Cory:
Unlock Your AI Assistant Now!
The Nordic Aortic Valve Intervention 2 (NOTION-2) trial was a randomised controlled trial (RCT) comparing transcatheter aortic valve implantation (TAVI) with surgical aortic valve replacement (SAVR) in young, low surgical risk patients with severe tricuspid (N=270) and bicuspid (N=100) aortic stenosis (AS)1. The primary endpoint of the trial − a composite of all-cause mortality, stroke or rehospitalisation at 12 months − was comparable in tricuspid AS patients (TAVI: 8.7% vs SAVR: 8.3%; hazard ratio [HR] 1.0, 95% confidence interval [CI]: 0.5-2.3) but differed significantly in those with bicuspid AS (TAVI: 14.3% vs SAVR: 3.9%; HR 3.8, 95% CI: 0.8-18.5). These findings can only be considered hypothesis-generating owing to the relatively small sample size, but they raise important concerns as indications for TAVI expand to include younger patients in whom bicuspid AS is more frequently encountered. To address these concerns, we conducted an in-depth, patient-level analysis of individual trial participants who experienced cardiovascular (CV) mortality or stroke following either TAVI or SAVR (Figure 1), evaluating clinical characteristics, anatomical features determined from the preprocedural computed tomography (CT), and procedural images and reports to obtain a deeper understanding of the factors responsible for these hard clinical endpoints. In this young, low surgical risk AS population, the rate of intraprocedural CV mortality amongst tricuspid AS patients was reassuringly low: only 1/135 (<1%) patients undergoing SAVR and no patients undergoing TAVI. In contrast, TAVI for bicuspid AS was associated with 1 intraprocedural CV mortality and 1 CV mortality at 58 days, both of which occurred in patients with Sievers type 2 anatomy (the only such patients treated with TAVI in the trial). The intraprocedural mortality was caused by annular rupture following predilatation with a conservatively sized 18 mm balloon, whereas the later CV mortality occurred following cardiac arrest with an unexplained haemothorax. Further analysis of the tricuspid AS cohort revealed that all strokes in the SAVR cohort (3/135, 2.2%) occurred in the immediate postprocedural period (1-5 days following surgery). In contrast, for TAVI in tricuspid AS, there were only 2 intraprocedural strokes, while 5 strokes occurred at a much later timepoint (59-268 days after the procedure). Of these late strokes, one was related to infective endocarditis, whereas the remaining four were all of ischaemic origin in patients with underexpanded transcatheter aortic valve (TAV) stent frames (ACURATE neo2 [Boston Scientific] n=2; SAPIEN 3 [Edwards Lifesciences] n=1, Portico [Abbott] n=1) receiving either antiplatelet or anticoagulant therapy. In two of these cases, there was proof of hypoattenuating leaflet thickening (HALT) on cardiac CT at the time of stroke. In the bicuspid AS cohort, there were no strokes in patients undergoing SAVR and two periprocedural ischaemic strokes in those who underwent TAVI. Both patients had severely calcified bicuspid Sievers type 1 valves (>1,500 mm3). These were treated with an Evolut TAV (Medtronic), requiring multiple repositioning manoeuvres. Additionally, in one patient, significant stent frame in-folding necessitated device retrieval and exchange. Cerebral embolic protection was not utilised for either patient. This in-depth analysis of all patients experiencing CV mortality or stroke within the NOTION-2 trial highlights the technical complexities of TAVI in patients with bicuspid AS. The finding of TAV underexpansion in patients presenting with late ischaemic strokes is concerning and consistent with results of the recent ACURATE IDE RCT, in which TAV underexpansion was associated with a 3-fold increase in stroke risk2. Previous studies have also linked TAV underexpansion to increased leaflet thickening and/or thrombosis, which may act as the pathophysiological precursor of delayed stroke34. TAV stent frame expansion can also be restricted by excess calcification, which further increases procedural complexity and risk and is often observed in bicuspid phenotypes. Indeed, intraprocedural stroke was observed in 2 TAVI patients with heavily calcified bicuspid Sievers type 1 anatomy requiring repeated self-expanding TAV repositioning, while CV mortality was only observed in bicuspid patients with Sievers type 2 anatomy who underwent TAVI. Based upon this analysis, we provide the following practical recommendations: (1) detailed preprocedural evaluation of the bicuspid phenotype and the extent and pattern of calcification should be undertaken prior to Heart Team discussion; (2) caution is advised when evaluating TAVI in patients with bicuspid Sievers type 2 anatomy, and cardiac surgery should be recommended as the first-line treatment choice for this phenotype; (3) multiple TAV repositioning manoeuvres should be avoided where possible, particularly in patients with heavily calcified anatomy and/or with an advanced degree of aortopathy, which may increase the risk of aortic dissection. Effective predilatation should be considered in severely calcified cases; (4) cerebral embolic protection should be considered when treating heavily calcified and challenging bicuspid anatomy; and (5) TAV stent frame underexpansion should be assessed for all TAV platforms and corrected by means of targeted postdilatation to ensure that adequate expansion is achieved. Calcium debulking technologies or “tricuspidisation” of bicuspid aortic valves using leaflet modification techniques may prove to be important developments, particularly in patients with more challenging calcified bicuspid anatomy5. The patient-level data derived from the NOTION-2 trial indicate the need to conduct large dedicated RCTs in younger patients with bicuspid AS to determine optimal treatment strategies for this challenging cohort. Nevertheless, a detailed preprocedural assessment of the bicuspid phenotype should remain a crucial and unmissable step of the RCTs themselves. 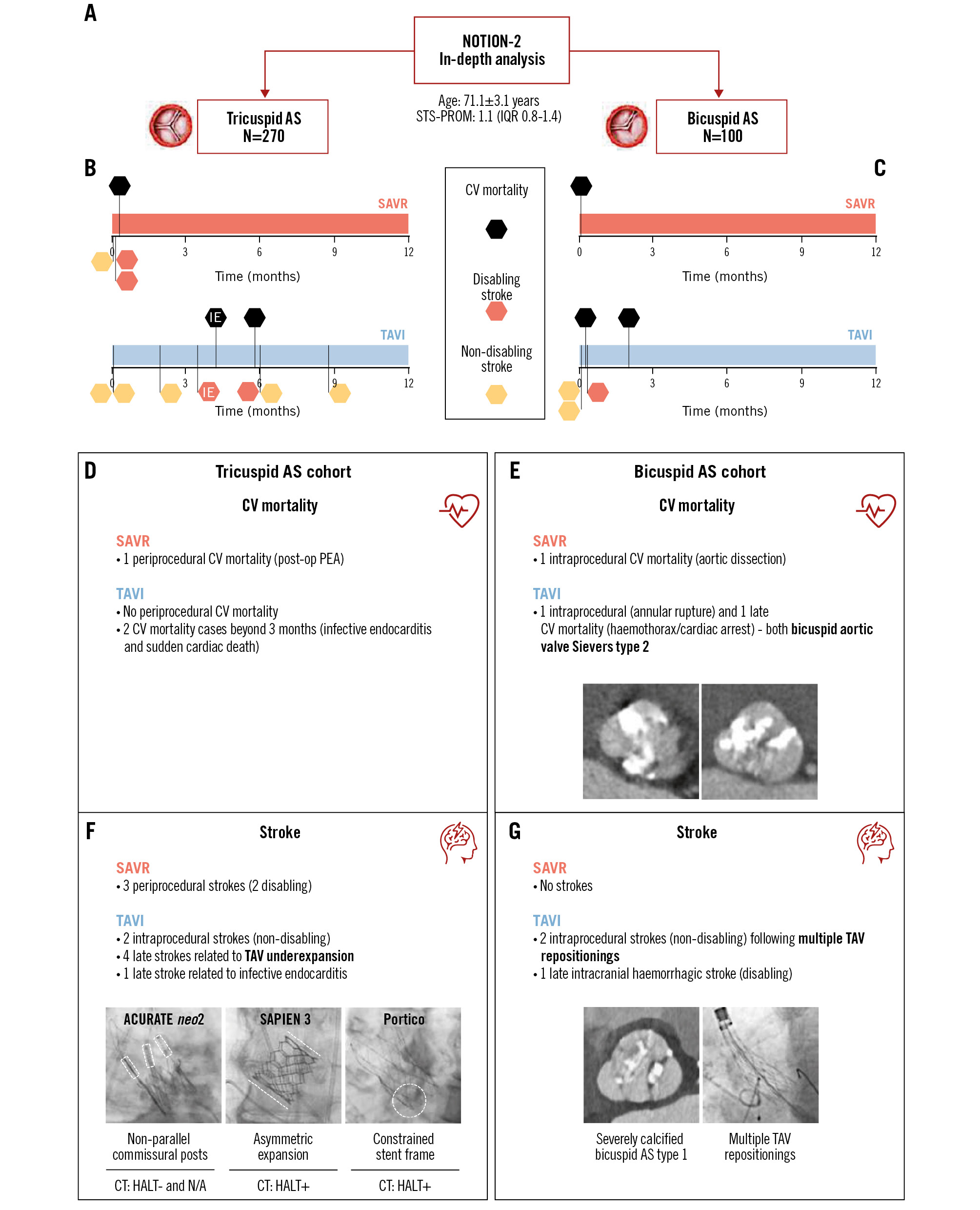
Figure 1. Cardiovascular mortality and stroke in the NOTION-2 trial. A) Study details. Timing and cause of cardiovascular mortality and stroke in individual patients with tricuspid (B) or bicuspid AS (C) undergoing SAVR or TAVI. D) Tricuspid AS: CV mortality. E) Bicuspid AS: CV mortality. F) Tricuspid AS: stroke. G) Bicuspid AS: stroke. AS: aortic stenosis; CV: cardiovascular; HALT: hypoattenuating leaflet thickening; IE: infective endocarditis; IQR: interquartile range; N/A: not available; PEA: pulseless electrical activity; SAVR: surgical aortic valve replacement; STS-PROM: Society of Thoracic Surgeons Predicted Risk of Mortality; TAV: transcatheter aortic valve; TAVI: transcatheter aortic valve implantation
Conflict of interest statement
A. Khokar has received speaker fees/honoraria from Abbott, Boston Scientific, and Medtronic. L. Sondergaard is an employee of Abbott. B. Prendergast has received educational and research grants from Edwards Lifesciences; speaker fees from Edwards Lifesciences, Medtronic, and Abbott; and consultancy fees from Anteris and Microport; O. De Backer has received consulting fees from Abbott, Boston Scientific, and Medtronic. The other authors have no conflicts of interest.