A 36-year-old gentleman was admitted with inferior STEMI due to a very late thrombosis (565 days) of a 3.5×12 mm bioresorbable vascular scaffold (BVS) (Absorb; Abbott Vascular, Santa Clara, CA, USA) in the distal right coronary artery (RCA) (Figure 1B, Moving image 1). The BVS had been previously implanted for an acute thrombotic occlusion of the vessel (Figure 1A). After the implant, a standard dual antiplatelet therapy (DAPT) with aspirin 100 mg and prasugrel 75 mg per day was prescribed for 12 months and then discontinued in favour of aspirin alone. After mechanical thrombectomy in the BVS, optical coherence tomography (OCT) (Moving image 2) showed residual thrombus apposition all along the scaffold (Figure 1D), suboptimal stent expansion (maximal diameter 2.3 mm; Figure 1E) and a proximal small area of uncovered struts (Figure 1F). The lesion was amended by stent-in-stent with a Biolimus A9™ (3.5×24 mm) drug-eluting stent (DES) (Biosensors International Group Ltd, Singapore) (Figure 1C, Moving image 3).
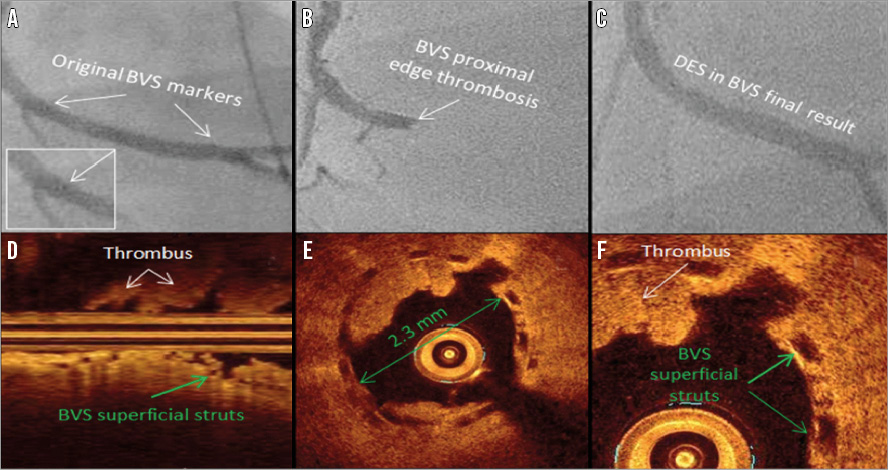
Figure 1. Angiographic and OCT views of the very late BVS thrombosis. A) Final results after BVS implantation to the distal RCA (white arrows: BVS markers). B) Very late thrombosis of the BVS proximal edge (white arrow: BVS markers). C) Biolimus A9 stent-in-stent, final result. D) Longitudinal OCT analysis showing diffuse residual thrombus (white arrows) and uncovered BVS struts (green arrow). E) Short-axis OCT analysis showing original BVS underexpansion (green arrows). F) Short-axis OCT magnification showing thrombus (white arrow) and uncovered BVS struts (green arrows).
To the best of our knowledge this is the first report on a “very late” BVS thrombosis most probably related to suboptimal BVS expansion (the BVS was not optimally post-dilated), and malapposition causing the incomplete healing process of the endothelium and thus the lack of strut coverage that led to thrombus formation. As the very late thrombosis occurred 200 days after DAPT suspension, it is unknown whether DAPT had a real protective role. DAPT was restored and empirically prescribed for a longer time (two years).
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
Moving image 1. Angiography of the RCA with very late thrombosis of the BVS.
Moving image 2. OCT of the RCA showing residual thrombus, suboptimal stent expansion and a proximal small area of uncovered struts.
Moving image 3. Angiography of the zotarolimus stent-in-stent to the RCA.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Angiography of the RCA with very late thrombosis of the BVS.
Moving image 2. OCT of the RCA showing residual thrombus, suboptimal stent expansion and a proximal small area of uncovered struts.
Moving image 3. Angiography of the zotarolimus stent-in-stent to the RCA.