Cory:
Unlock Your AI Assistant Now!
Mitral transcatheter edge-to-edge repair (M-TEER) is the gold-standard therapy for carefully selected patients with severe ventricular secondary mitral regurgitation (SMR) who remain symptomatic despite guideline-directed medical therapy (GDMT)1. However, the residual 5-year risk of death and heart failure (HF) hospitalisation after intervention in these patients is very high23. Furthermore, moderate residual mitral regurgitation (MR) after M-TEER is associated with an increased risk of clinical events as compared to mild or less residual MR4. The latter is in line with epidemiological data showing a possible prognostic role of moderate MR in HF populations5. Recently, the RESHAPE-HF2 trial, including 53% of patients with an effective regurgitant orifice area (EROA) <0.30 cm2 and showing a beneficial effect of M-TEER+GDMT as compared to GDMT alone regardless of baseline SMR severity, has raised the question of whether M-TEER indication can be expanded to patients with moderate ventricular SMR6. In addition, an analysis from the EXPANDed studies – single-arm prospective registries evaluating the safety and efficacy of the latest-generation MitraClip (Abbott) − reported favourable outcomes in a subgroup of patients with moderate SMR7.
In this issue of EuroIntervention, Lurz et al report 1-year data from the MiCLASP study, a European post-market registry assessing the safety and efficacy of M-TEER using the PASCAL device (Edwards Lifesciences)8. In this analysis, patients with SMR were stratified according to baseline MR severity: 101 patients had moderate SMR (2+) and 197 had more than moderate SMR (≥3+). M-TEER yielded a significant MR reduction in both groups, sustained up to 1 year. Significant LV reverse remodelling and improvement in quality of life (QoL) were observed in both groups. Notably, the annualised HF hospitalisation rate dropped by over 60% in both patients with SMR 2+ and SMR ≥3+. Finally, survival at 1 year was comparable between groups (90.0% in SMR 2+ vs 84.2% in SMR ≥3+; p=0.176). The main limitations of the study are the observational and single-arm design with no control arm for GDMT adherence, as well as limited follow-up (1 year) and some missing echocardiographic data after intervention8. Nonetheless, the authors should be congratulated for this study that adds an important piece to the puzzle of current evidence on M-TEER in moderate SMR.
In MiCLASP, similarly to EXPANDed, the proportion of patients with moderate SMR is lower than in RESHAPE-HF2. Furthermore, as compared to RESHAPE-HF2, the registries include slightly older patients, a higher proportion of females, patients with better left ventricular (LV) dimensions and function, as well as those with a lower rate of HF hospitalisation during the year before enrolment (Table 1). A possible explanation is the inclusion of patients with atrial SMR in the registries and the exclusion of patients with preserved LV function from the RESHAPE-HF2 trial. In this regard, a stratification by atrial versus ventricular aetiology would be of great interest in future randomised controlled studies (RCTs) assessing the role of M-TEER in patients with moderate SMR.
In both MiCLASP and EXPANDed, there was a similar improvement in symptoms, QoL and HF hospitalisation rate in SMR 2+ and SMR ≥3+ groups. However, in MiCLASP, the proportion of patients with residual MR ≤1+ at 1 year was higher among those with baseline SMR 2+ vs SMR ≥3+ (90% vs 78%). This finding, although less pronounced, was reported also in the EXPANDed analysis where 97% of patients had residual MR ≤1+ at 1 year in the moderate group versus 92% in the severe group. These results, though limited by the partial availability of echocardiographic data during follow-up, confirm that the ability of achieving optimal results after M-TEER is more frequent in patients with a lower EROA9. Since it is known that residual MR ≤1+ is associated with a better prognosis compared to residual MR 2+4, it could be speculated that these differences may affect clinical outcomes during longer follow-up (>1 year) in these low-risk populations.
Significant LV reverse remodelling after M-TEER was observed in both MiCLASP and EXPANDed78, whereas LV reverse remodelling data from RESHAPE-HF2 are not yet available. Of note, a subanalysis of COAPT including only patients with an EROA ≥0.3 mm2 did not show interaction between LV reverse remodelling and the beneficial effect of M-TEER on the primary endpoint10. Importantly, no safety alerts emerged in patients with moderate SMR treated in either RESHAPE-HF2, EXPANDed, or MiCLASP.
Overall, the results of these three studies suggest that M-TEER may have a major role in patients with moderate SMR. Early treatment could ensure optimal MR reduction and prevent the risk of HF progression and adverse events. This proof of concept requires confirmation by RCTs specifically targeting moderate SMR populations. Meanwhile, managing moderate SMR in patients with HF requires a personalised approach that should take into account symptoms, clinical history, response to exercise, tolerance to medical therapy, and mitral valve anatomy.
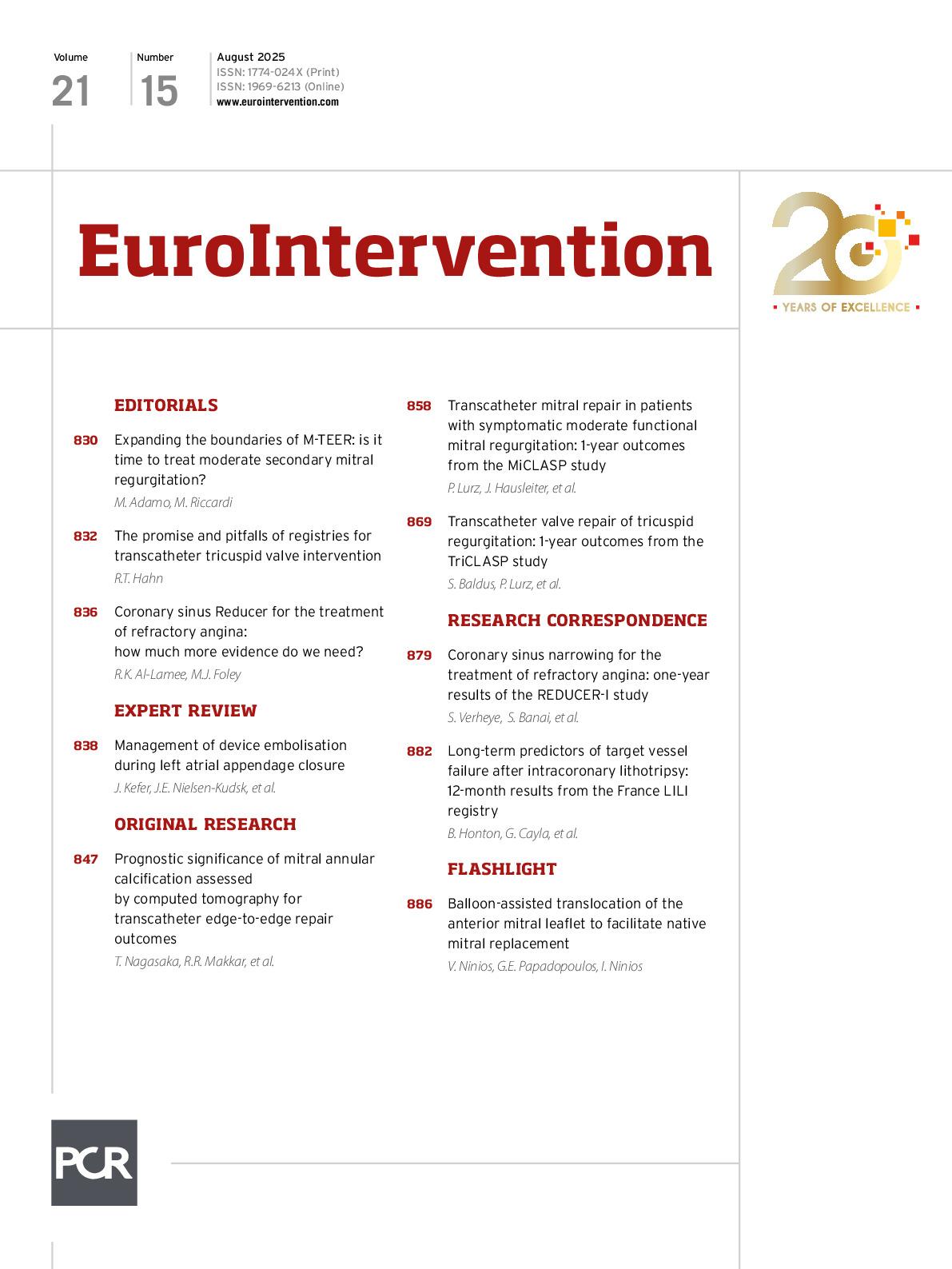
Table 1. Baseline characteristics of studies including patients with moderate SMR undergoing M-TEER.
| RESHAPE-HF2 | EXPANDed* | MiCLASP* | |
|---|---|---|---|
|
Sample size (n) |
505 |
968 |
322 |
|
Mean age, years |
70 |
75 |
75 |
|
Male (%) |
80 |
58 |
60 |
|
NYHA III/IV (%) |
75 |
78 |
76 |
|
Prior HFH (%) |
66 |
57 |
52 |
|
Mean LVEF, % |
31 |
39 |
42 |
|
Mean LVEDV, mL |
211 |
171 |
176 |
|
Mean EROA, mm2 |
0.25 |
0.25 |
0.29 |
|
Moderate MR (%) |
53 |
36 |
31 |
|
*Secondary MR cohort. EROA: effective regurgitant orifice area; HFH: heart failure hospitalisation; LVEDV: left ventricular end-diastolic volume; LVEF: left ventricular ejection fraction; MR: mitral regurgitation; M-TEER: mitral transcatheter edge-to edge repair; NYHA: New York Heart Association; SMR: secondary mitral regurgitation |
|||
Conflict of interest statement
M. Adamo reports speaker fees from Abbott and Edwards Lifesciences. M. Riccardi has no conflicts of interest to declare.