Abstract
BACKGROUND: Intracoronary continuous thermodilution is a novel technique to quantify absolute true coronary flow and microvascular resistance. However, few data are available in patients with angina with non-obstructive coronary arteries (ANOCA).
AIMS: This study aimed to investigate the diagnostic potential of hyperaemic absolute coronary flow (Qmax) and absolute microvascular resistance (Rμ,hyper) among different ANOCA endotypes, and to determine the correlation between continuous – and bolus – thermodilution indexes.
METHODS: A total of 222 patients were scheduled for clinically indicated coronary function testing (CFT), of whom 120 patients were included in this analysis. These patients underwent CFT including acetylcholine (ACh) provocation testing and microvascular function assessment using both bolus and continuous thermodilution.
RESULTS: CFT was negative (CFT−) in 32 (26.7%) patients. Endothelium-dependent dysfunction (ACh+) was present in 63 (52.5%) patients, and coronary microvascular dysfunction (CMD) identified at bolus thermodilution (CMD+) was present in 62 (51.7%) patients. Patients with a positive CFT (CFT+) showed significantly lower Qmax and higher Rμ,hyper values as compared to CFT−. Qmax was significantly lower in CMD+ versus CMD− patients (0.174 vs 0.222 L/min; p=0.04) but did not differ in patients with or without a positive ACh test (0.198 vs 0.219 L/min; p=0.86).
CONCLUSIONS: The prevalence of a CFT+ is high in a selected ANOCA population. In our study, Qmax and Rμ,hyper were associated with a positive CFT. Qmax was associated with the presence of microvascular dysfunction but not with a positive acetylcholine test. The novel continuous thermodilution method can provide further insights into ANOCA endotypes.
Angina or ischaemia with non-obstructive coronary arteries (ANOCA/INOCA) can be found in up to 25% of patients with chest pain undergoing coronary angiography123.
The pathogenesis of ANOCA relies on two distinctive mechanisms (alone or in combination) which subsequently define different endotypes: coronary microvascular dysfunction (CMD) and epicardial/microvascular spasm. CMD is the consequence of structural microcirculatory remodelling, while epicardial or microvascular spasm is caused by vasomotor dysregulation and enhanced vessel reactivity4567.
Clinical manifestations of ANOCA comprise a wide range of symptoms which are often misdiagnosed and under- or mistreated89.
The direct assessment of coronary microcirculatory responses to vasodilatory stimuli and the assessment of vasomotor disorders are pivotal to implement stratified medicine, which leads to a reduction in angina severity and better quality of life as compared with standard care1.
Invasive coronary function testing (CFT) is currently the only diagnostic option which allows a definitive diagnosis of microvascular disorders along with characterisation of different endotypes, as recommended by current consensus guidelines1011.
The administration of vasoreactivity-inducing stimuli investigates the endothelium-dependent mechanisms of microvascular and epicardial vasomotor tone disorders12. Endothelium-independent mechanisms of CMD can be assessed using bolus thermodilution or Doppler guidewire testing13.
However, technical challenges in acquiring a stable Doppler signal as well as the need for adenosine-induced hyperaemia for bolus thermodilution limit the widespread adoption of these diagnostic tools14. The diagnostic process can be implemented by using a novel technology which allows the measurement of true coronary flow and microvascular resistance15. Continuous thermodilution assessment of the microcirculation has been proven to be safe and reproducible and correlates with the gold standard, positron emission tomography16.
The aim of this study was to investigate the diagnostic potential of absolute flow and microvascular resistance among different ANOCA endotypes and to assess the correlation between these continuous thermodilution-derived variables and standard physiological indices as assessed by bolus thermodilution. We further defined a continuous thermodilution-derived range of values able to predict CMD, as diagnosed by bolus thermodilution.
Methods
STUDY DESIGN
This was a single-centre, prospective observational registry conducted at Maasstad Hospital, the Netherlands, which is a large tertiary referral centre specialising in patients with ANOCA. The study protocol conforms to the International Conference on Harmonisation/Good Clinical Practice standards and the Declaration of Helsinki. All patients gave written informed consent.
Clinical characteristics including medical history, risk factors and symptoms were obtained from both the electronic patient file and an online patient questionnaire. The data were stored and pseudonymised in an online database (Castor EDC) and were only accessible to the involved researchers.
STUDY POPULATION
The study population included all consecutive suspected ANOCA patients referred to our centre for CFT from January 2019 to February 2023. Eligible patients were selected from the outpatient clinic of the cardiology department of the enrolling centre. Only patients presenting with chronic angina − defined as having symptoms of angina at least 2 times a week despite medical therapy for 3 months − were included in the final analysis.
Obstructive coronary artery disease (CAD) was ruled out before CFT by anatomical imaging via coronary angiography (CAG) or coronary computed tomography angiography (CCTA) or via non-invasive ischaemia detection.
Exclusion criteria were patterns of anginal symptoms other than those defined as chronic angina, contraindication to adenosine (e.g., asthma, bronchospasm, conduction disorders), significant valve disease, acute coronary syndrome presentation, left ventricular dysfunction (left ventricular ejection fraction <30%), and the inability or unwillingness to give informed consent.
A description of the CFT can be found in Supplementary Appendix 1.
ENDOTYPES DEFINITION
We defined the endotypes according to the underlying pathophysiological mechanisms in patients with or without coronary spasm, as assessed with acetylcholine (ACh) vasoreactivity testing (ACh+/−), and patients with or without CMD, as measured by the bolus thermodilution method (CMD+/−) (Figure 1).
The definitions of epicardial or microvascular spasm were based on contemporary international criteria as follows and are displayed in Table 1. According to the Coronary Vasomotor Disorders International Study Group (COVADIS) criteria, the ACh vasoreactivity testing was defined as abnormal in case of recognisable symptoms and ischaemic electrocardiogram (ECG) changes (i.e., ST-segment depression or ST-segment elevation of ≥0.1 mV or T-wave peaking in at least 2 contiguous leads) with either epicardial or microvascular spasm1217. Epicardial coronary diameter reduction ≥90%, either focal or diffuse, in response to ACh administration was defined as vasospastic angina (VSA)12. Microvascular spasm was diagnosed in the absence of ≥90% epicardial diameter reduction during ACh infusion18. Any inconclusive result in response to ACh administration (e.g., recognisable symptoms without ECG modifications) was considered negative.
CMD was defined as the presence of an index of microvascular resistance (IMR) ≥25 and/or a coronary flow reserve (CFR) <2.5 measured with bolus thermodilution11. CMD was further classified as structural CMD − defined as an IMR ≥25 and CFR <2.5 − and functional CMD − defined as a CFR <2.5 with a normal IMR19.
A positive CFT was defined by a positive response to ACh vasoreactivity testing or the presence of CMD or both.
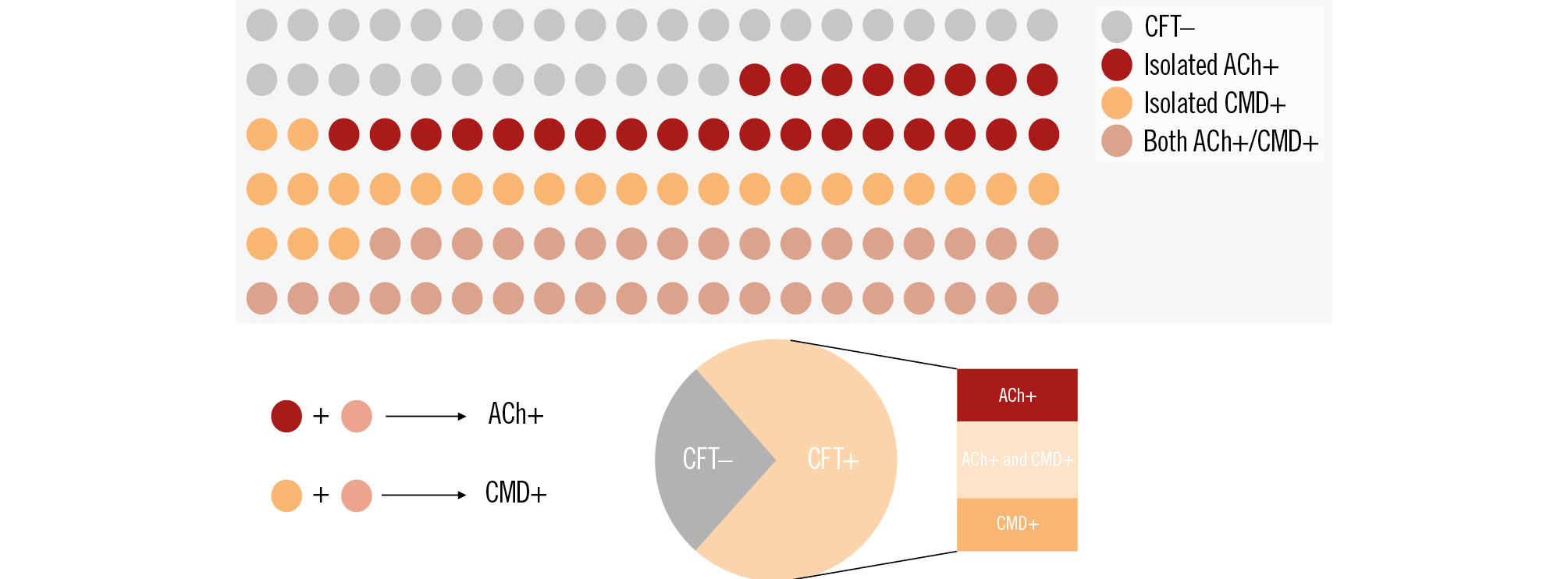
Figure 1. Prevalence of ANOCA endotypes. ACh+: patients with coronary spasm; ANOCA: angina with non-obstructive coronary arteries; CFT: coronary function testing; CMD: coronary microvascular dysfunction
Table 1. ANOCA endotype definitions.
| Bolus thermodilution | Spasm provocation results | |
|---|---|---|
| Vasospastic angina | Angina, ischaemic ECG changes, and ≥90% luminal reduction | |
| Microvascular angina | Angina, ischaemic ECG changes, but no or <90% luminal reduction | |
| CMD | CFR <2.5 and/or IMR ≥25 | |
| ANOCA: angina with non-obstructive coronary arteries; CFR: coronary flow reserve; CMD: coronary microvascular dysfunction; ECG: electrocardiogram; IMR: index of microvascular resistance | ||
STATISTICAL ANALYSIS
In this study, the continuous thermodilution parameters (hyperaemic absolute coronary flow [Qmax] and absolute microvascular resistance [Rμ,hyper]) were compared in different groups of patients CFT (+/−), CMD (+/−) and ACh (+/−), and in patients with isolated CMD+ or isolated ACh+. Normally distributed continuous variables are expressed as mean±standard deviation (SD), and categorical variables are displayed as number and percentage. Differences between groups were assessed by an unpaired Student’s t-test for continuous data with a normal distribution. Otherwise, the non-parametric Mann-Whitney U test was used as appropriate. All p-values<0.05 were considered statistically significant. We used SPSS Statistics, version 29.0 (IBM) for all statistical analysis.
Results
CLINICAL CHARACTERISTICS
A total of 222 patients were scheduled for clinically indicated CFT, of whom 120 patients were included in this analysis. Reasons for exclusion were no informed consent (n=38), obstructive CAD with percutaneous coronary intervention (PCI) performed (n=5), fractional flow reserve ≤0.80 in the left anterior descending artery (n=20), clinical presentation other than chronic angina as described above (n=29), or missing parameters (n=10). Baseline and procedural characteristics are displayed in Table 2 and Table 3. Non-invasive ischaemia detection was performed in 38 (31.6%) patients, of whom 26 (21.6%) underwent exercise testing and 12 (10.0%) underwent imaging stress testing. Medications at baseline and after CFT are displayed in Table 4.
Table 2. Baseline characteristics across the whole cohort and according to ANOCA endotypes.
| All patients (n=120) | CFT−(n=32) | CFT+(n=88) | p-value | CMD−(n=58) | CMD+(n=62) | p-value | ACh−(n=57) | ACh+(n=63) | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Age, years | 59.2±10.4 | 57.5±11.5 | 59.2±11.7 | 0.25 | 57.1±11.3 | 60.2±11.7 | 0.07 | 58.3±10.3 | 59.1±12.8 | 0.69 |
| Female | 89 (74.2) | 28 (87.5) | 63 (71.6) | 0.07 | 49 (84.5) | 42 (67.7) | 0.03 | 45 (78.9) | 46 (73.0) | 0.44 |
| BMI, kg/m2 | 27.8±4.8 | 28.3±5.6 | 27.6±4.5 | 0.30 | 27.7±4.6 | 27.8±4.9 | 0.43 | 27.5±5.05 | 28.1±4.54 | 0.58 |
| History of diabetes | 17 (14.2) | 3 (9.4) | 14 (16.3) | 0.34 | 9 (15.8) | 8 (12.9) | 0.68 | 5 (8.7) | 12 (19.6) | 0.09 |
| History of hypertension | 66 (55.0) | 19 (59.4) | 47 (54.7) | 0.64 | 29 (50.9) | 37 (60.7) | 0.28 | 34 (59.6) | 32 (52.4) | 0.43 |
| History of hyperlipidaemia | 54 (44.9) | 16 (50.0) | 36 (41.9) | 0.43 | 23 (40.4) | 29 (55.8) | 0.43 | 27 (47.3) | 25 (40.9) | 0.48 |
| Smoking status | ||||||||||
| Never | 69 (57.3) | 22 (68.8) | 45 (52.9) | 36 (63.2) | 31 (51.7) | 36 (63.1) | 31 (51.6) | |||
| Former | 24 (20.0) | 8 (25.0) | 18 (21.2) | 0.06 | 13 (22.8) | 13 (21.7) | 0.22 | 12 (21.0) | 14 (23.3) | 0.09 |
| Current | 27 (22.7) | 2 (6.3) | 22 (25.9) | 8 (14.0) | 16 (25.8) | 9 (15.7) | 15 (25.0) | |||
| COPD | 3 (2.5) | 0 (0) | 3 (6.0) | 0.28 | 2 (2.9) | 1 (1.5) | 0.42 | 3 (5.2) | 3 (4.7) | |
| History of AMI | 22 (18.3) | 7 (21.9) | 15 (17.4) | 0.58 | 9 (15.8) | 13 (21.3) | 0.44 | 10 (17.5) | 12 (19.6) | 0.76 |
| Autoimmune disease | 12 (10.0) | 1 (3.0) | 11 (12.5) | 0.13 | 4 (6.9) | 8 (12.9) | 0.27 | 3 (5.2) | 9 (14.2) | 0.10 |
| Prior CAG | 76 (63.3) | 20 (62.5) | 56 (64.4) | 0.85 | 35 (61.4) | 41 (66.1) | 0.59 | 35 (61.4) | 41 (66.1) | 0.59 |
| Prior coronary CTA | 32 (26.7) | 11 (34.4) | 21 (23.9) | 0.25 | 16 (27.6) | 16 (25.8) | 0.82 | 17 (29.8) | 15 (23.8) | 0.46 |
| Prior non-invasive ischaemia detection | 38 (31.6) | 9 (28.1) | 29 (32.9) | 0.78 | 20 (28.5) | 21 (33.3) | 0.25 | 16 (28.0) | 22 (34.9) | 0.43 |
| Exercise stress testing | 26 (21.6) | 6 (18.7) | 20 (22.7) | 14 (20.0) | 12 (24.0) | 12 (21.0) | 14 (22.2) | |||
| Imaging stress testing | 12 (10.0) | 3 (9.4) | 9 (10.2) | 6 (8.6) | 6 (12.0) | 4 (7.0) | 8 (12.7) | |||
| Data are given as mean±standard deviation or n (%). ACh: acetylcholine; ACh+: patients with coronary spasm; ACh−: patients without coronary spasm; AMI: acute myocardial infarction; ANOCA: angina with non-obstructive coronary arteries; BMI: body mass index; CAG: coronary angiography; CFT: coronary function testing; CMD: coronary microvascular dysfunction; COPD: chronic obstructive pulmonary disease; CTA: computed tomography angiography | ||||||||||
Table 3. Haemodynamic parameters across the whole cohort and according to ANOCA endotypes.
| All patients (n=120) | CFT−(n=32) | CFT+(n=88) | p-value | CMD−(n=58) | CMD+(n=62) | p-value | ACh−(n=57) | ACh+(n=63) | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Pd/Pa | 0.92±0.02 | 0.93±0.03 | 0.93±0.02 | 0.26 | 0.93±0.02 | 0.92±0.03 | 0.16 | 0.92±0.02 | 0.92±0.02 | 0.39 |
| LAD FFR | 0.88±0.04 | 0.89±0.05 | 0.88±0.04 | 0.12 | 0.88±0.05 | 0.88±0.04 | 0.14 | 0.88±0.05 | 0.88±0.04 | 0.84 |
| LAD CFR | 3.57±1.84 | 4.79±2.25 | 3.13±1.44 | <0.01 | 4.66±1.99 | 2.54±0.99 | <0.01 | 3.81±2.11 | 3.35±1.54 | 0.16 |
| LAD CFR norm | 3.70±1.58 | 4.86±2.37 | 3.34±1.61 | 0.05 | 4.32±1.64 | 2.89±1.08 | <0.01 | 3.72±1.59 | 3.68±1.59 | 0.93 |
| LAD IMR | 28.77±19.90 | 13.78±5.90 | 31.77±18.63 | <0.01 | 15.96±5.39 | 38.94±21.36 | <0.01 | 24.72±18.55 | 33.05±20.64 | 0.08 |
| LAD IMR norm | 26.97±18.08 | 15.05±6.00 | 33.52±20.84 | <0.01 | 15.41±5.67 | 37.79±19.01 | <0.01 | 21.89±16.18 | 31.57±18.58 | <0.01 |
| LAD Qmax, L/min | 0.157±0.06 | 0.233±0.08 | 0.188±0.06 | 0.04 | 0.222±0.10 | 0.174±0.10 | 0.04 | 0.219±0.09 | 0.198±0.11 | 0.86 |
| LAD Rµ,hyper, WU | 485.0±196.7 | 469.4±176.5 | 552.7±199.5 | 0.02 | 492.1±180.4 | 566.4±204.5 | 0.02 | 466.6±172.4 | 588.3±200.2 | <0.01 |
| Data are given as mean±standard deviation. ACh: acetylcholine; ACh+: patients with coronary spasm; ACh−: patients without coronary spasm; ANOCA: angina with non-obstructive coronary arteries; CFR: coronary flow reserve; CFT: coronary function testing; CMD: coronary microvascular dysfunction; FFR: fractional flow reserve; IMR: index of microvascular resistance; LAD: left anterior descending artery; Pa: aortic pressure; Pd: distal coronary pressure; Qmax: hyperaemic absolute coronary blood flow; Rµ,hyper: hyperaemic absolute microvascular resistance; WU: Wood units | ||||||||||
Table 4. Medications at baseline and after CFT across the whole cohort and according to ANOCA endotypes.
| All patients (n=120) | CFT−(n=32) | CFT+(n=88) | p-value | CMD−(n=58) | CMD+(n=62) | p-value | ACh−(n=57) | ACh+(n=63) | p-value | |
|---|---|---|---|---|---|---|---|---|---|---|
| Medications pre-CFT | ||||||||||
| Beta blockers | 42 (35.0) | 13 (40.6) | 29 (32.9) | 0.43 | 23 (39.7) | 19 (30.6) | 0.30 | 22 (38.5) | 20 (74.2) | 0.43 |
| Calcium channel blockers | 50 (41.7) | 12 (37.5) | 38 (43.2) | 0.57 | 22 (37.9) | 28 (56.0) | 0.42 | 22 (38.5) | 28 (44.4) | 0.52 |
| ACEi/ARBs | 55 (45.8) | 15 (46.9) | 40 (45.5) | 0.89 | 24 (41.4) | 31 (50.0) | 0.34 | 29 (50.8) | 26 (41.2) | 0.29 |
| Statins | 68 (56.7) | 18 (56.3) | 50 (56.8) | 0.96 | 30 (51.7) | 38 (61.3) | 0.29 | 30 (52.6) | 38 (60.3) | 0.39 |
| Long-acting nitrates | 35 (29.2) | 6 (18.8) | 29 (33.0) | 0.13 | 14 (24.1) | 21 (33.9) | 0.24 | 17 (29.8) | 18 (28.5) | 0.88 |
| Medications post-CFT | ||||||||||
| Beta blockers | 43 (35.8) | 13 (40.6) | 30 (34.1) | 0.51 | 28 (48.3) | 15 (24.0) | 0.04 | 23 (40.3) | 20 (31.7) | 0.32 |
| Calcium channel blockers | 104 (86.7) | 24 (75.0) | 80 (90.9) | 0.02 | 48 (84.2) | 52 (93.6) | 0.02 | 45 (78.9) | 59 (93.6) | 0.02 |
| ACEi/ARBs | 55 (45.8) | 15 (46.9) | 40 (45.5) | 0.89 | 28 (48.3) | 27 (42.8) | 0.44 | 29 (50.8) | 26 (41.2) | 0.29 |
| Statins | 67 (55.8) | 18 (56.3) | 49 (55.7) | 0.96 | 30 (51.7) | 37 (59.7) | 0.38 | 30 (52.6) | 37 (58.7) | 0.50 |
| Long-acting nitrates | 42 (35.0) | 6 (18.8) | 36 (40.9) | 0.02 | 18 (31.0) | 24 (38.7) | 0.38 | 15 (26.3) | 27 (42.8) | 0.06 |
| Data are presented as n (%). ACEi: angiotensin-converting enzyme inhibitors; ACh: acetylcholine; ACh+: patients with coronary spasm; ACh−: patients without coronary spasm; ANOCA: angina with non-obstructive coronary arteries; ARBs: angiotensin II receptor blockers; CFT: coronary function testing; CMD: coronary microvascular dysfunction | ||||||||||
PREVALENCE OF ENDOTYPES
Coronary function testing was negative in 32 (26.7%) patients.
Endothelium-dependent dysfunction (ACh+) was present in 63 (52.5%) patients, of whom 21 presented with VSA. In VSA patients, epicardial vasospasm >90% was diagnosed in 14 patients using a third injection of ACh (at a reduced dose of 100 μg) and in 7 patients with a third injection at the maximum dose of ACh (200 μg). Non-endothelium-dependent microvascular dysfunction identified at bolus thermodilution (CMD+) was present in 62 (51.7%) patients, of whom 35 presented with IMR ≥25 and normal CFR, 10 with CFR <2.5 and normal IMR, and 17 with both abnormal CFR and IMR.
The coexistence of both ACh+ and CMD+ endotypes was detected in 37 (30.8%) patients, while isolated ACh+ and CMD+ was present in 26 (21.7%) and 25 (20.8%) patients, respectively.
SAFETY
Procedural complications were evaluated in all patients included in the analysis.
No fatal or serious adverse complications (e.g., coronary intervention, ventricular or atrial fibrillation, myocardial infarction, persistent ventricular tachycardia, sinus arrest) were observed. In 2 patients, a Type 1 Bleeding Academic Research Consortium bleeding occurred, which did not require further treatment. Eleven patients developed a transient atrioventricular (AV) block during the ACh provocation test, which is a frequent side effect of intracoronary ACh administration20. In all these patients, the AV block was resolved within seconds by stopping the infusion of ACh. The ACh provocation test was then continued, with the injection of ACh at a lower rate. No patients required the administration of intravenous atropine.
ABSOLUTE FLOW AND RESISTANCE ACROSS DIFFERENT ENDOTYPES
Patients exhibiting either a positive response to ACh and/or CMD (CFT+) demonstrated significantly lower Qmax and higher Rμ,hyper values compared to CFT− patients (0.188 vs 0.233 L/min; p=0.04; and 552.7 vs 469.4 Wood units [WU]; p=0.02, respectively).
Patients with a positive response to acetylcholine (ACh+) exhibited no difference in terms of Qmax (0.198 vs 0.219 L/min; p=0.86) but showed significantly higher Rμ,hyper (588.3 vs 466.6 WU; p<0.01) than ACh− patients (Central illustration). Comparisons between patients with isolated positive responses to acetylcholine (ACh+) and the rest of the group revealed no differences in terms of Qmax or Rμ,hyper (0.207 vs 0.208 L/min; p=0.49; and 533.4 vs 520.1 WU; p=0.38, respectively), as depicted in Figure 2A and Figure 2B.
Patients diagnosed with microvascular dysfunction (CMD+) displayed significantly lower Qmax and significantly higher Rμ,hyper values compared to CMD− patients (0.174 vs 0.222 L/min; p=0.04; and 566.4 vs 492.1 WU; p=0.02, respectively), as depicted in the Central illustration.
Similarly, when patients with isolated CMD (CMD+) were compared to the remainder of the group, Qmax was significantly lower and Rμ,hyper was significantly higher (0.157 vs 0.208 L/min/m2; p=0.03; and 548.3 vs 463.1 WU; p=0.03, respectively), as shown in Figure 2C and Figure 2D.
Further classification of CMD revealed significantly decreased Qmax and increased Rμ,hyper in patients with structural CMD compared to patients without structural CMD (0.194 vs 0.212 L/min; p=0.04 and 611.9 vs 500.9 WU; p<0.01, respectively), as depicted in Figure 3A. Conversely, patients with functional CMD showed no differences in Qmax or Rμ,hyper compared with patients without functional CMD (0.248 vs 0.202 L/min; p=0.12; and 481.2 vs 536.5 WU; p=0.34, respectively), as illustrated in Figure 3B.
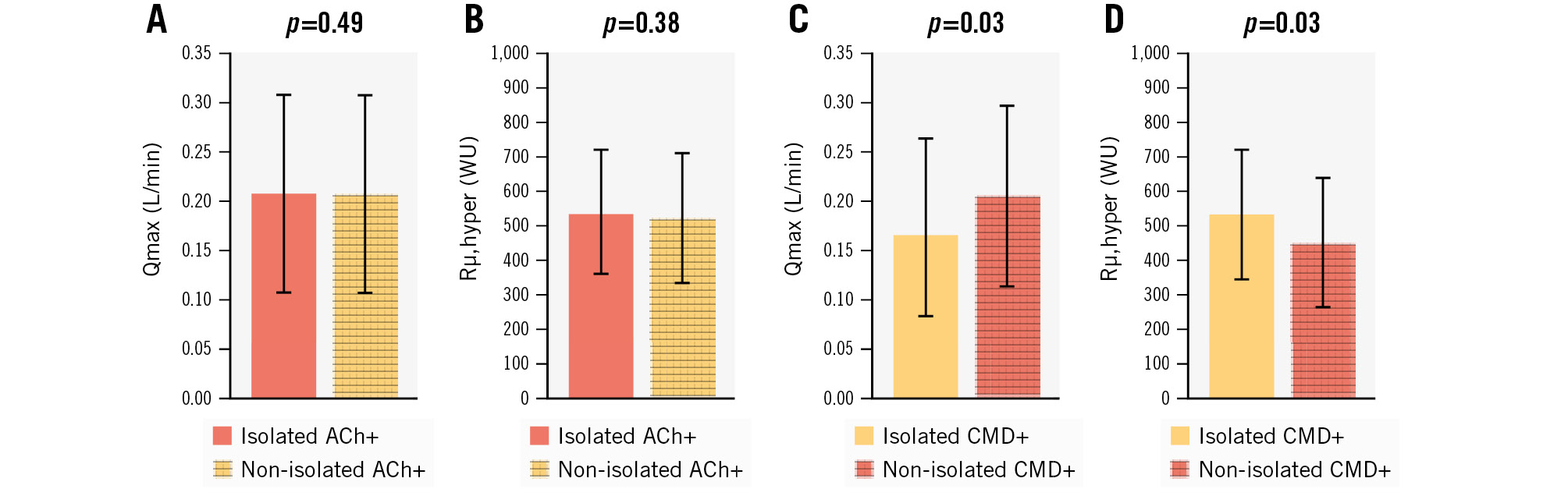
Figure 2. Qmax and Rμ,hyper according to the prevalence of isolated ACh+ and isolated CMD+. A,B) Qmax and Rµ,hyper in patients with isolated/non-isolated acetylcholine testing. C,D) Qmax and Rµ,hyper in patients with isolated/non-isolated CMD. ACh+: patients with coronary spasm; CMD: coronary microvascular dysfunction; Qmax: hyperaemic absolute coronary flow; Rµ,hyper: absolute microvascular resistance; WU: wood unit
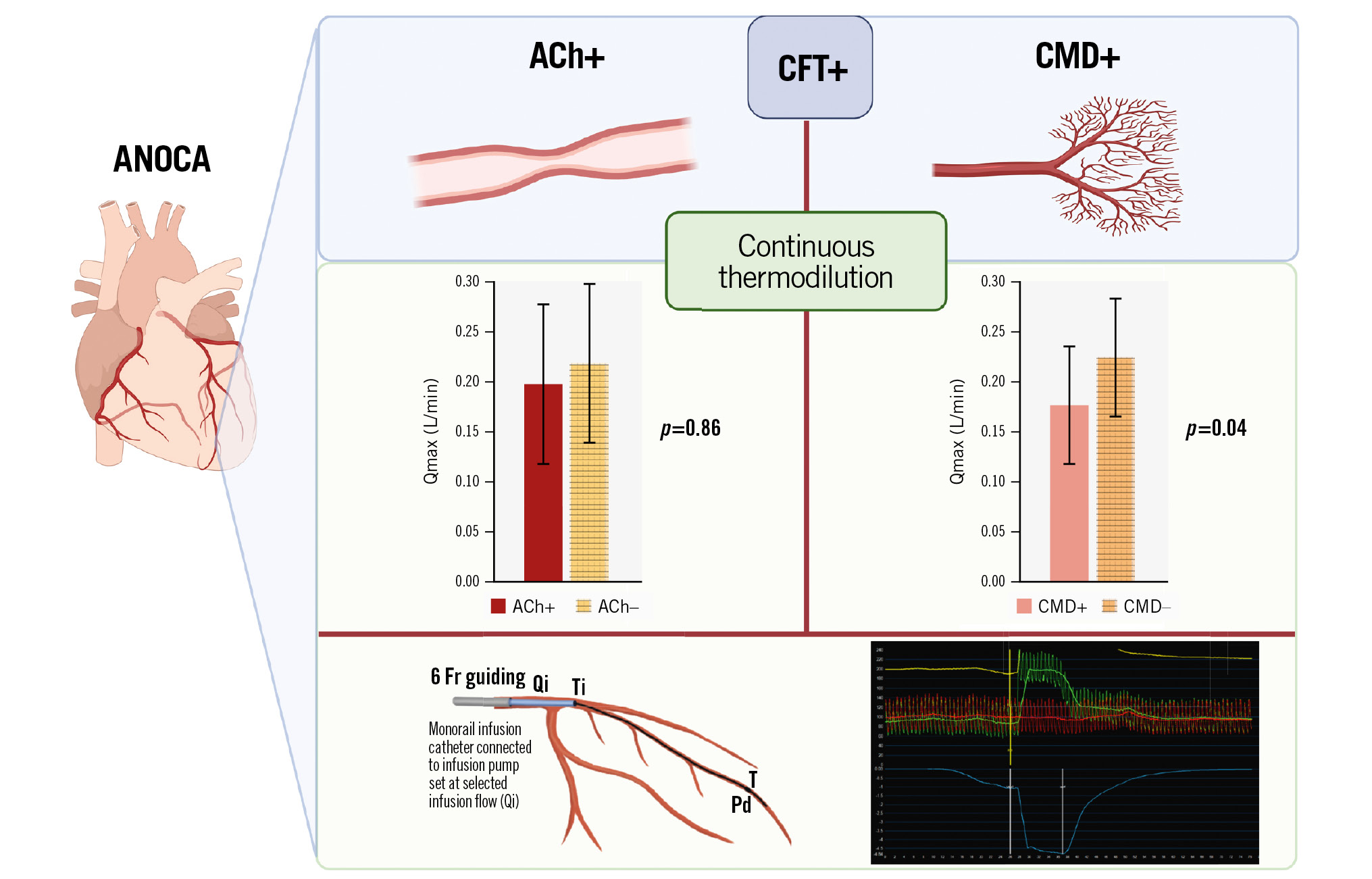
Central illustration. Absolute flow across different ANOCA endotypes. ACh+: patients with coronary spasm; ANOCA: angina with non-obstructive coronary arteries; CFT: coronary function testing; CMD: coronary microvascular dysfunction; Fr: French; Pd: distal coronary pressure; Qi: infusion flow rate; Qmax: hyperaemic absolute coronary flow; T: blood temperature; Ti: temperature of infusion
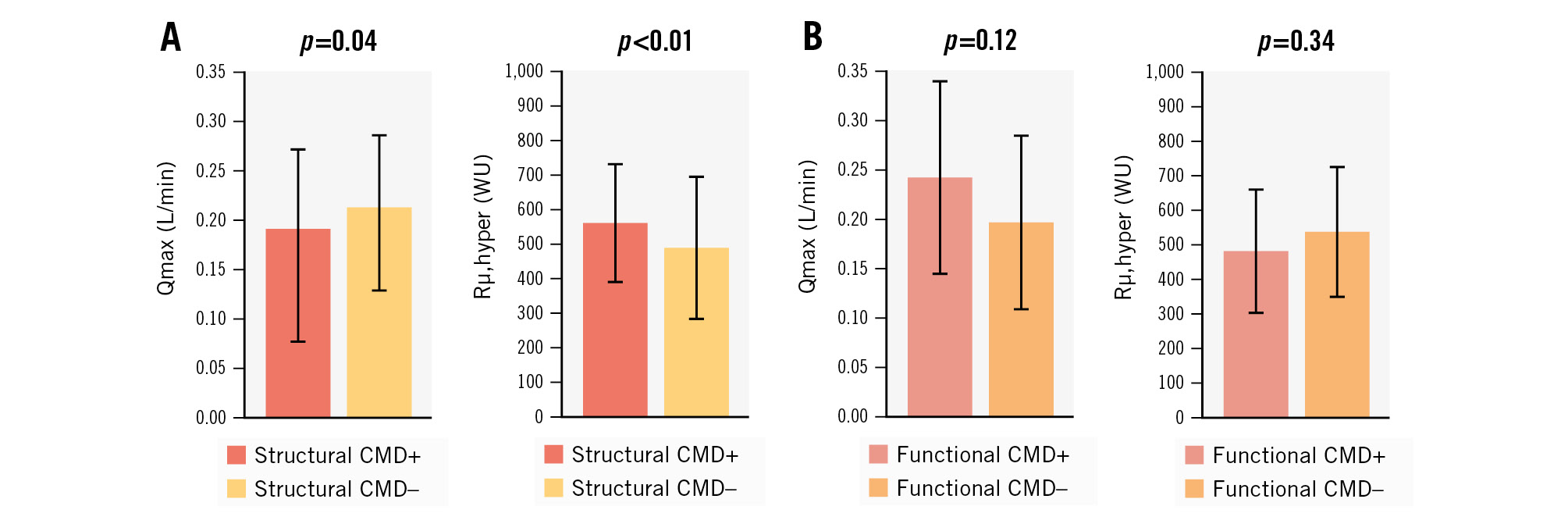
Figure 3. Qmax and Rµ,hyper according to the prevalence of structural or functional CMD. A) Structural CMD+ patients. B) Functional CMD+ patients. CMD: coronary microvascular dysfunction; Qmax: hyperaemic absolute coronary flow; Rµ,hyper: hyperaemic absolute microvascular resistance; WU: wood unit
CORRELATION BETWEEN BOLUS AND CONTINUOUS THERMODILUTION PARAMETERS
Receiver operating characteristic (ROC) analyses revealed that the optimal Rμ,hyper cutoff to predict patients with an IMR ≥25 was identified as 500 WU, with an area under the ROC curve (C-statistic) of 0.66 (95% confidence interval [CI]: 0.56 to 0.76; p=0.003). This 500 WU cutoff accurately classified patients with CMD, achieving a sensitivity of 72% and a specificity of 57%. The optimal range of Rμ,hyper values to predict patients with an IMR ≥25 was found to be between 460 and 540 WU, with a sensitivity ranging from 74% to 72%.
Similarly, ROC analyses identified 0.160 L/min as the optimal Qmax cutoff to predict patients with an IMR ≥25, with an area under the ROC curve (C-statistic) of 0.71 (95% CI: 0.62 to 0.80; p<0.001). This 0.160 L/min cutoff accurately classified patients with CMD, achieving a sensitivity of 65% and a specificity of 58%. The optimal range of Qmax values to predict patients with an IMR ≥25 was found to be between 0.155 and 0.167 L/min, with a sensitivity ranging from 66% to 60% (Figure 4).
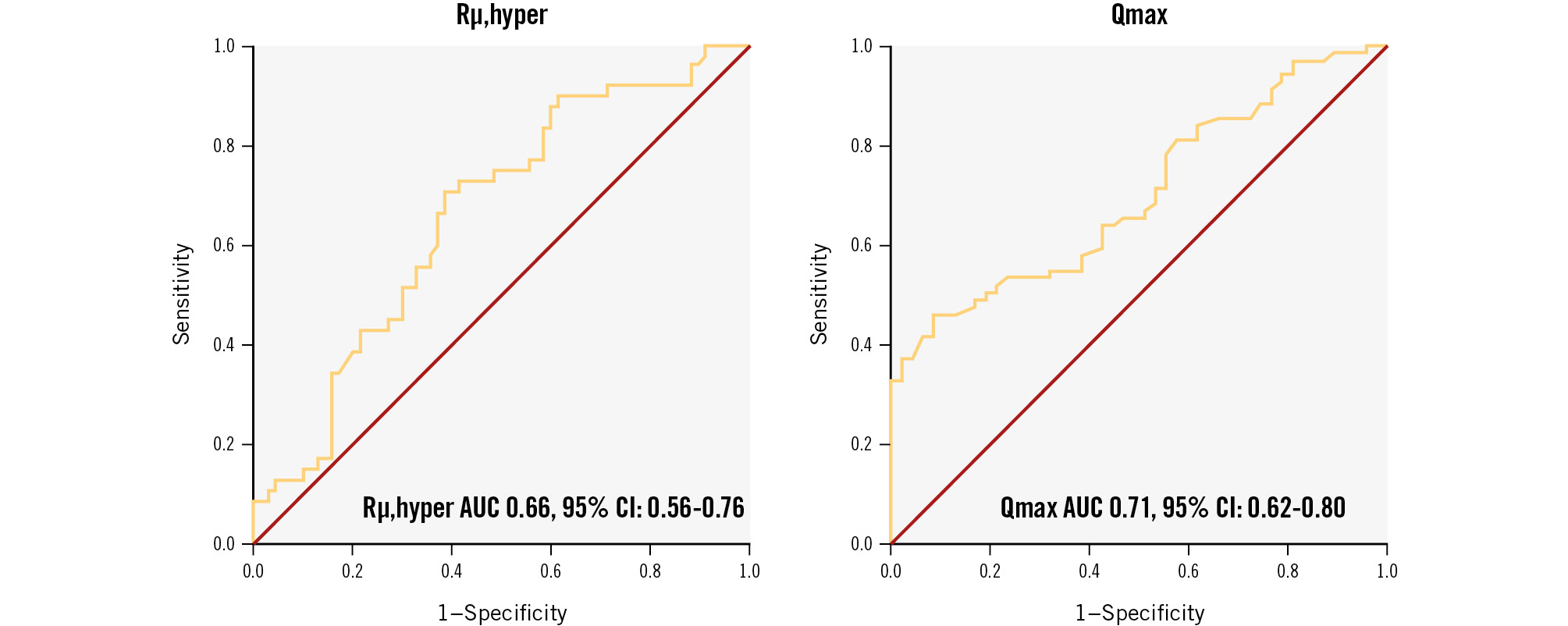
Figure 4. ROC analyses identifying Rµ,hyper and Qmax values for best predicting an IMR ≥25. AUC: area under the curve; CI: confidence interval; IMR: index of microvascular resistance; Qmax: hyperaemic absolute coronary flow; Rµ,hyper: hyperaemic absolute microvascular resistance; ROC: receiver operating characteristic
THERAPEUTIC APPROACHES FOR ANOCA PATIENTS ACROSS VARIOUS ENDOTYPES FOLLOWING CORONARY FUNCTION TESTING
Prior to coronary function testing, 42 (35%) patients were taking beta blockers (BB), 50 (41.7%) were on calcium channel blockers (CCBs), 55 (45.8%) were using angiotensin-converting enzyme (ACE) inhibitors and angiotensin II receptor blockers (ARBs), 68 (56.7%) were prescribed statins, and 35 (29.2%) were using long-acting nitrates.
Following coronary function testing, the percentage of patients taking CCBs and long-acting nitrates increased from 41.7% to 86.7% and from 29.2% to 35.0%, respectively. After CFT, a significantly higher percentage of patients taking CCBs was found in the CFT+ group as compared to the CFT− group (90.9% vs 75.0%; p=0.02). These results were consistent across different ANOCA endotypes (Table 4). Regarding long-acting nitrates, a higher percentage of nitrates was prescribed in CFT+ as compared to CFT− patients (40.9% vs 18.8%; p=0.02). A trend towards a higher use of nitrates was found in the ACh+ group versus the ACh− group (42.8% vs 26.3%; p=0.06). Conversely, the use of nitrates after CFT did not differ between CMD+ and CMD− groups (38.7% vs 31.0%; p=0.38).
Discussion
In this study, we assessed the continuous thermodilution-derived parameters in ANOCA patients undergoing coronary function testing. The goal of the study was to provide a better understanding of the different ANOCA endotypes using Qmax and Rμ,hyper. Moreover, we aimed to assess the correlation between bolus and continuous thermodilution parameters across different ANOCA endotypes.
Up to now, few studies have investigated this novel technique in ANOCA patients, and for the first time, Qmax and Rμ,hyper have been evaluated across all ANOCA endotypes.
The main findings of our study are the following:
- The prevalence of a CFT+ is high in a selected ANOCA population.
- Coronary function testing significantly impacts on the use of antianginal medications across all ANOCA endotypes.
- The novel continuous thermodilution method is safe in patients with ANOCA and can provide further insights into ANOCA endotypes.
- The novel Qmax and Rμ,hyper are associated with a positive CFT.
- Qmax is associated with microvascular dysfunction (CMD+) but not associated with a positive acetylcholine test (ACh+).
- The optimal ranges of Qmax and Rμ,hyper to predict an IMR ≥25 were found to be between 0.155 and 0.167 L/min and 460 and 540 WU, respectively.
Current evidence indicates that ANOCA is not a benign condition, and these patients are at higher risk for major adverse cardiovascular events including death, non-fatal myocardial infarction, heart failure, rehospitalisation and repeated coronary angiography for recurrent angina versus reference subjects8921. The social and economic burden of ANOCA is worsened by the poor awareness of this condition among treating physicians and by the lack of evidence-based recommendations, resulting in inadequate treatment in these patients21.
The CORonary MICrovascular Angina (CorMicA) trial provided evidence that stratified therapy based on invasive diagnostic testing and addressing the underlying mechanisms of ischaemia reduces angina burden and improves quality of life in ANOCA patients1.
A comprehensive assessment of the microcirculatory domain includes detection of both structural microcirculatory remodelling and/or functional arteriolar dysregulation1011. Haemodynamic findings associated with an impaired structural microvasculature in response to a non-endothelium-dependent vasodilator, such as adenosine, are reduced CFR and increase in minimal hyperaemic microcirculatory resistance measured by either bolus thermodilution or the Doppler technique. However, reliable Doppler measurements may be difficult to obtain in “real-world” practice due to a suboptimal Doppler signal in up to 31% of cases14. Bolus thermodilution measurement, based on a manual injection of saline bolus, may be hampered by intraobserver variability and by the cost and side effects of adenosine use22.
A newly developed invasive technique − the continuous thermodilution method − has been shown to be safe, reproducible and operator independent, with no need for additional hyperaemic stimuli14. Continuous thermodilution was found to be associated with significantly less variability in repeated measurements than bolus thermodilution in the assessment of CMD23. Microvascular resistance reserve (MRR), defined as the ratio of true resting microvascular resistance and hyperaemic microvascular resistance measured by continuous thermodilution, has been found to be a suitable index to distinguish the presence or absence of CMD in patients with angina and no obstructive coronary artery disease2425.
Functional arterial dysregulation is related to endothelial dysfunction, determining impaired vasorelaxation or paradoxical vasospasm in response to endothelium-dependent vasoconstricting agents. A positive ACh test indicates the presence of either epicardial or microvascular vasoconstriction.
In our study, coronary function testing was deemed safe and had a significant impact on the utilisation of antianginal medications. Subsequent to CFT, there was a marked increase in the number of patients using CCBs across all ANOCA endotypes. A positive CFT result was associated with a higher prevalence of patients using long-acting nitrates; this was particularly evident in the ACh+ subgroup. However, no significant differences were observed in patients with or without CMD. These findings may be attributed to the vasodilatory effects of long-acting nitrates on both microvascular and epicardial vasomotor disorders, while their efficacy in microvascular structural remodelling remains limited, often accompanied by side effects that restrict their benefits26.
Konst et al showed that Rμ,hyper was higher in patients with the endotype of microvascular dysfunction (defined as high IMR and/or low CFR) and that both Qmax and Rμ,hyper were not associated with the endotype of epicardial or microvascular spasm27. However, no information was provided for either of the subgroups of isolated CMD or isolated positive ACh test, nor for structural or functional CMD. In our study, we found significantly lower Qmax values in patients with CMD (CMD+), regardless of the presence of a vasomotor dysregulation. Interestingly, Qmax values were confirmed to be significantly lower in the subgroup of isolated CMD+, which validates the accuracy of this novel technology to detect the presence of microvascular (dys)function. In our study, Qmax was also not associated with a positive response to acetylcholine (ACh+), and we confirmed this finding to be valid in the subgroup of patients with isolated vasospastic disorder (isolated ACh+).
In line with the results from Konst et al, when we looked at microvascular resistance as assessed by continuous thermodilution, we found that the presence of microvascular dysfunction (CMD+) was associated with significantly higher Rμ,hyper values. These values were consistently higher in isolated CMD+ patients and were within the range of the values previously described as “abnormal”2728. Patients with structural CMD showed a significantly decreased Qmax and a significantly increased Rμ,hyper, whereas the functional CMD subgroup (CFR <2.5 with normal IMR values) did not show any differences in terms of Qmax or Rμ,hyper as compared to the rest of the study population. Structural CMD identifies patients with architectural changes in their coronary circulation, such as arteriolar obliteration, microvascular obstruction and/or capillary rarefaction. These patients can be identified by a decreased Qmax and an increased Rμ,hyper during continuous thermodilution. In contrast, functional CMD patients with diminished CFR and preserved IMR, are characterised by a preserved maximum coronary blood flow and an increased resting coronary blood flow29. These patients can be identified by an increased resting Q (Qrest) and a decreased resting R (Rμ,rest) during continuous thermodilution (i.e., during infusion of saline at 10 mL/min), which was unfortunately not measured at the time of these analyses. The differentiation of these two CMD subgroups not only reflects different underlying pathophysiological mechanisms but also leads to different optimal treatments19.
Both Qmax and Rμ,hyper were significantly abnormal in the whole cohort of patients with positive reaction testing (CFT+). We cannot rule out that the prevalence of 51.7% of patients with CMD (either isolated or combined) may have driven these results, leading to abnormal Qmax and Rμ,hyper values in patients with CFT+ versus CFT−.
In addition, more than one-third of the patients showed both a positive ACh test and microvascular dysfunction. Structural remodelling can also lead to an increased passive stiffness of the vessels and functional dysregulation, enhancing arteriolar sensitivity to vasoconstricting stimuli; therefore, we cannot exclude crosstalk between the two endotypes28.
We further defined the continuous thermodilution range of values able to predict CMD, as diagnosed by bolus thermodilution. ROC analyses identified 500 WU as the optimal Rμ,hyper cutoff to predict patients with an IMR ≥25; these results are in line with those of Rivero et al28.
Despite the easier applicability in clinical practice of a single, sharp cutoff value able to discriminate between “normal” and “diseased” patients with a very high accuracy, a range of abnormal values might better suit the purpose of identifying patients with CMD using continuous thermodilution parameters. The main reason supporting this hypothesis is the considerable variability between individual patients regarding the perfused myocardial mass. Hyperaemic flow and resistance are dependent on the myocardial mass perfused by the supplying artery30. The recently developed MRR index, expressing the ratio of true resting to hyperaemic microvascular resistance, might be the best tool to identify CMD patients. At present, thermodilution methods do not possess the capability to distinguish between ANOCA endotypes, as defined by bolus thermodilution. Nevertheless, the findings of the current analysis hold promise for shedding additional light on the exploration of various endotypes. This study lays the groundwork for future investigations aimed at pinpointing optimal cutoff values capable of distinguishing between different endotypes using a more standardised and reproducible technique.
Limitations
The results of this study should be interpreted in light of some limitations.
This is a single-centre study of a large tertiary referral centre specialising in patients with ANOCA. Patients included in this study are selected and might not represent the whole population of ANOCA patients. However, the aim of this study was to evaluate patients who were symptomatic despite optimal medical therapy.
Despite this limitation, our study represents one of the largest single-centre cohorts published so far. The sample size in each ANOCA subgroup was limited, which hampers the ability to draw strong conclusions and prevented us from further investigating a possible interaction between endotypes. As mentioned above, strict criteria were used to select patients for the final analysis.
Presently, various protocols exist for diagnosing vasospastic angina, each employing different doses of ACh. We opted for a dosage of ACh at 200 μg, acknowledging the potential risk of overdiagnosing the VSA endotype. However, consensus has yet to be reached regarding the threshold of ACh dosage necessary to define VSA.
At the time this manuscript was submitted, no consensus had been reached on reference values for Qmax and Rμ,hyper; the proposed normal values are Qmax >200 mL/min and Rμ,hyper <500 WU16. This limits the interpretation of these results, as the definition of different endotypes was based on the results of bolus thermodilution assessment.
At the time when the majority of patients were enrolled, the MRR index had not been developed, therefore resting Q and Rμ were only measured in a limited subgroup of patients, which did not allow for further analysis.
Conclusions
Our results confirm the safety of performing continuous thermodilution measurements in patients with ANOCA.
Qmax is lower in patients with microvascular dysfunction and does not correlate with the presence of vasomotor dysregulation, as detected by acetylcholine testing. The best range of Qmax and Rμ,hyper values to identify IMR ≥25 are 0.155-0.167 L/min and 460-540 WU, respectively.
Future studies with a predefined effect and sample size are needed to determine the diagnostic potential of Qmax and Rμ,hyper across different ANOCA endotypes.
Impact on daily practice
This study demonstrates the safe implementation of continuous thermodilution in patients with angina with non-obstructive coronary arteries, offering new perspectives on endotype differentiation and serving as a complementary tool to traditional thermodilution methods.
Conflict of interest statement
V. Paradies declares a research grant from Abbott via the institution; speaker fees from Abbott and Boston Scientific; and an educational grant from Terumo via the institution. P.C. Smits has received consultancy fees and institutional research grants from Abbott. P. Damman has received consultancy fees from Philips and Abbott; institutional research grants from Philips and Abbott; and speaker fees from Philips and Abbott. The other authors have no conflicts of interest relevant to the contents of this paper to declare.
Supplementary data
To read the full content of this article, please download the PDF.