Cory:
Unlock Your AI Assistant Now!
Transfemoral access is the preferred choice for most transcatheter aortic valve implantation (TAVI) procedures. However, there are patient-specific femoral features that can limit its use. For this reason, alternative approaches, such as transcaval access, have been explored to overcome these limitations. In this procedure, an introducer is placed in the femoral vein and guided into the inferior vena cava (IVC). A fistula is then created between the IVC and the aorta using a guidewire-electrification technique. Finally, the fistula is closed with an Amplatzer occluder (Abbott). One factor that can make this approach difficult is the descending aorta calcium burden (since transcatheter electrosurgery techniques are more challenging through calcified areas and could increase the risk of vessel damage)1.
We treated a 78-year-old male with a history of chronic obstructive pulmonary disease (COPD), severe peripheral vasculopathy with bilateral bypasses in inferior extremities, previous myocardial infarction, and severe aortic stenosis with high operative risk and a challenging anatomy that hindered alternative access.
A preprocedural computed tomography (CT) scan showed diffuse and severely calcified atheromatosis in the descending aorta. Due to severe aortic wall calcifications and a narrow window without calcium (Figure 1, Supplementary Figure 1), the team foresaw a potentially unfeasible or dangerous entry into the aorta. To facilitate crossing, we decided to modify the classic transcaval crossing trajectory, from the descending aorta into the IVC, for an aorta-outward traversal through a less calcified aortic surface.
Intravascular ultrasound (IVUS) evaluation of the descending aorta calcification was carried out to visualise the path for and steer guidewire traversal (Figure 1, Moving image 1). After locating a less calcified target, simultaneous aortic and caval angiograms were acquired to correlate anatomical landmarks with the IVUS findings. Aortocaval traversal was made with an electrified 190 cm Gaia Second wire (ASAHI). After crossing, the wire was snared into the IVC, a FineCross microcatheter (Terumo) was advanced into the IVC and the Gaia Second wire exchanged for a 300 mm BMW wire (Abbott) (Supplementary Figure 2). Sequential dilations of the descending aortic wall were performed with semicompliant balloons, but due to incomplete expansion, we used a non-compliant balloon (3.0 mm OPN NC balloon [SIS Medical]) (Supplementary Figure 3). We crossed a 5 Fr 45 cm Flexor introducer sheath (COOK), with the balloon-assisted tracking technique, from the IVC into the aorta, followed by predilation with 4.0 mm and 5.0 mm balloons over a Lunderquist Extra-Stiff wire (COOK) in order to be able to cross a 14 Fr eSheath (Edwards Lifesciences) (Supplementary Figure 4). After the transcaval pathway was ready, a 27 mm Navitor valve (Abbott) was implanted (Supplementary Figure 5). For aortocaval closure, we used a 10 mm/8 mm Amplatzer Duct Occluder (Abbott) over an Agilis NxT Steerable Introducer (Abbott) (Supplementary Figure 6). Femoral vein access was closed with a figure-of-8 suture.
The transcaval approach is a good alternative when the gold-standard transfemoral access is not possible. In patients with complex anatomical features, such as a heavy calcium burden, that could preclude a transcaval path, a modification in the electrification trajectory of the classic technique can be feasible in selected patients when performed by experienced operators. Availability of a vascular access needs to be considered for bailout resolutions in case of vessel damage.
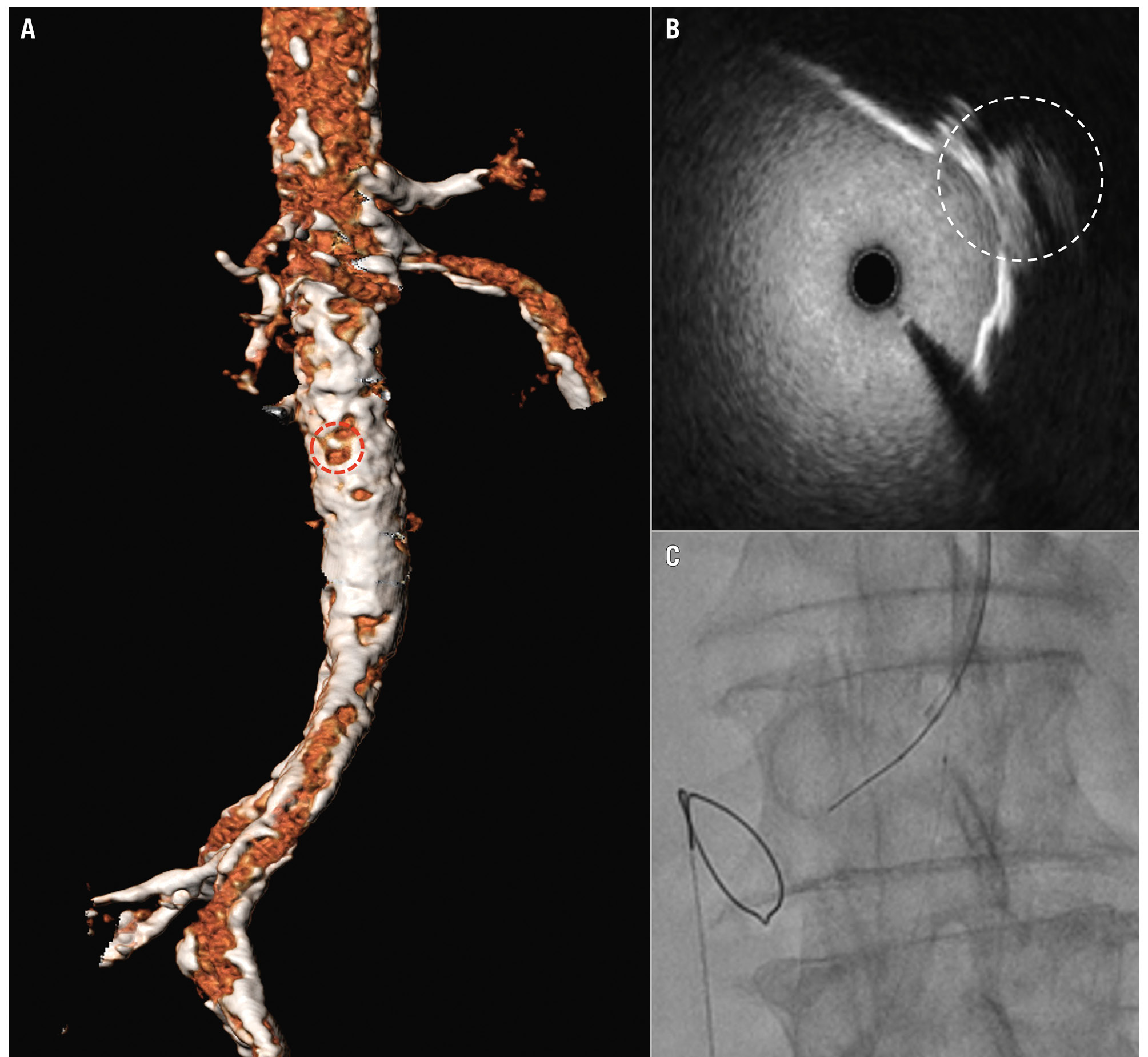
Figure 1. Heavily calcified descending aorta and iliac-femoral axis. Note the narrow, “less calcified” window (A, red dotted circle) corresponding to the IVUS image target (B, white dotted circle) used for aortocaval traversal (C) in this transcaval TAVI procedure. IVUS: intravascular ultrasound; TAVI: transcatheter aortic valve implantation
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. IVUS evaluation of descending aorta calcification: note the narrow, less calcified target for traversal (appearing as a dotted circle).

