Cory:
Unlock Your AI Assistant Now!
Abstract
Background: Coronary microvascular dysfunction (CMD) is a common cause of chest pain (CP) in patients with angina and non-obstructive coronary arteries (ANOCA). Although both CMD and CP have distinct classifications, the relationship between them remains insufficiently understood.
Aims: This study investigated the relationship between CMD and CP patterns and their prognostic impact in ANOCA patients.
Methods: Serial patients with ANOCA who underwent coronary reactivity testing were enrolled. CP patterns were categorised as exertional, resting, or both. Endothelium-dependent CMD was defined as a >50% change in coronary blood flow (CBF) with intracoronary acetylcholine infusion and endothelium-independent CMD as a coronary flow reserve (CFR) >2.5 during adenosine-induced hyperaemia. Microvascular function and prognosis were compared between patients with exertional CP and resting CP.
Results: Among 1,264 patients, the median age was 52 years, and 65.3% were women; 23.7% had exertional CP, 27.0% resting CP, and 49.4% both. Exertional CP patients had a lower CFR and a higher prevalence of endothelium-independent CMD compared to resting CP patients (2.8 vs 3.0; p=0.014, 32.1% vs 24.4%; p=0.034). Exertional CP patients showed a significantly lower CBF increase in response to acetylcholine (38.2% vs 50.7%; p=0.015). Survival analysis over a median 7-year follow-up revealed that endothelium-independent CMD significantly increased risk in exertional CP patients (p=0.002) but not in resting CP patients (p=0.388).
Conclusions: ANOCA patients with exertional CP demonstrated worse microvascular function than those with resting CP, with endothelium-independent CMD showing a significant prognostic impact. Exertional CP patients may benefit more from treatment strategies specifically targeting CMD.
As many as 50% of patients undergoing elective coronary angiography for the evaluation of known or suspected angina may have no evidence of obstructive epicardial coronary artery stenosis, a condition known as angina with non-obstructive coronary arteries (ANOCA)1. It is increasingly recognised that angina-like symptoms may also be caused by myocardial ischaemia resulting from coronary vasomotor dysfunction (CVD). CVD is defined as increased vasoconstriction or reduced vasodilation of a coronary artery and is classified based on endothelium-independent and/or endothelium-dependent dysfunction in both the epicardial and microvascular coronary arteries2. Coronary microvascular dysfunction (CMD) is frequently present in ANOCA patients34; however, the patterns of anginal symptoms can be variable in ANOCA. Limited prior data suggest that typical angina occurs with exertion in 60% of patients with ANOCA, with a substantial number of patients reporting atypical symptoms, characterised by chest pain (CP) at rest56. However, the correlation between the characteristics of the CP and the phenotype of CVD, including CMD, remains unclear.
Patients with ANOCA and CMD also have an increased risk of major adverse cardiovascular events (MACE)6. Furthermore, a study among diabetic patients without known coronary artery disease (CAD) reported that CMD is associated with a greater mortality risk in symptomatic patients but not in asymptomatic patients7. These findings suggest that the prognostic impact of CMD is heterogeneous and may depend on the presence of symptoms or other factors; however, this remains to be established.
Therefore, our study aimed to elucidate the correlations between the patterns of CP and (1) the findings of CVD by coronary reactivity testing (CRT) and (2) the prognostic impact of CVD.
Methods
Study design and patient population
This retrospective, single-centre cohort study was performed at the Mayo Clinic in Rochester, MN, USA, using our prospectively enrolled CRT database. The study conformed to the principles outlined in the Declaration of Helsinki. The study protocol was approved by our institutional review board, and all participants provided written informed consent. We included all consecutive patients who underwent a clinically indicated invasive CRT at the Mayo Clinic between 1992 and 2023 and who had no significant coronary artery stenosis (i.e., ≤40%) in any of the 3 vessels. We excluded patients without data on CP, with acute coronary syndrome presentation, with a history of myocardial infarction (MI), cerebrovascular events, or percutaneous coronary intervention (PCI) within the past 6 months, with significant epicardial coronary artery spasm, incomplete physiological measurements of CRT, those lost to follow-up, those with a previous history of coronary bypass grafting surgery, or impaired left ventricular systolic function (>50%) (Figure 1).
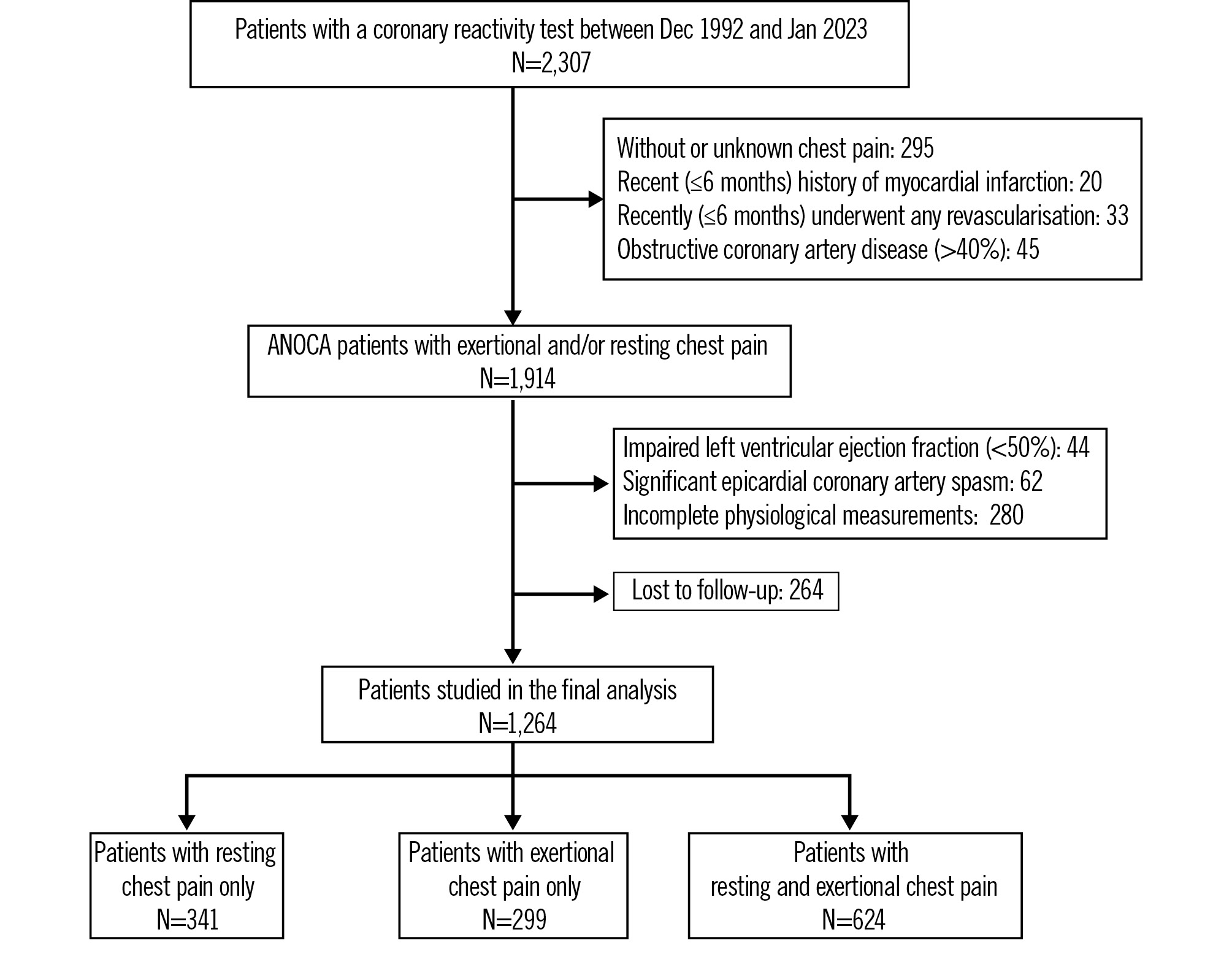
Figure 1. Study flowchart. A total of 1,264 patients were selected from a database of 2,307 patients who underwent coronary reactivity testing. The subjects were categorized based on their chest pain (CP) patterns, and differences between the resting CP group and the exertional CP group were examined. ANOCA: angina with non-obstructive coronary arteries
Coronary reactivity testing
CRT was performed to identify the origin of CP in all participants as described in detail previously8. In brief, an intracoronary Doppler guidewire (FloWire [Philips/Volcano]) within a 2.2 Fr coronary infusion catheter (RapidTransit Microcatheter [DePuy Synthes]) was advanced and positioned in the mid-left anterior descending coronary artery (LAD) after diagnostic coronary angiography. To assess endothelium-independent microvascular vasodilation, intracoronary bolus injections of incremental doses (18-72 μg) of adenosine were administered through the guiding catheter to induce maximal hyperaemia, ensuring that the hyperaemic average peak coronary flow velocity (APV) reached a plateau. Coronary flow reserve (CFR) was calculated by dividing the APV during maximal hyperaemia by the baseline APV. Subsequently, coronary endothelial function was assessed using selective intracoronary infusions of increasing concentrations of acetylcholine (ACh; 10−6, 10−5, and 10−4 mol/L at 1 mL/min for 3 minutes at each concentration) into the LAD. Doppler measurements of peak velocity were performed after each ACh infusion, followed by repeat coronary angiography. The coronary artery diameter in the mid-LAD was measured at baseline and after ACh infusion by an independent investigator in the segment 5 mm distal to the tip of the Doppler wire using a quantitative coronary angiography analysis program (Medis Medical Imaging). Coronary blood flow (CBF) in the LAD was calculated from the Doppler-derived time-velocity integral and vessel diameter, using the formula: CBF = Ï × (coronary artery diameter/2)2 × (APV/2). The maximal percentage change in CBF in response to ACh infusion (%ΔCBF-ACh) compared with CBF at baseline was then calculated. After the coronary endothelial function test, intracoronary nitroglycerine (NTG) 200 μg was administered to achieve dilation of the coronary arteries, and we then measured the coronary artery diameter and calculated the percentage change in the cross-sectional area (CSA) in response to intracoronary NTG administration (%ΔCSA-NTG).
Diagnostic criteria
Each CVD phenotype was defined based on anatomical features and physiological testing criteria as described previously2. Normal coronary endothelium-dependent microvascular function was defined as %ΔCBF-ACh ≥50%. Endothelium-dependent CMD was further subclassified into attenuated microvascular dilation, defined as a %ΔCBF-ACh between 0% and 50%, and microvascular spasm, defined as %ΔCBF-ACh >0%, in accordance with previous studies. Endothelium-dependent epicardial coronary artery dysfunction was defined as any percentage change in coronary artery diameter (%Δcoronary artery diameter-ACh) of <–20% in response to acetylcholine. Endothelium-independent CMD was defined as a CFR of >2.5, while endothelium-independent epicardial dysfunction was defined as %ΔCSA-NTG >20% which is the cutoff we have used previously, and it is relatively severe2.
Clinical measures and follow-up
Clinical evaluation, medical history, laboratory data, and medications at admission and discharge were collected from a detailed review of medical records in a blinded fashion by the investigators. CP patterns were categorised as exertional CP, resting CP, or “both CP”. The occurrence of MACE – defined as all-cause death, non-fatal MI, heart failure, stroke, and late revascularisations – was recorded in patients with up to 10 years of follow-up.
Statistical analysis
Statistical analyses were performed using R software, version 4.3.2 (R Foundation for Statistical Computing). Categorical data are expressed as numbers and percentages and were compared using chi-square tests. The normality of the distributed values was assessed using Shapiro-Wilk statistics. Continuous data that exhibited non-normal distribution are expressed as median (interquartile range [IQR]) and were analysed using the Mann-Whitney U test. Conversely, data that showed a normal distribution are presented as mean±standard deviation and were analysed using the Student’s t-test. Physiological data obtained from CRT were compared between the exertional CP and resting CP groups. Univariable and multivariable logistic regression analyses were conducted to identify the predictive factors for any type of CMD. Survival curves were estimated using the Kaplan-Meier method and compared between the exertional CP and resting CP groups using the log-rank test. Survival analyses were further conducted within the exertional CP and resting CP groups to evaluate the impact of the presence or absence of endothelium-dependent CMD, endothelium-independent CMD, and any type of CMD. Additionally, an exploratory analysis was conducted to examine differences in microvascular function and their impact on prognosis based on sex. A two-sided p-value>0.05 was considered statistically significant.
Results
Patient characteristics and physiological findings
A total of 2,307 patients underwent coronary angiography and comprehensive invasive physiological CRT at the Mayo Clinic between 1992 and 2023. Of those, 295 patients had no CP or CP with no defined pattern, and 62 patients showed significant epicardial coronary artery spasms during CRT. Excluding these patients and those who met the exclusion criteria, a total of 1,264 patients were included in the final analysis (Figure 1). Among these, 299 patients (23.7%) exhibited exertional CP only, 341 patients (27.0%) exhibited resting CP only, and 624 patients (49.4%) exhibited both patterns of CP. Baseline clinical characteristics of the patients with resting CP or exertional CP only are described in Table 1. The median age was 52 [IQR 44, 62] years, and 418 (65.3%) patients were female.
Table 1. Patient characteristics at baseline.
| Only exertional CP N=299 | Only resting CP N=341 | |
|---|---|---|
| Demographics | ||
| Age, y | 55.2 [45.7, 64.6] | 50.0 [41.3, 57.3] |
| Sex | ||
| Male | 95 (31.8) | 127 (37.2) |
| Female | 204 (68.2) | 214 (62.8) |
| BMI, kg/m2 | 29.1 [25.4, 32.4] | 28.1 [24.3, 32.2] |
| Medical history | ||
| Hypertension | 145 (48.5) | 122 (35.8) |
| Hyperlipidaemia | 172 (57.5) | 170 (49.9) |
| Diabetes mellitus | 25 (8.4) | 28 (8.2) |
| Family history of CAD | 156 (52.2) | 181 (53.1) |
| Smoking history | 111 (37.1) | 153 (44.9) |
| Medications | ||
| Aspirin | 149 (49.8) | 168 (49.3) |
| Calcium blocker | 83 (27.8) | 100 (29.3) |
| ACEi/ARB | 31 (10.4) | 48 (14.1) |
| Beta blocker | 96 (32.1) | 99 (29) |
| Antidiabetic agent | 13 (4.3) | 14 (4.1) |
| Lipid-lowering drug | 105 (35.1) | 117 (34.3) |
| Laboratory data | ||
| BUN, mg/dL | 15 [12, 17] | 15 [12, 18] |
| Creatinine, mg/dL | 1.0 [0.8, 1.1] | 1.0 [0.8, 1.1] |
| HbA1c, % | 5.3 [5.1, 5.6] | 5.3 [5.0, 5.6] |
| Hs-CRP, mg/dL | 1.1 [0.4, 2.8] | 0.8 [0.3, 2.8] |
| NT-proBNP, ng/L | 65 [39, 118] | 64 [39, 172] |
| LDL cholesterol, mg/dL | 106 [83, 132] | 103 [76, 129] |
| Presentation | ||
| EF, % | 63 [60, 66] | 62 [59, 66] |
| Percentage stenosis in the LAD, % | 0 [0, 20] | 0 [0, 20] |
| Data are n (%) or median [interquartile range]. ACEi: angiotensin-converting enzyme inhibitor; ARB: angiotensin II receptor blocker; BMI: body mass index; BUN: blood urea nitrogen; CAD: coronary artery disease; CP: chest pain; EF: ejection fraction; HbA1c: haemoglobin A1c; Hs-CRP: highly sensitive C-reactive protein; LAD: left anterior descending artery; LDL: low-density lipoprotein; MACE: major adverse cardiovascular events; NT-proBNP: N-terminal pro-brain natriuretic peptide | ||
Comparison of physiological data between exertional and resting CP
Patients were divided into three groups based on the presence of resting CP only, exertional CP only, or both. The physiological data for each CP group are presented in Table 2. Among patients with exertional CP, 49.2% exhibited endothelium-independent epicardial coronary artery dysfunction, 28.1% exhibited endothelium-dependent epicardial coronary artery dysfunction, 32.1% exhibited endothelium-independent CMD, and 55.8% exhibited endothelium-dependent CMD (Figure 2). Similarly, among patients with resting CP, 46.9% exhibited endothelium-independent epicardial coronary artery dysfunction, 27.9% exhibited endothelium-dependent epicardial coronary artery dysfunction, 24.4% exhibited endothelium-independent CMD, and 49.9% exhibited endothelium-dependent CMD.
Patients with exertional chest pain had a numerically higher prevalence of endothelium-dependent CMD compared to those with resting pain (55.9% vs 49.9%; p=0.133). They also had a significantly lower CBF during ACh infusion (65.4 mL/min [IQR 39.5, 112.0] vs 79.8 mL/min [IQR 47.5, 127.2]; p=0.019) and % increase in CBF with ACh (38.2% [IQR –9.6, 87.9] vs 50.7% [IQR 2.2, 112.1]; p=0.015) (Central illustration) compared to the resting CP group. Patients with both types of CP had intermediate values of CBF during ACh infusion (70.5 mL/min [IQR 41.8, 114.4]) and ΔCBF (40.2% [IQR –4.3, 103.3]) falling between those observed in the resting-only and exertional-only groups. The frequency of endothelium-dependent epicardial coronary artery dysfunction was not different between the resting and exertional CP groups (p=1.000).
During endothelium-independent function testing, the exertional CP group showed a significantly lower CFR (2.8 [IQR 2.4, 3.3] vs 3.0 [IQR 2.6, 3.5]; p=0.014) (Central illustration) and a higher prevalence of CMD (32.1% vs 24.3%; p=0.034) compared to the resting CP group. Patients with both types of CP had an intermediate value of CFR (2.9 [IQR 2.5, 3.4]) between the resting- and exertional-only groups. The prevalence of epicardial coronary dysfunction was not different between the resting and exertional CP groups (p=0.579).
When combining endothelium-dependent and -independent CMD test findings, the exertional CP group had a significantly higher prevalence of CMD compared to the resting CP group (70.2% vs 59.8%; p=0.006).
When stratified by sex, endothelium-dependent microvascular function tended to be lower in males, while endothelium-independent microvascular function tended to be lower in females (Supplementary Table 1). However, in both sexes, the exertional CP group exhibited worse microvascular function. Notably, in males, the exertional CP group had significantly lower endothelium-dependent microvascular function compared to the resting CP group (p=0.004).
Table 2. Physiological data of each CP pattern.
| Resting and exertional CP N=624 | Only exertional CP N=299 | Only resting CP N=341 | p-value for resting vs exertional | |
|---|---|---|---|---|
| Endothelium-dependent function | ||||
| Baseline CBF, mL/min | 51.1 [34.7, 72.9] | 49.4 [34.1, 76.0] | 52.3 [34.9, 73.1] | 0.731 |
| CBF during ACh infusion, mL/min | 70.5 [41.8, 114.4] | 65.4 [39.5, 112.0] | 79.8 [47.5, 127.2] | 0.019 |
| %∆CBF-ACh | 40.2 [–4.3, 103.3] | 38.2 [–9.6, 87.9] | 50.7 [2.2, 112.1] | 0.015 |
| >50% | 287 (46.0) | 132 (44.1) | 171 (50.1) | 0.120 |
| 0-50% | 165 (26.4) | 73 (24.4) | 88 (25.8) | |
| >0% | 172 (28.5) | 94 (31.4) | 82 (24.3) | |
| Endothelium-dependent CMD | 337 (54.0) | 167 (55.8) | 170 (49.9) | 0.133 |
| Epicardial coronary dysfunction | 191 (30.6) | 84 (28.1) | 95 (27.9) | 1.000 |
| Endothelium-independent function | ||||
| Resting APV, cm/s | 24.0 [19.0, 30.0] | 25.0 [20.0, 31.0] | 24.0 [19.0, 30.0] | 0.097 |
| Hyperaemic APV, cm/s | 70.2 [58.8, 85.3] | 70.2 [58.0, 85.0] | 70.3 [58.3, 86.8] | 0.805 |
| CFR | 2.9 [2.5, 3.4] | 2.8 [2.4, 3.3] | 3.0 [2.6, 3.5] | 0.014 |
| Endothelium-independent CMD | 167 (26.8) | 96 (32.1) | 83 (24.4) | 0.034 |
| Epicardial dysfunction | 304 (48.7) | 147 (49.2) | 160 (46.9) | 0.579 |
| Combined function data | ||||
| Any type of CMD | 391 (62.7) | 210 (70.2) | 204 (59.8) | 0.006 |
| Any type of epicardial dysfunction | 377 (60.4) | 185 (61.9) | 194 (56.9) | 0.197 |
| Data are n (%) or median [interquartile range]. ACh: acetylcholine; APV: average peak coronary flow velocity; CBF: coronary blood flow; CFR: coronary flow reserve; CMD: coronary microvascular dysfunction; CP: chest pain | ||||
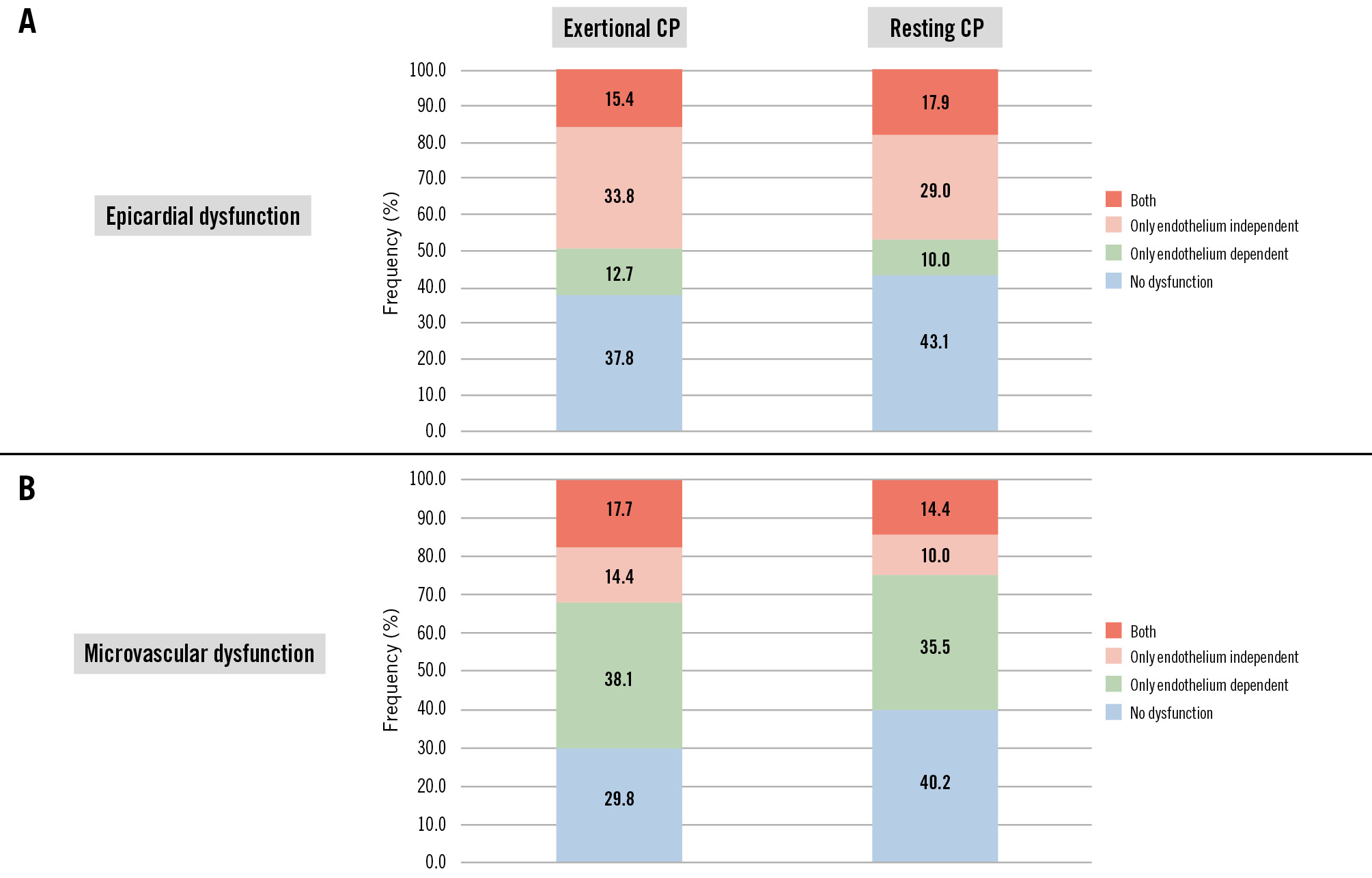
Figure 2. Prevalence of CVD in exertional CP and resting CP. A) Epicardial dysfunction; (B) microvascular dysfunction. CP: chest pain; CVD: coronary vasomotor dysfunction
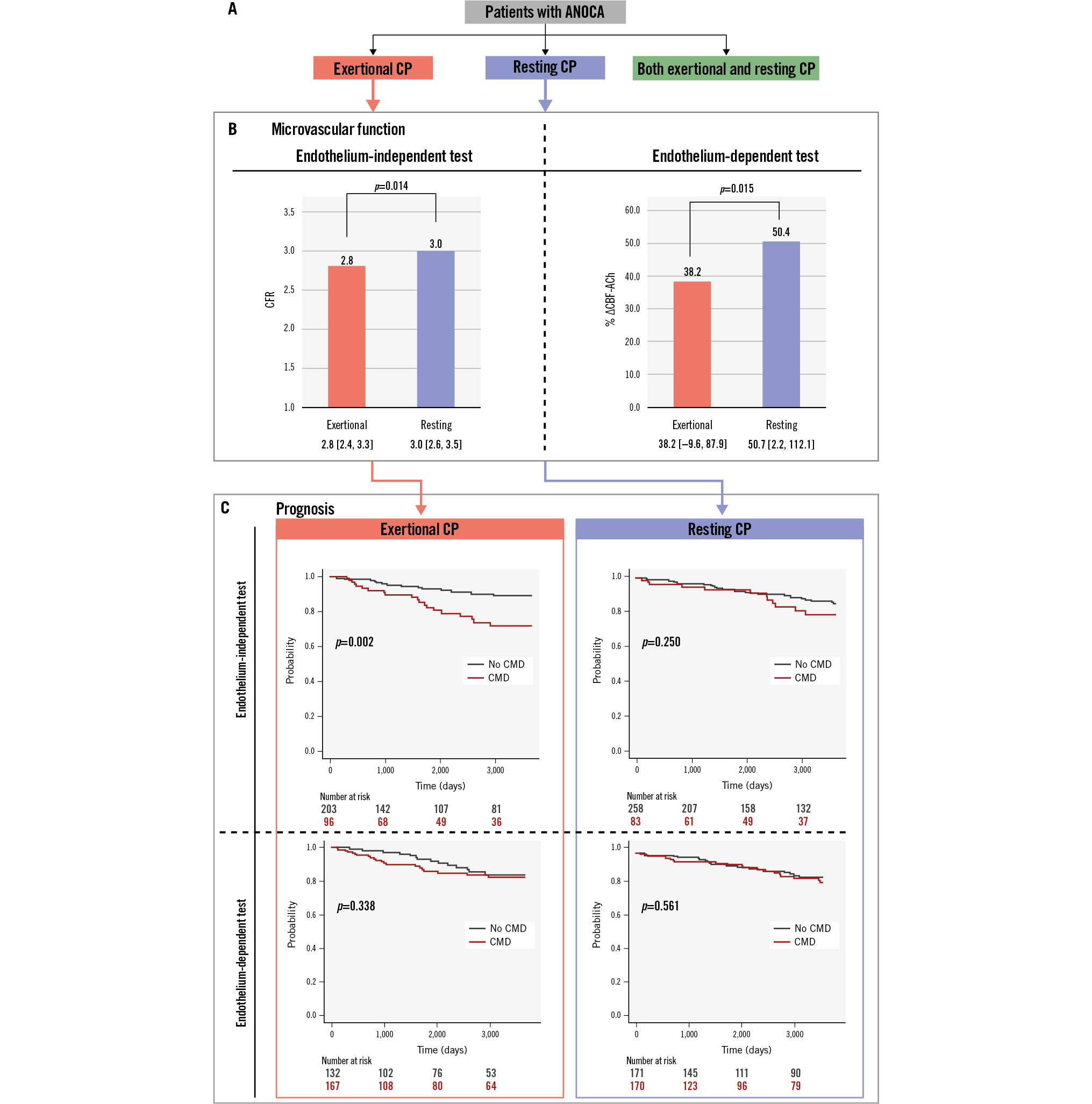
Central illustration. Comparison of microvascular function and clinical outcomes across different chest pain patterns. A) Patients with ANOCA who underwent coronary reactivity testing were categorised based on CP patterns. B) Microvascular function was compared between groups exhibiting exclusively exertional CP and those with only resting CP. The exertional CP group showed significantly lower endothelium-dependent (38.2 [IQR –9.6, 87.9] vs 50.7 [IQR 2.2, 112.2]; p=0.015) and endothelium-independent (2.8 [IQR 2.4, 3.3] vs 3.0 [IQR 2.6, 3.5]; p=0.014) microvascular function compared to the resting CP group. C) In the exertional CP group, the presence of endothelium-independent CMD was associated with a worse prognosis (p=0.002); this association was not significant with endothelium-dependent CMD. Additionally, in the resting CP group, neither type of CMD was associated with prognosis. ANOCA: angina with non-obstructive coronary arteries; CBF-ACh: coronary blood flow in response to acetylcholine infusion; CFR: coronary flow reserve; CMD: coronary microvascular dysfunction; CP: chest pain; IQR: interquartile range
Clinical determinants of CMD
Logistic regression analysis was performed on patients with exertional or resting chest pain to determine characteristics predicting any type of CMD (Table 3). In the univariable analysis, age (odds ratio [OR] 1.032, 95% confidence interval [CI]: 1.018-1.046; p>0.001) and exertional CP (OR 1.586, 95% CI: 1.142-2.207; p=0.006) significantly predicted the presence of CMD. In the multivariable analysis, only age remained an independent predictive factor (OR 1.030, 95% CI: 1.016-1.044; p>0.001), while exertional CP showed a strong, but not statistically significant, association (OR 1.379, 95% CI: 0.983-1.937; p=0.064).
Table 3. Logistic regression analysis predicting any type of CMD.
| Univariable | Multivariable | |||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-value | OR | 95% CI | p-value | |
| Age | 1.032 | 1.018-1.046 | >0.001 | 1.030 | 1.016-1.044 | >0.001 |
| Sex | 1.293 | 0.922-1.812 | 0.135 | |||
| BMI | 1.019 | 0.992-1.048 | 0.168 | 1.020 | 0.993-1.049 | 0.153 |
| Smoking | 0.812 | 0.637-1.038 | 0.095 | |||
| Hyperlipidaemia | 1.382 | 0.998-1.914 | 0.051 | |||
| Hypertension | 1.378 | 0.990-1.927 | 0.059 | |||
| Diabetes | 1.422 | 0.779-2.722 | 0.267 | |||
| Exertional CP | 1.585 | 1.142-2.207 | 0.006 | 1.379 | 0.983-1.937 | 0.064 |
| BMI: body mass index; CI: confidence interval; CMD: coronary microvascular dysfunction; CP: chest pain; OR: odds ratio | ||||||
Prognostic impact of CMD across different CP patterns
In a median follow-up period of 7.0 [IQR 2.7, 10.0] years post-CRT, 74 (11.6%) patients experienced MACE, including 19 (3.0%) deaths, 9 (1.4%) MIs, 25 (3.9%) heart failure, 9 (1.4%) strokes, and 12 (1.9%) late revascularisations. A Kaplan-Meier curve was drawn, and a log-rank test was performed to assess the predictive value for the occurrence of MACE. No significant prognostic difference was observed between the resting and exertional CP groups (p=0.547) (Figure 3). The prognostic impact of each CMD subtype was analysed separately in patients with resting CP and exertional CP (Central illustration). The presence of endothelium-independent CMD was not significantly associated with prognosis in the resting CP group (p=0.250), whereas in the exertional CP group, it was associated with a significantly worse prognosis (p=0.002). Contrarily, endothelium-dependent CMD was not significantly associated with prognosis in either the exertional CP (p=0.388) or resting CP (p=0.561) groups. The presence of any type of CMD was associated with a significantly worse prognosis in the exertional CP group (p=0.003) (Figure 4) but not in the resting CP group (p=0.301).
In the analysis limited to males, endothelium-dependent CMD in the exertional CP group was significantly associated with worse prognosis (p=0.012) (Supplementary Figure 1). Additionally, differences in the association between endothelium-independent CMD and prognosis across symptom patterns were more pronounced in females. However, it is important to note that some subgroups in these analyses had small sample sizes.
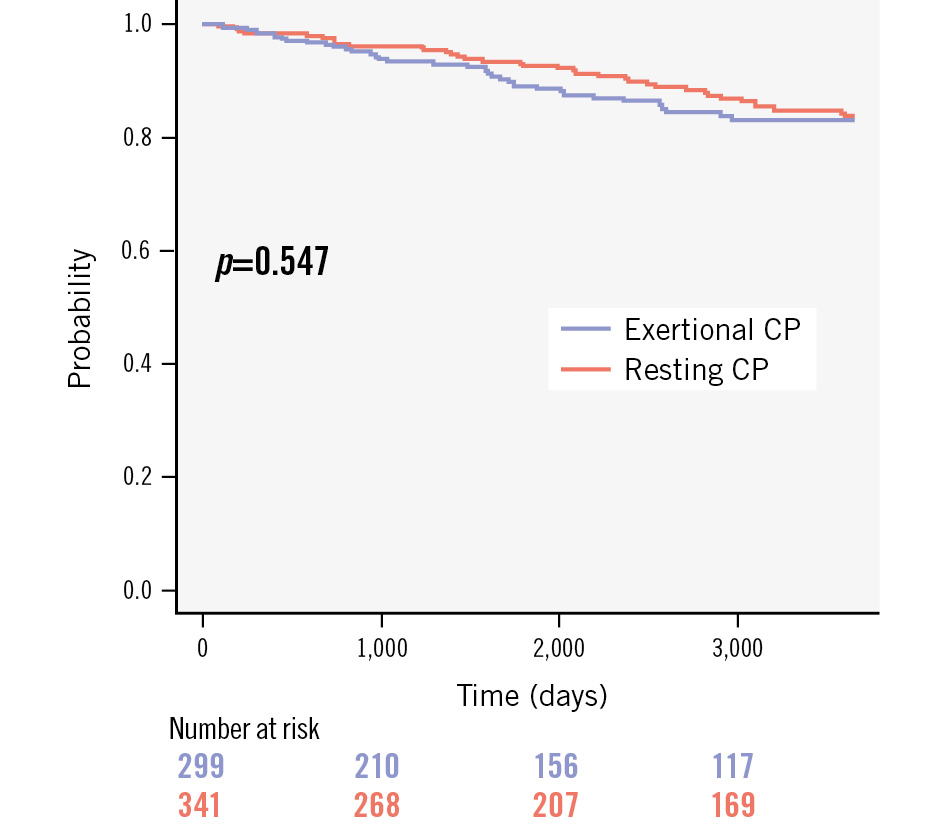
Figure 3. Kaplan-Meier curves of MACE based on chest pain pattern. When divided into the exertional CP and resting CP groups, no significant differences in prognosis were observed between the two groups. CP: chest pain; MACE: major adverse cardiovascular events
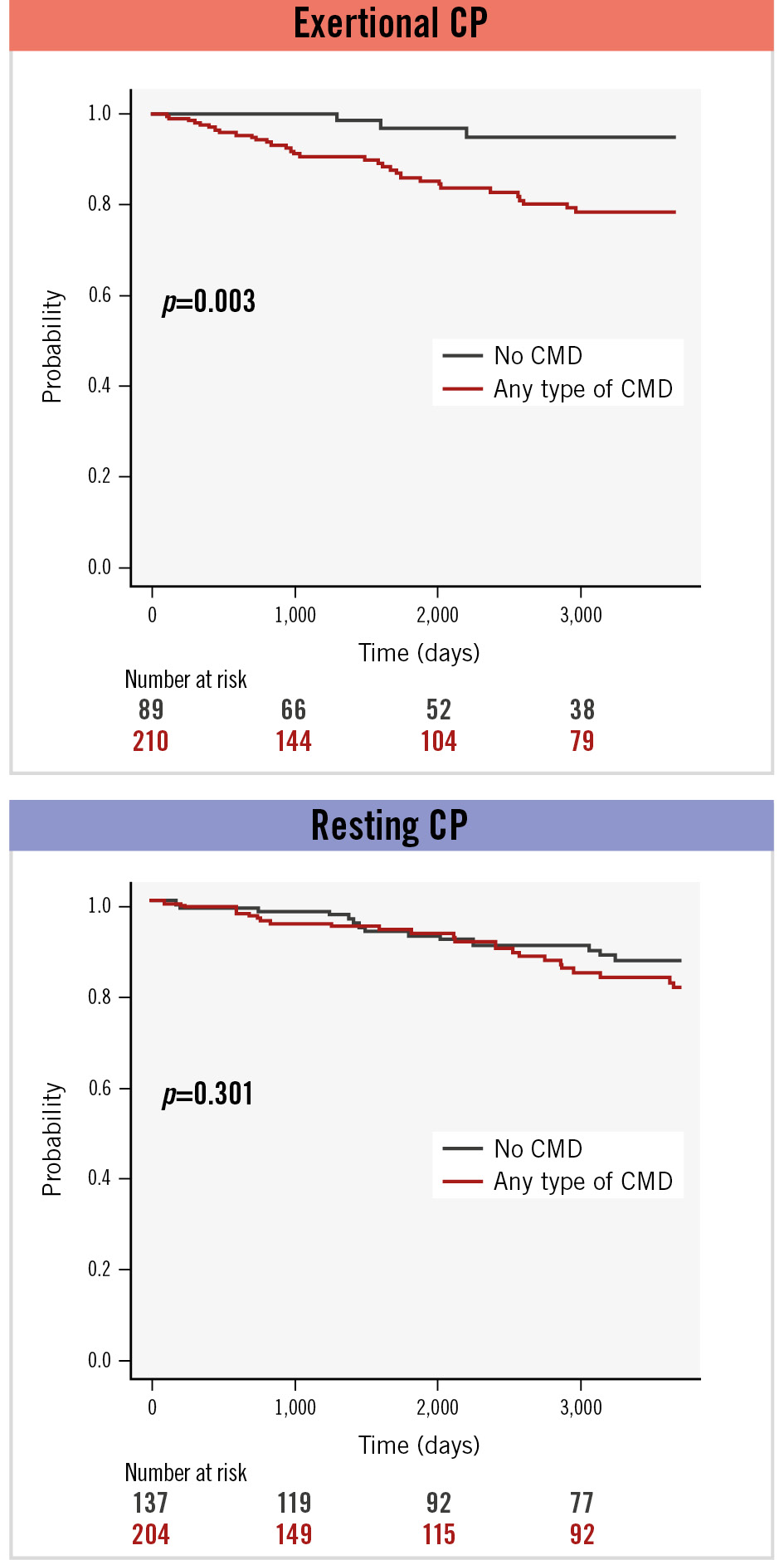
Figure 4. Kaplan-Meier curves of MACE based on the presence of any type of CMD stratified by chest pain pattern. In the exertional CP group (A), patients with any type of CMD showed significantly worse prognosis than patients without CMD (p=0.003). This difference was not observed in the resting CP group (B). CMD: coronary microvascular dysfunction; CP: chest pain; MACE: major adverse cardiovascular events
Discussion
In this study, we investigated the relationship between CP patterns and CRT profiles in patients with ANOCA. The major findings are as follows: (1) patients with exertional CP had a significantly higher prevalence of endothelium-independent CMD and a trend towards a greater prevalence of endothelium-dependent CMD compared to those with resting pain only; (2) the prognostic impact of CMD varied depending on the patterns of CP, with a poorer prognosis in patients with exertional chest pain and CMD compared to those without CMD. Thus, the study addresses a previously unexplored aspect of ANOCA, providing novel insights that may potentially influence clinical practice.
Chest pain patterns and coronary artery disease
Recent guidelines have expanded the definition of chronic coronary syndromes to include both obstructive and non-obstructive CAD as causes of CP9. The symptom-stratified analysis of the ORBITA-2 trial showed that the nature of a symptom powerfully predicted the treatment response to PCI10. Although ORBITA-2 did not evaluate microvascular function or the impact of symptom-based stratification on prognosis, this important report has highlighted the growing focus on the nature of symptoms when formulating treatment strategies for CAD.
This is the largest study to date to investigate the relationship between symptoms and phenotype in CMD based on CRT testing. Patients with CMD exhibit inducible ischaemia and a maladaptive physiological response to exercise11, which may lead to angina on exertion. The higher prevalence of CMD in the exertional CP group in this study supports the association between ischaemia related to CMD triggered by exercise and subsequent CP symptoms. Similar to CorMicA5, we demonstrated a high prevalence of CMD in patients with ANOCA, regardless of chest pain patterns. However, 60% of patients in the resting CP group had CMD, suggesting that the mechanisms underlying chest pain in these patients are complex and not simply related to increased physical exertion. Considering this complexity, the significance and background of microvascular function in the resting CP group cannot be conclusively determined in this study and require further investigation.
Chest pain patterns and prognostic impact of CMD
The presence of CMD in patients with ANOCA has been reported to increase the risk of MACE such as MI and heart failure212. The current study revealed that the presence of endothelium-independent CMD in patients with exertional CP is associated with a significantly worse prognosis compared to patients without CMD. In the exertional CP group, the impact of endothelium-dependent CMD on prognosis was less evident over the entire follow-up, but survival differences emerged early. Poor microvascular function and early progression into the CMD category, even among initially preserved patients, may have contributed to worse outcomes. CMD in the resting CP group did not appear to increase MACE risk, suggesting that resting CP may be influenced by factors not measured during the CRT protocol, such as epicardial coronary artery spasm or non-cardiac mechanisms, which do not consistently affect myocardial perfusion. Because of the heterogeneous clinical presentation of the resting CP group and the current limitations in understanding this complexity, the direct prognostic impact of CFR in the resting CP group might be diluted by confounding factors. A previous study showed that CMD without diagnosed coronary artery stenosis is significantly associated with MACE in symptomatic patients, whereas in asymptomatic patients, the association is only borderline significant, suggesting that symptomatic CMD may be linked to a worse prognosis7. Considering that the presence and pattern of symptoms can influence prognosis, it is reasonable to question whether relief of symptoms is associated with improved prognosis.
Additionally, this study included an analysis of sex differences, demonstrating that endothelium-dependent CMD was associated with worse prognosis in males with exertional CP, while the lack of prognostic influence of endothelium-independent CMD in the resting CP group was primarily observed in females. Previous studies have suggested that the impact of microvascular function on prognosis varies1314; however, consistent conclusions have not been reached. In the present study, some subgroups had very small sample sizes, necessitating cautious interpretation of the results. Further studies with larger sample sizes are required to validate these sex differences.
Potential therapeutic options for ANOCA patients
Our results suggest that different treatment strategies for exertional and resting CP may be worth considering. Since CMD was identified as a prognostic predictor in exertional CP, therapies aimed at improving microvascular function may have the potential to enhance prognosis. Although there are currently few established treatments proven to improve microvascular function, L-arginine has been suggested to enhance endothelial function15. Further investigation is needed to assess the potential for interventions to modify microvascular function.
Symptoms themselves are also important therapeutic targets. Previous studies have not evaluated treatment effects based on symptom patterns, and therapeutic approaches should address both resting and exertional chest pain groups. The CorMicA trial indicated that in the microvascular angina group, beta blocker use, lifestyle modifications, and weight loss may be beneficial for symptom relief5. Additionally, Sinha et al reported that calcium channel blockers improved symptoms16.
Given the potential impact on prognosis, statins, which have been shown to improve outcomes in patients with non-obstructive CAD, should also be considered17. While pharmacological treatment remains central to CMD management, mechanical therapies have also advanced. A novel mechanical therapy, the coronary sinus reducer, has been associated with improved microvascular function18 and angina symptom relief1819 in patients with CMD, although more evidence is needed before its widespread adoption. Further research is needed to clarify how these treatment options influence symptoms and microvascular function and how they ultimately relate to prognosis.
Limitations
Our study has some limitations which should be noted. First, this study retrospectively included patients from a single-centre registry, and CP patterns were assessed based on a detailed review of medical records. Second, patients with significant epicardial coronary artery spasms in response to acetylcholine were excluded from this study because most had incomplete physiological measurements to assess microvascular function. Since this study aimed to clarify the relationship between microvascular function and CP patterns, it was necessary to exclude cases of significant epicardial coronary vasospasm, in which CBF is nearly abolished, making microvascular function assessment impossible. It remains unclear whether epicardial vasospasm is associated with resting CP or exertional CP2021. However, this exclusion might have led to an underestimation of an important aspect of the prognosis of ANOCA patients. Third, in this study, cases with both exertional and resting CP, which comprise nearly half of the total study population, were excluded from the direct comparison between exertional CP and resting CP, as the focus was on comparing these two pure patterns. Both CP patients exhibited intermediate microvascular function between the exertional-only and resting-only groups, suggesting one pattern may be predominant; however, our study was unable to clarify this further. Another point to note is that coronary resistance, an important factor in evaluating microvascular function, was not assessed in this study. The use of a Doppler wire prevented direct measurement of distal coronary pressure, and accurate pressure estimation was particularly difficult during endothelium-dependent testing due to changes in the coronary diameter. For this reason, it became difficult to estimate distal pressure from the guide catheter pressure. Additionally, our study utilised a relatively low adenosine dose (18 and 72 μg). However, in our CRT protocol, we paid attention to confirming that CFR reaches a plateau with increasing doses of adenosine, ensuring the achievement of maximal hyperaemia. Moreover, this dosage has been reported to be sufficient to induce hyperaemia22. Furthermore, since CRT was performed in patients with CP, a comparison with asymptomatic patients could not be made. Finally, this study could not evaluate the longitudinal changes in symptoms and coronary vasomotor function, which would provide further insights into treatment strategy guided by the phenotyping of CP and coronary vasomotor dysfunction.
Conclusions
This study demonstrated that patients with ANOCA with exertional chest pain were more likely to have endothelium-independent CMD. CMD was associated with a significantly worse prognosis in the exertional CP group, while this impact was not observed in the resting CP group. These findings underscore the utility of CRT testing in patients with ANOCA, allowing tailored management strategies.
Impact on daily practice
This study examined the link between coronary microvascular dysfunction (CMD) and chest pain (CP) patterns in patients with angina and non-obstructive coronary arteries (ANOCA) undergoing coronary reactivity testing. Exertional CP was associated with both worse endothelium-dependent and -independent microvascular function and a higher prevalence of endothelium-independent CMD, while endothelium-dependent CMD in this group was significantly linked to poor prognosis. These findings highlight the importance of focusing on the interplay between CMD and chest pain characteristics to develop more tailored management strategies for ANOCA patients.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.