Cory:
Unlock Your AI Assistant Now!
Until recently, only small-scale randomised controlled trials (RCTs) had evaluated the impact of invasive approaches in elderly patients with acute coronary syndromes (ACS). To address the inherent limitations of these smaller trials, a comprehensive individual participant data (IPD) meta-analysis was conducted1. Following this meta-analysis, the SENIOR-RITA trial2, with a sample size comparable to the total sample of the IPD meta-analysis1 was published. This RCT2 found no evidence that an invasive strategy reduces cardiovascular death or non-fatal myocardial infarction (MI) compared to a conservative approach in older patients with non-ST-segment elevation myocardial infarction. Here, we employ this large RCT2 to update the meta-analysis1 within a Bayesian framework, providing a probabilistic perspective on the interpretation of the estimated effects.
We considered the comprehensive IPD meta-analysis of 6 small-scale RCTs (sample sizes ranging from 106-457, with a total number of 1,479 individuals) evaluating the impact of percutaneous coronary intervention (PCI) in elderly ACS patients1. The recently published SENIOR-RITA trial2 included 1,518 patients ≥75 years old with ACS. Patients in all these trials were randomised to an invasive strategy with coronary angiography and revascularisation or guideline-driven medical therapy. We used a Bayesian random-effects meta-analysis to obtain the posterior distribution of the hazard ratios (HR) with a minimally informative prior for the treatment effect (i.e., N(0,102)) and a vague prior for the standard deviation of random effects, i.e., the positive part of a standard normal distribution N(0,1)T(0,). We fitted the model via Markov Chain Monte Carlo using 6 chains, 10,000 iterations each, after an initial adaptation of 500 iterations. We checked convergence by visually checking the posterior distribution and the mixing of the chains, and via R-hat. We performed a series on sensitivity analyses, using different priors for the treatment effects and heterogeneity parameter. All analyses were performed in R software (R Foundation for Statistical Computing).
For the primary composite outcome of all-cause mortality or MI, we found weak evidence of superiority of the invasive strategy compared to the conservative treatment. The estimated effect size was HR 0.89 (95% credible interval [CrI]: 0.68-1.14) and was similar to the one from the IPD meta-analysis. The probability that the invasive strategy is better than the conservative one (corresponding to HR <1) was estimated at 86% (Figure 1A). Detailed results are provided in Supplementary Appendix 1. For the individual outcomes of all-cause and cardiovascular mortality, we found weak evidence that an invasive strategy may be detrimental, with posterior probabilities of 91% and 67%, respectively, in favour of the conservative approach (Figure 1B, Figure 1C), similar to the findings from the SENIOR-RITA trial. Conversely, we found strong evidence that an invasive strategy reduces the hazard of MI (HR 0.70 [95% CrI: 0.56-0.86]) compared to a conservative approach, and there was almost certainty (posterior probability ~100%) that the true HR is <1 (Figure 1D). For urgent revascularisation, we found very strong evidence of a beneficial effect of an invasive strategy (HR 0.28 [95% CrI: 0.20-0.41]), with ~100% probability that the invasive approach is better (Figure 1E). However, for stroke we found no evidence for a difference between the treatment strategies (HR 0.97 [95% CrI: 0.67-1.43]), with a 55% posterior probability that invasive is better.
Overall, the inclusion of the large RCT2 in the meta-analysis did not change the direction of the effects for most outcomes but considerably increased the precision of the estimates. The probabilistic interpretation facilitates a nuanced understanding of the treatment effects and allows for quantitative statements that are easy to understand, thus enhancing the decision-making process. This is especially pertinent for patients who are at risk of multiple clinical outcomes. In this context, non-mortality outcomes may be more relevant, as all-cause mortality lacks sensitivity and specificity for assessing interventions, especially in elderly ACS patients34. Here, the increase in life expectancy among elderly patients in recent years should be factored into treatment decisions for those with ACS. However, decision-making remains complex due to comorbidities and frailty in this population. As a result, shared decision-making is crucial to ensure that interventions align with the patient’s values, preferences, health status, and overall goals for quality of life56. Unfortunately, the type of data that was available from the studies (aggregated data) and the absence of quality-of-life metrics prevented us from evaluating the impact of either strategy on quality of life, which may be more relevant for this patient group.
The present analysis illustrates how accumulated evidence can be interpreted within a Bayesian framework and provides insights into the potential benefits and risks of invasive procedures for a specific group of patients, which healthcare providers can share with patients and their families to support informed decision-making. As a direction for future research, in such scenarios involving treatments with varying effectiveness-safety trade-offs, combining patient-level data from multiple studies using dedicated statistical methods may allow accurate predictions of intervention effects at the patient level. This approach may empower practitioners to make better-informed decisions and help patients receive treatments that are most aligned with their individual characteristics, preferences, and needs.
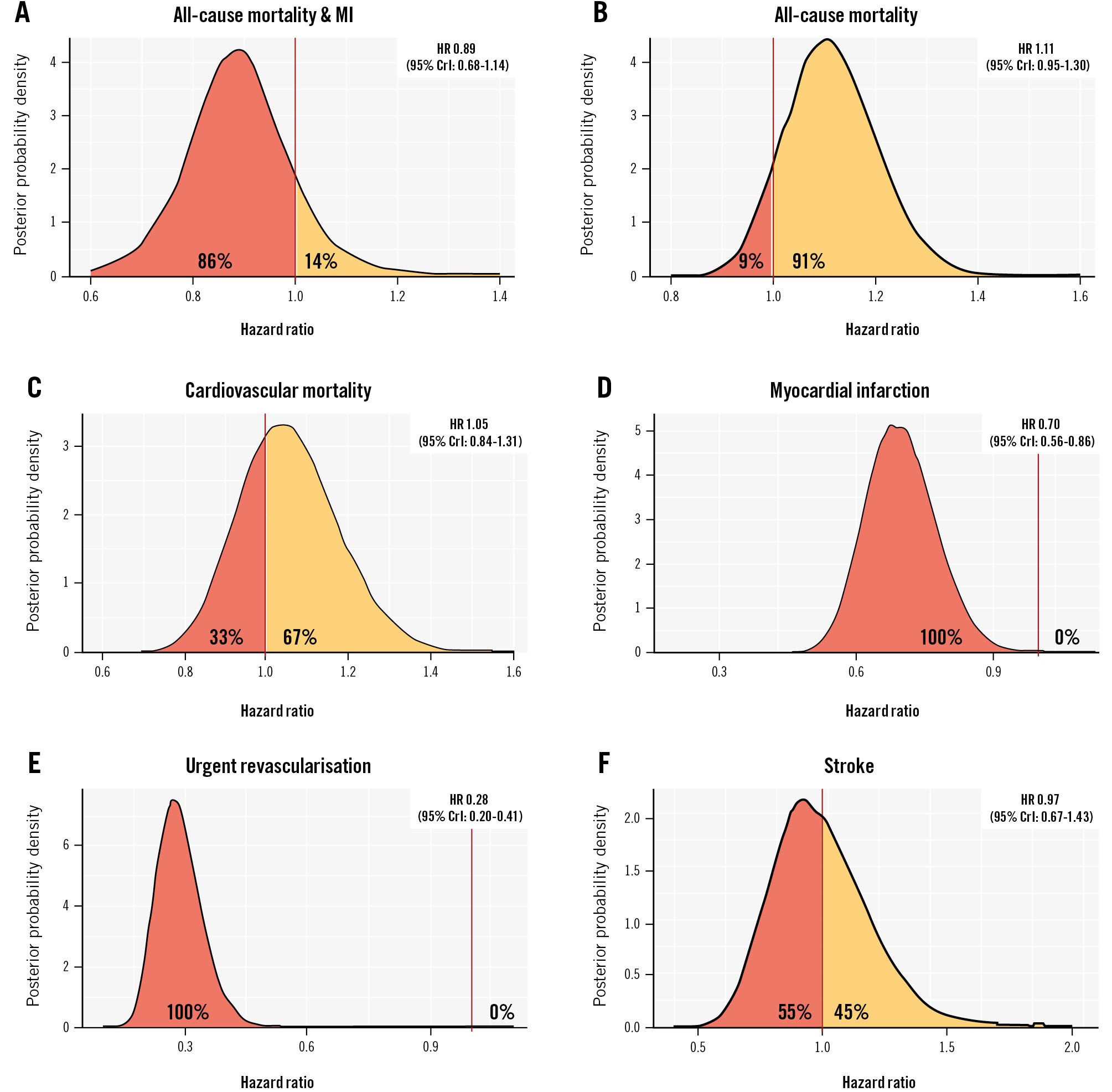
Figure 1. Posterior distributions for the different outcomes. Combined posterior distributions for the composite endpoint of all-cause mortality and myocardial infarction (A), all-cause mortality (B), cardiovascular mortality (C), myocardial infarction (D), urgent revascularisation (E) and stroke (F). We abstracted the effect sizes in hazard ratios (HR) as reported from each trial, along with the corresponding confidence intervals. For the Bayesian meta-analysis of the primary composite outcome of all-cause mortality or myocardial infarction, we included effect estimates from the individual trials separately. For the adjudicated secondary outcomes, we were unable to obtain study-level data from the 6 RCTs in the meta-analysis. Thus, we used the summary estimates from the one-stage, random-effects, IPD meta-analysis as our prior distribution, which we updated using the results reported by SENIOR-RITA to obtain our posterior estimates. The treatment effects are expressed in hazard ratios (95% credible intervals [CrI]). The percentages shown to the left/right of the null effect in the graphs represent the posterior probability that the invasive strategy is better/worse than conservative treatment. IPD: individual participant data; MI: myocardial infarction; RCT: randomised controlled trial
Conflict of interest statement
The authors have no conflicts of interest relevant to the contents of this paper to declare.
Supplementary data
To read the full content of this article, please download the PDF.