Cory:
Unlock Your AI Assistant Now!
The publication of major randomised controlled trials (RCTs) about patent foramen ovale (PFO) provided much needed evidence that made a longstanding intervention a mainstream cryptogenic stroke prevention strategy. In our real-world study of 479 patients with the Amplatzer PFO Occluder (Abbott), at the median follow-up of 9.3 years, we noted a 1.5% risk of stroke (0.16/100 person-years) and 4% risk of transient ischaemic attack (TIA; 0.44/100 person-years)1.
Few things are as disheartening to patients and physicians alike than a positive bubble study after PFO closure. Wasn’t this the reason we pursued device closure at the outset? It is a source of anxiety and consternation that prompts the question “what do we do now?”
We do not have an ideal methodology to evaluate the risk of stroke recurrence after PFO closure. We default to the use of saline contrast echocardiography, which typically has 16-38 μm microbubbles, larger than the 7-8 μm diameter of pulmonary capillaries. These bubbles may shrink in size when dissolved in a solution because of the effects of diffusion and surface tension. Smaller bubbles may traverse the lung circulation, leading to false positive results. Pseudocontrast, the appearance of weakly echodense material from the pulmonary veins following a Valsalva or cough, may also contribute2.
In practice, bubble studies are rarely homogeneous as a group, with variable right atrial opacification. A large Eustachian valve often prevents bubbles from approximating the septum diagnostically. While different quantification schemas have been used in RCTs, it seems almost absurd to use a single two-dimensional image to quantitate a three-dimensional volume where bubbles move rapidly in and out of the echocardiographic imaging plane.
Whether or not a positive bubble study after PFO closure is materially significant as a risk for recurrent stroke is a very important and, as yet, unresolved issue. Cohort studies examining this issue are often methodologically flawed, lump stroke and TIA together to increase power, and are insufficiently adjudicated34. If a positive bubble study is going to be used to justify a second, much less studied intervention, it is quite important to establish this more definitively.
In a pooled analysis of individual patient data from all PFO RCTs, complete PFO closure, defined as no residual shunt (RS) at 6-18 months post-procedure, was observed among 89.9% of 1,475 patients5. At a median follow-up of 57 months, recurrent ischaemic stroke was reported in 2.3% of patients with complete closure compared with 2.7% with any RS (p=0.74). The rate of the composite outcome of recurrent ischaemic stroke, TIA, or vascular death was also not different between the groups (5.0% vs 6.0%; p=0.58). Is a positive bubble study important, or is the device which holds the PFO, previously wafting in the breeze, approximated?
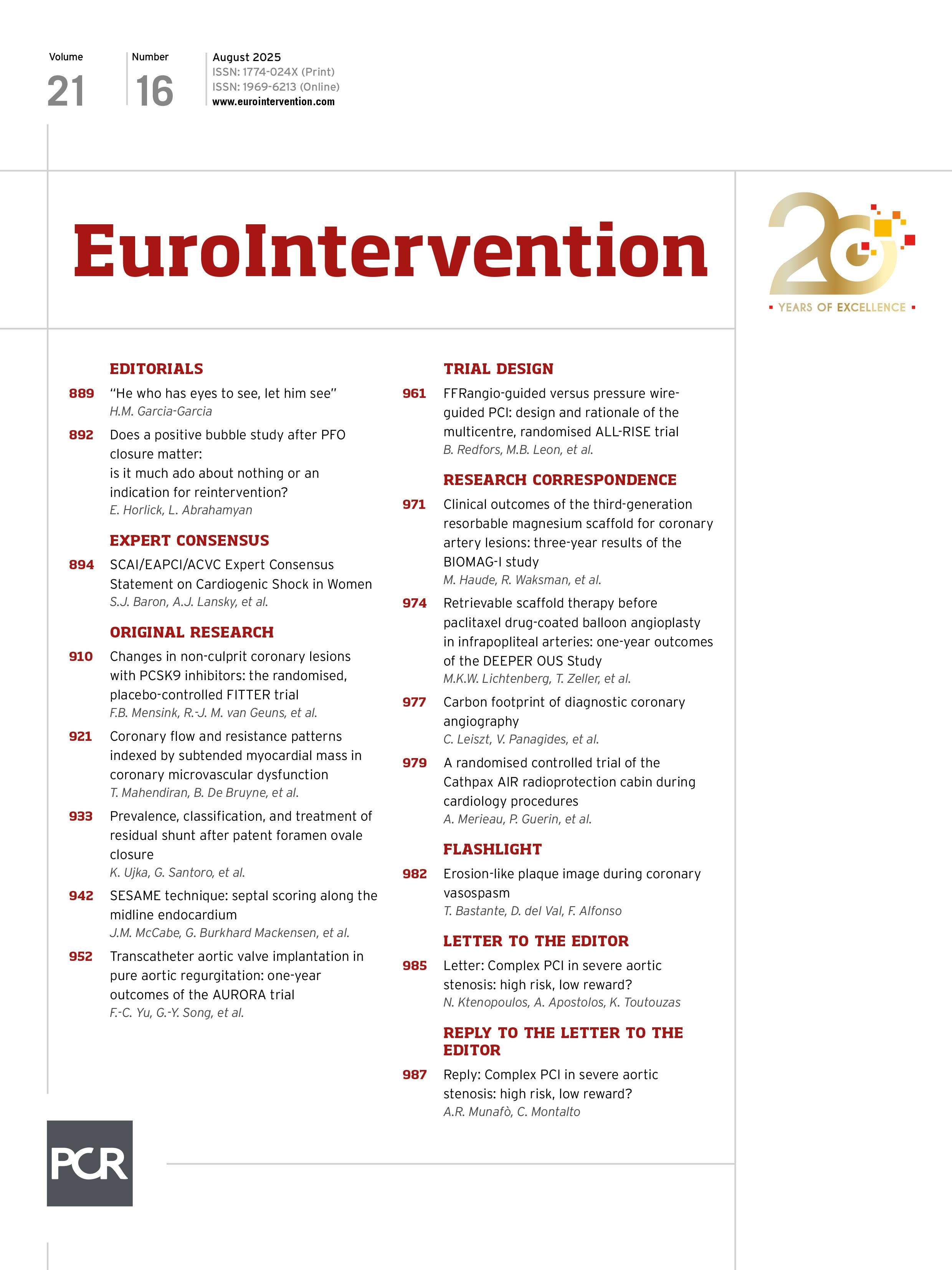
In this issue of EuroIntervention, Ujka et al examine a retrospective cohort of 2,362 patients who underwent PFO closure from 2000-2022 at three Italian centres using five different devices6. The outcome reporting was focused on 207 patients with confirmed RS on contrast-enhanced transcranial Doppler at 12 months post-procedure, of whom 84 had a significant shunt (>10 bubbles), and 106 agreed to undergo a repeat procedure. They classified patients morphologically into 3 types: (1) a tunnel-like intradevice shunt, (2) extradevice shunt, (3) RS consisting of characteristics that were not present in the other 2 groups. The type 1 shunts were treated with a variety of plugs, type 2 with double-disc devices, and type 3 with double-disc devices in the case of incomplete closure with NobleStitch EL (Heartstitch), or coils and plugs as necessary.
Aside from the NobleStitch EL device which had a 20% RS rate, no other analysis is pertinent with respect to device type or size and the contribution to RS, given there was no systematic approach to a priori device selection, as acknowledged by the authors in their discussion.
Of the 41 patients with type 1 RS, vascular plugs were used to close 80.4% of leaks, while 7 had leaks that could not be crossed with a wire. In the type 2 group, 30/33 patients were found to have an accessory atrial septal defect (ASD). This is unexpected given the original procedures were done with transoesophageal echocardiography (TOE) guidance, balloon interrogation and a bubble study at the end of the procedure. Of the type 3 leaks, 10/14 patients had a suspected loosening of the NobleStitch knot, and two had a potential late onset tear in the septum. The RS closure procedure failed in 10/94 patients. While 89% (84/94) of all the RS closure procedures had a negative TOE bubble test at the end of the procedure, only 79 of 84 patients underwent a 1-year contrast-enhanced transcranial Doppler evaluation reporting any grade RS in 15.2% and significant RS in 8.9%. Given 30 ASDs were missed originally, it is unclear how to view these results.
The authors should be congratulated for sharing a series of complex interventions for dealing with RS after PFO closure. Their study suffers from typical sources of uncertainty present in retrospective studies, and we would scarcely criticise them for that; experience is a powerful teacher, and demanding prospective standards from this type of study are misplaced.
The context of this study is important. We lack an optimal diagnostic test to predict which of our patients post-PFO closure are at risk for recurrent events. The saline contrast study is ill-suited, but widely available and used, to evaluate this risk, especially when it is exceptionally low. A positive saline contrast study introduces pressure to reintervene, which may not be justified, and the results of reintervention remain unclear. Using the lack of an RS after repeat intervention as a surrogate for a successful stroke prevention intervention is a difficult jump to make.
Despite the lack of serious adverse events in this study, a cautious approach is mandated when considering “fixing” an intervention that by rigorous RCTs has exceptionally low event rates5. We know far less about fixing leaks related to the devices we choose than we do about the original intervention for PFO closure. As a community, we are desperately in need of not only studies that compare devices after their market approval, but also better algorithms to match the original closure device to the anatomy of the defect. Finding the sweet spot for the latter in a systematic way may reduce the likelihood of an RS. A wholehearted attempt to understand the natural history of patients with RS after PFO closure is an important piece of our management of these patients.
Conflict of interest statement
E. Horlick reports grants or contracts from Occlutech; grants/contracts, honoraria, consulting fees from Abbott; and participation in an Abbott advisory board. L. Abrahamyan has no conflicts of interest to declare.