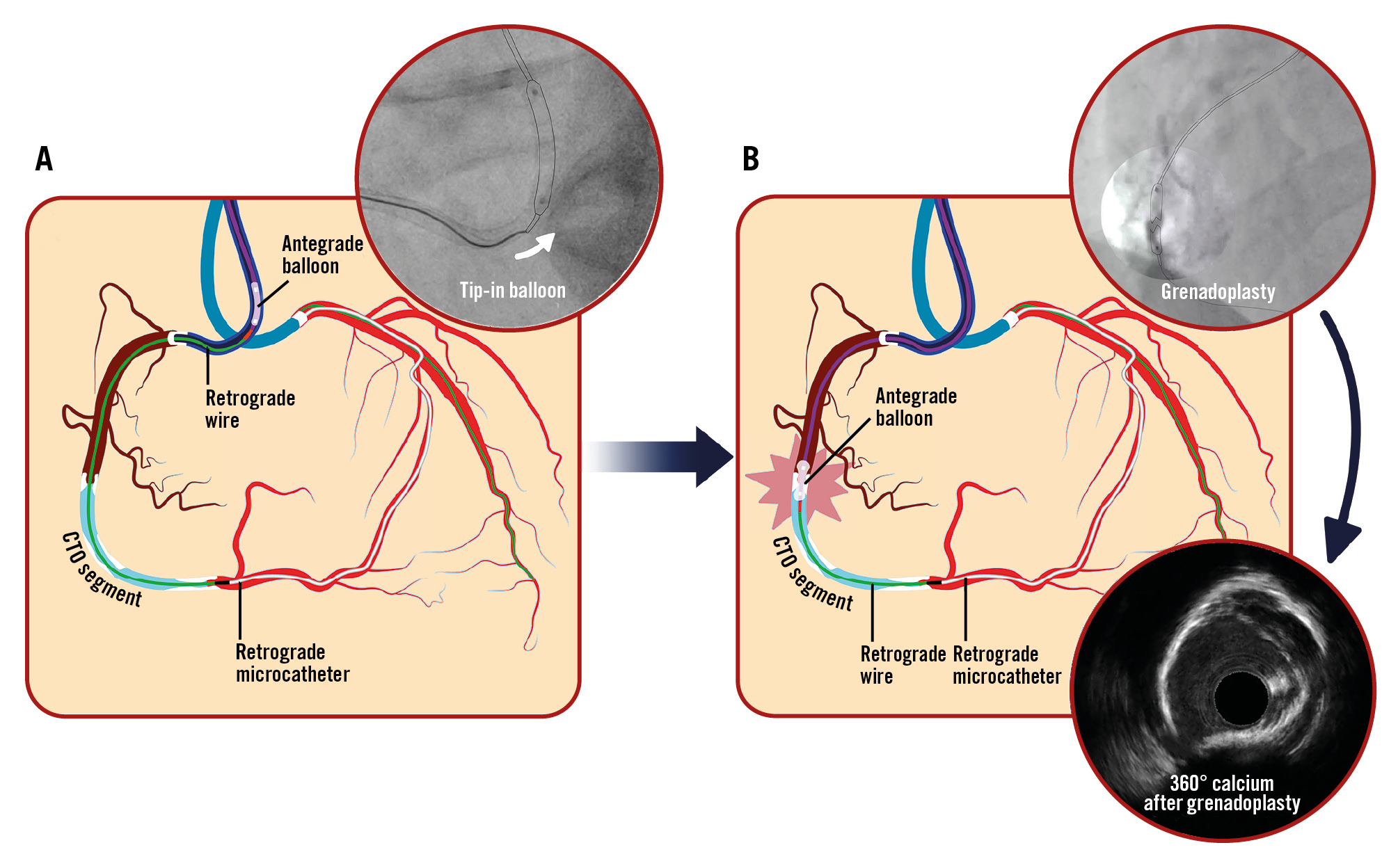
Figure 1. Tip-in balloon grenadoplasty: case illustration and technique overview. A) Tipping-in the retrograde wire inside the antegrade balloon. B) Balloon advacement and grenadoplasty. CTO: chronic total occlusion
Conflict of interest statement
The authors have no conflicts of interest to declare regarding the content herein.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Case step-by-step videos and description.