Cory:
Unlock Your AI Assistant Now!
We describe a technique to facilitate transcaval (TC) transcatheter aortic valve implantation (TAVI) in a patient with an occluded right common iliac vein. We highlight the feasibility of a left-sided femoral venous approach and the technique employed to overcome the technical challenge encountered in achieving successful transcaval access.
An 86-year-old male with severe symptomatic aortic stenosis and severe peripheral arterial disease presented for elective TC TAVI. Transcaval access was preferred over transaxillary access to minimise the risk of stroke in a patient with significant atherosclerotic disease, given that this access site avoids instrumenting the head and neck vessels. A conventional transcaval approach via right common femoral venous (CFV) access (Figure 1A) was precluded by occlusion of the patient’s right common iliac vein (CIV), presumed secondary to a prior undiagnosed deep vein thrombosis (Figure 1B). An attempt was then made to achieve TC access from the left CFV access site rather than exploring percutaneous revascularisation of the right iliac venous occlusion, as we anticipated this would be a more challenging procedure. However, due to the angulation between the left CIV and the IVC (Figure 1C), we encountered two major technical issues that made TC access impossible using the conventional technique. First, the tip of the renal double curve and renal internal mammary guide catheters did not achieve a horizontal trajectory between the inferior vena cava (IVC) and the aorta (Ao). Second, neither catheter apposed the aortic facing wall of the IVC with sufficient force. Consequently, attempts to advance the electrified Astato wire (Asahi Intecc) resulted in a vertical rather than horizontal trajectory of the wire (Figure 1D, Figure 1E).
This technical challenge was overcome by using a coronary Amplatz left (AL) 0.75 guide catheter which was shortened to achieve the typical renal length (i.e., 65 cm) to facilitate conventional TC TAVI access (Figure 1F). The terminal 35 cm of the AL 0.75 guide catheter was cut off with a scalpel. The terminal 4 cm of a 5 Fr sheath (Cordis) was cut off and the dilator was reintroduced to the sheath. The dilator of the 5 Fr Cordis sheath was then advanced into the cut end of the AL 0.75 guide, and the 5 Fr Cordis sheath was advanced over the end of the AL 0.75 guide. The dilator was then removed (Figure 1G). The AL 0.75 guide provided a horizontal trajectory between the IVC and the aorta. The heel of the AL 0.75 guide against the opposite wall of the IVC provided the support required to maintain stability of the guide tip during advancement of the electrified Astato wire and subsequent delivery of the Finecross and Navicross catheters (both Terumo) (Figure 1H). Once transcaval access was established (Moving image 1), the standard procedural transcaval technique was performed, achieving successful technical and clinical results1. An Agilis steerable sheath (Abbott) was used to facilitate deployment of the patent ductus arteriosus occluder device to close the aorta at the completion of the case (Moving image 2, Moving image 3).
This case highlights the importance of preprocedural assessment of iliofemoral venous patency during computed tomography TAVI analysis for appropriate planning of the TC TAVI procedure. A horizontal trajectory between the IVC and the Ao as well as the stability of the guide tip against the aortic wall of the IVC are critical for successful TC access. The modification to the AL coronary guide described in this report should allow successful TC TAVI from the left CFV access in most cases.
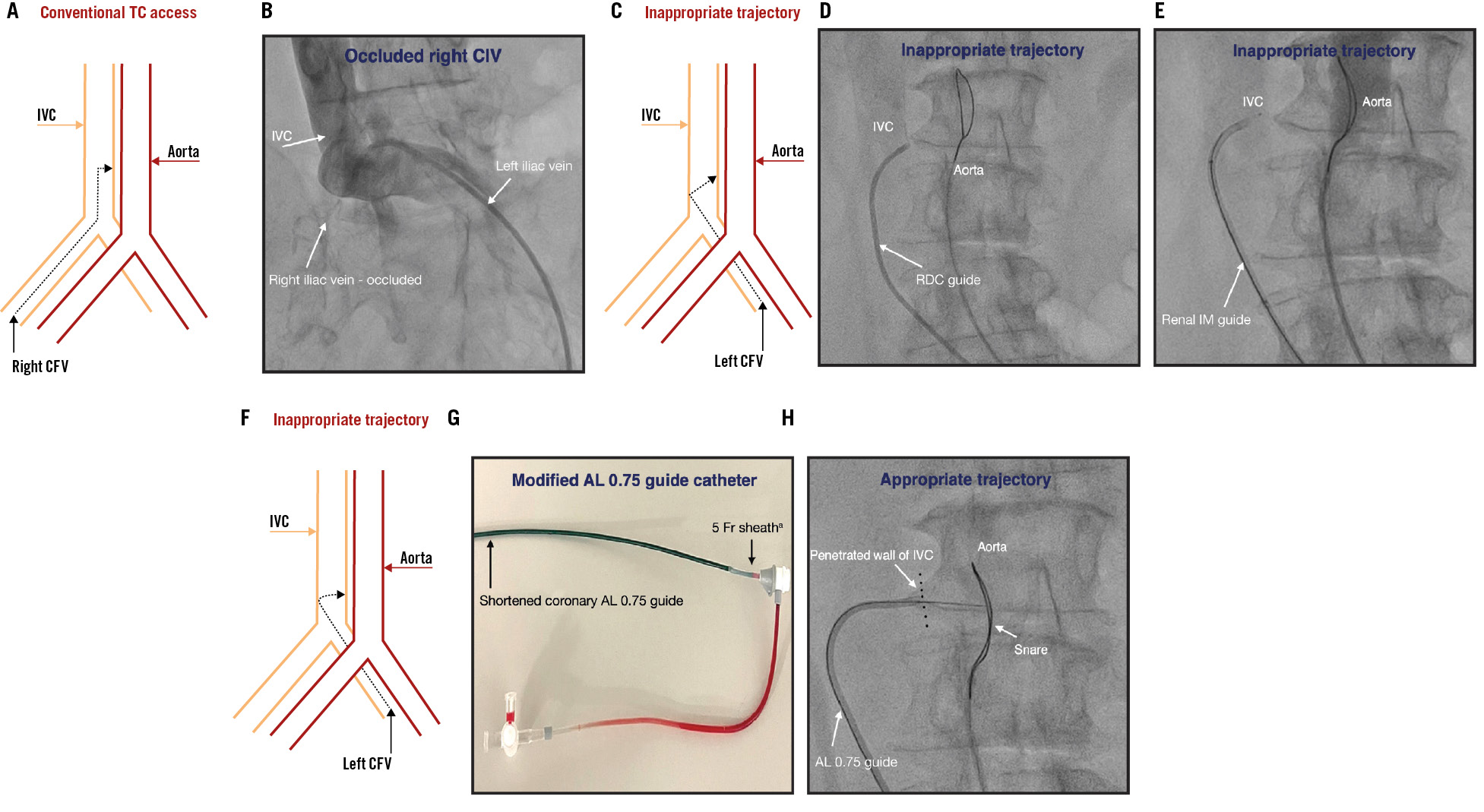
Figure 1. Challenges and strategies with left-sided transcaval TAVI. A) Line drawing illustrating conventional transcaval access and appropriate guide trajectory in right-sided venous approach due to favourable angulation between the right CIV and IVC. B) Venogram under fluoroscopy showing occlusion of the right CIV. C) Line drawing illustrating inappropriate guide trajectory for transcaval access in left-sided venous approach due to unfavourable angulation between the left CIV and IVC. D) Fluoroscopy showing failure to achieve horizontal trajectory for transcaval access with the RDC guide catheter via left-sided venous approach. E) Fluoroscopy showing failure to achieve a horizontal trajectory for transcaval access with renal IM guide catheter via left-sided venous approach. F) Line drawing illustrating achievement of appropriate trajectory for transcaval access with a modified AL 0.75 guide catheter. G) Modified coronary AL 0.75 guide catheter attached to a shortened 5 Fr sheath. H) Fluoroscopy showing a horizontal trajectory for transcaval access achieved with the modified AL 0.75 guide catheter. aBy Cordis. AL: Amplatz left; CFV: common femoral vein; CIV: common iliac vein; IM: internal mammary; IVC: inferior vena cava; RDC: renal double curve
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Fluoroscopy demonstrating successful transcaval access with a modified coronary AL 0.75 guide.
Moving image 2. Fluoroscopy demonstrating deployment of patent ductus arteriosus occluder device to close the transcaval tract.
Moving image 3. Aortogram showing successful closure of transcaval tract with type 1 stable aortocaval fistula.