Cory:
Unlock Your AI Assistant Now!
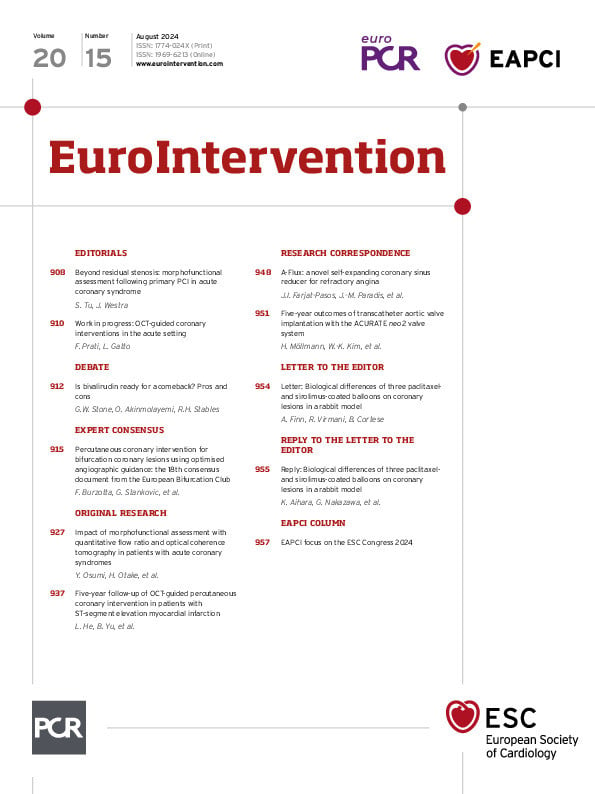
The role of wire-based physiology to guide and evaluate revascularisation in acute coronary syndrome (ACS) is still heavily debated. While fractional flow reserve (FFR)-guided complete revascularisation is superior to culprit-only revascularisation, multiple studies have recently failed to show an advantage of FFR-guided complete revascularisation over angiography-guided complete revascularisation1. The conflicting evidence underlying pressure-based assessment in ACS may be related to acute and temporary disturbances in the microcirculation. Image-derived physiology has the theoretical advantage of being less affected by microvascular involvement in the acute setting of ACS. Indeed, quantitative flow ratio (QFR) was largely unchanged for paired measurements in non-culprit lesions measured during primary percutaneous coronary intervention (PCI) or in a staged setting2. Furthermore, initial reports have documented the prognostic value of post-PCI QFR in ACS patients3. In addition to physiological lesion assessment, high-risk plaque features in non-culprit lesions that are not flow limiting (FFR>0.80) are associated with worse clinical outcome4. Hence, there may exist a complementary value of physiology and morphology for risk stratification.
In this issue of EuroIntervention, Osumi et al assessed the prognostic impact of combined post-PCI QFR and OCT in culprit vessels immediately after primary PCI5. The authors retrospectively performed QFR analysis in a total of 456 patients that underwent optical coherence tomography (OCT)-guided PCI at 5 Japanese institutions from 2010 to 2020. The primary endpoint was target vessel failure (TVF), defined as a composite of cardiac death, target vessel-related myocardial infarction and ischaemia-driven target vessel revascularisation. Following the exclusion of some patients, mainly because of suboptimal image quality for QFR and/or OCT analysis, a total of 298 patients were included for the final analyses. In the median follow-up period of 999 days, the presence of thin-cap fibroatheroma (TCFA) in non-culprit segments (NCS) (hazard ratio [HR] 3.47, 95% confidence interval [CI]: 1.46-8.24), high ΔQFR in the NCS (HR 1.15, 95% CI: 1.10-1.21) and low-post PCI QFR (HR 0.49, 95% CI: 0.39-0.62) were independently associated with TVF. The integration of TCFA and post-PCI QFR into models with traditional cardiac risk factors improved the discrimination ability.
The study provides useful insight into the value of morphofunctional assessment in the residual stenosis of the target vessel and suggests the need for improving the treatment strategy in ACS patients. However, the study did not evaluate non-culprit vessels. Furthermore, the applied models are potentially overfitted because (1) cutoffs for QFR and ΔQFR were derived from the same sample, (2) no cross-validation was performed, and (3) several important clinical and procedural characteristics (e.g., age, sex, post-dilation, residual % diameter stenosis [DS], irregular protrusion, malapposition) were not adjusted for because they were not judged statistically significant during univariate analyses. The overall event numbers are small and thus limit the generalisability of the findings (e.g., n=7-8 in groups with TCFA and QFR <0.88 or ΔQFR>0.046 in non-culprit segments).
The study adds to the accumulating evidence underlying an additive value of functional and morphological assessment of coronary lesions. Artificial intelligence is now applied to enable fast morphofunctional assessment from OCT or merely angiographic images67. It is expected that the diagnostic performance of imaging in the catheterisation laboratory will continue to improve in the coming years and ultimately translate into better patient care.
Conflict of interest statement
S. Tu is the cofounder of, has received research grants from, and has been a consultant for Pulse Medical. J. Westra has no conflicts of interest to declare.