Cory:
Unlock Your AI Assistant Now!
Abstract
Background: The diagnostic yield of invasive coronary angiography (ICA) in patients with chronic coronary syndromes (CCS) in contemporary practice is uncertain.
Aims: We investigated the value of an advanced invasive diagnosis (AID) strategy combining angiography and intracoronary testing.
Methods: AID-ANGIO is an all-comers, prospective, multicentre study enrolling CCS patients referred for ICA. Obstructive coronary artery disease (CAD) was investigated with angiography and pressure guidewires. In the absence of obstructive CAD, intracoronary testing for ischaemia with non-obstructive coronary arteries (INOCA) was performed. The primary endpoint was the proportion of patients with a cause of ischaemia identified by the AID strategy. To assess the effect of AID on decision-making, an initial therapeutic plan was first prepared by clinical cardiologists based on ICA and medical information. Subsequently, based on AID data, a final therapeutic plan was drafted by clinical and interventional cardiologists (Ischaemia Team).
Results: We enrolled 317 patients (44.2% female). Based on ICA, obstructive CAD was diagnosed in 32.2% of patients. With the AID strategy, a cause of myocardial ischaemia was identified in 84.2% (p<0.001): obstructive CAD in 39.1% and INOCA in 45.1%. Only 15.8% of patients did not show any abnormalities. Modification of the original treatment plan with the AID strategy occurred in 59.9% of cases.
Conclusions: In assessing ischaemia-generating coronary abnormalities, prespecified use of the AID strategy was associated with a 2.6-fold increase in diagnostic yield compared with ICA (84.2% vs 32.2%, respectively), largely due to the identification of INOCA. Modification of the therapeutic plan with the AID strategy occurred in 59.9% of cases. (ClinicalTrials.gov: NCT05635994)
Invasive coronary angiography (ICA) is a standardised method to identify coronary artery disease (CAD). However, its diagnostic yield is very low, with a reported prevalence of obstructive CAD of <38% in a nationwide series of 400,000 patients with chronic coronary syndrome (CCS)1. Such limited performance may be explained by the fact that ICA alone is a suboptimal tool for assessing the functional relevance of intermediate-grade stenosis2345 and in its inability to identify non-obstructive causes of myocardial ischaemia6.
Contemporary American and European clinical practice guidelines recommend the evaluation of intermediate-grade stenosis with pressure guidewires, using fractional flow reserve (FFR) or non-hyperaemic pressure ratios789. Likewise, they recommend considering an invasive assessment of microvascular function and vasomotor responses in patients with persistent anginal symptoms and coronary arteries that are either angiographically normal or have functionally non-significant stenoses789. Despite the widespread availability of the technologies, functional assessment of obstructive and non-obstructive causes of myocardial ischaemia in the catheterisation laboratory is heterogeneous and far from optimal, precluding adequate cause-based, stratified treatment1011.
The objective of our study was to investigate the diagnostic yield of an invasive strategy for a hierarchical identification of obstructive and non-obstructive mechanisms of ischaemia in patients with CCS, performed at the time of ICA. We also aimed to assess how the obtained information modified a therapeutic plan based only on ICA and the available clinical information.
Methods
Study overview
Advanced Invasive Diagnosis for Patients with Chronic Coronary Syndromes Undergoing Coronary ANGIOgraphy (AID-ANGIO) is an all-comers, observational, prospective, multicentre study (ClinicalTrials.gov: NCT05635994) carried out at four hospitals in the Madrid region (Spain). The study activities were approved by the local ethics committee at each of the enrolling centres, and written informed consent was obtained from all participants.
Study population
The study enrolled all consecutive patients with CCS referred for ICA by their responsible clinical cardiologist due to angina and/or evidence of ischaemia in non-invasive tests and/or the presence of CAD in coronary computed tomography angiography (CCTA).
Clinical scenarios for CCS identified by European Society of Cardiology (ESC) guidelines were considered7. Only patients with congestive heart failure or severe left ventricular dysfunction were excluded, since invasive functional coronary assessment in these scenarios remains uncertain12. Patients with previous coronary artery bypass graft (CABG) or who had undergone percutaneous coronary intervention (PCI) within the past 3 months were not included. A full list of exclusion criteria is provided in Supplementary Table 1.
The AID strategy
The advanced invasive diagnosis (AID) strategy is a hierarchical algorithm designed to streamline the assessment of both obstructive and non-obstructive causes of myocardial ischaemia at the time of ICA. The protocol was started by performing ICA in a standard fashion. Patients were instructed not to take either caffeine or antianginal medications within the 12 hours before the procedure. The radial artery approach was the preferred arterial access. Orthogonal angiographic projections were obtained to ensure optimal outlining of epicardial vessels. Severe-grade stenoses (≥90% diameter stenosis [DS] by visual assessment) were considered flow limiting and responsible for the patients’ symptoms, without further physiological assessment. Intermediate-grade stenoses (<90% DS by visual assessment) were evaluated with FFR and/or resting full-cycle ratio (RFR) to determine their physiological significance (Figure 1). General recommendations for adequate pressure guidewire measurements were followed1314. Under full heparinisation (50-70 U/kg with an activated clotting time over 250 s), a dedicated 0.014 inch guidewire was advanced into the target vessel via a 6 Fr guiding catheter. Pressure equalisation was performed at the tip of the catheter, and then the wire was positioned distal to the stenosis. Flushing of contrast media with saline was ensured before measuring the RFR and/or FFR.
Patients with either angiographically normal epicardial vessels or only intermediate stenoses with non-ischaemic FFR/RFR values (FFR>0.80 and/or RFR>0.89) underwent functional coronary testing to rule out microcirculatory and/or vasomotor coronary disorders causing ischaemia with non-obstructive coronary arteries (INOCA). A physiological evaluation of the epicardial and microvascular domains was performed using the PressureWire X Guidewire (Abbott) with the CoroFlow Cardiovascular System (Coroventis), which is equipped with both a pressure sensor, to evaluate FFR and RFR, and a thermistor, to perform thermodilution-based flow measurements.
The interpretation of intracoronary testing was based on available ESC guidelines on CCS7 and the European Association of Percutaneous Cardiovascular Interventions (EAPCI) consensus document on INOCA15. A diagnosis of endothelium-independent coronary microvascular dysfunction (CMD) was established in the presence of a reduced coronary flow reserve (CFR) and/or an increased index of microcirculatory resistance (IMR), measured by bolus thermodilution. The abnormality cutoff value for CFR was <2.0 and for IMR was ≥25. The calculation of IMR was corrected by Yong’s formula to estimate the influence of epicardial disease. Measurements were performed in the left anterior descending artery by default, since it supplies a larger myocardial mass. However, other coronary arteries could be studied at the operator’s discretion if the initial tests were negative and clinical suspicion was high. Steady-state hyperaemia was induced by intravenous infusion of adenosine at 140 μg/kg/min16. To assess endothelium-dependent coronary function, sequential intracoronary boli of acetylcholine at concentrations of 2 μg, 20 μg, 100 μg, and 200 μg in the left main or 2 μg, 20 μg, and 80 μg in the right coronary artery were manually performed. The time administration of each dose lasted from 50-60 s, followed by flushing of the guiding catheter with saline to ensure that the whole dose reached the coronary arteries1517. Epicardial coronary spasm was diagnosed if a ≥90% reduction of angiographic vessel diameter was present, with reproduction of the patient’s anginal symptoms and transient ischaemic electrocardiogram (ECG) changes at the time of acetylcholine administration. Conversely, microvascular spasm was diagnosed when both anginal symptoms and ischaemic ECG changes occurred, in the absence of epicardial spasm15. Further details regarding the functional coronary assessment protocol are provided elsewhere14.
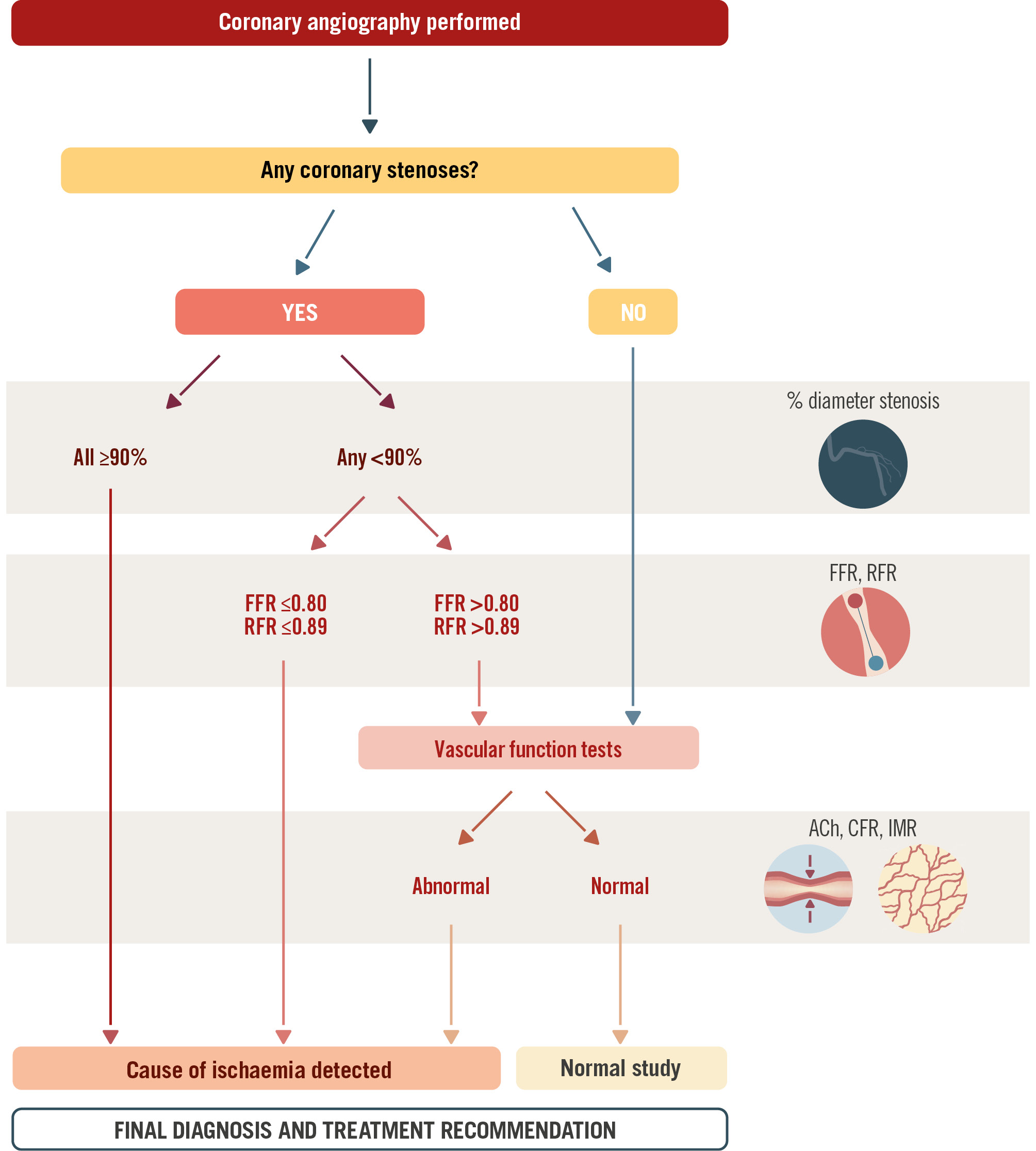
Figure 1. Schematic representation of the advanced invasive diagnosis (AID) algorithm. The AID strategy combines invasive angiography with intracoronary testing to outline obstructive and non-obstructive causes of myocardial ischaemia. ACh: acetylcholine; CFR: coronary flow reserve; FFR: fractional flow reserve; ICA: invasive coronary angiography; IMR: index of microcirculatory resistance; RFR: resting full-cycle ratio
Impact of the AID strategy on clinical decision-making
In order to assess how the complementary information obtained with the AID strategy might modify the therapeutic plan based on ICA and available clinical information, the study was conducted in two steps. First, once ICA was performed, the angiographic images were shown to the patient’s referring clinical cardiologist. They were asked to identify epicardial stenoses affecting vessels amenable to revascularisation, specifying if they were angiographically severe or not. In the case of intermediate-grade stenoses, they were asked to judge whether they were ischaemia-generating or not. In scenarios of angiographically normal vessels, whenever non-obstructive ischaemia was suspected as the underlying cause for the patient’s symptoms, the referring clinical cardiologist was also requested to specify the suspected INOCA endotype (vasomotor, CMD, or mixed). The clinical cardiologist was then asked to suggest a tentative therapeutic plan, advocating for revascularisation (PCI or CABG) or medical treatment (including the selection of specific drugs). All of this information was collected in a written document to which the interventional cardiologists were blinded. As a second step, the AID strategy was then applied, and the results of intermediate-grade stenosis assessment and/or functional coronary testing were collected in a separate form. The final step consisted of a meeting between the clinical and interventional cardiologists (Ischaemia Team) to review the case and decide on a definite diagnosis and therapeutic plan. Modification from the initial to the final therapeutic plan was recorded. Treatment recommendations for patients with INOCA were followed1115 and are summarised in Supplementary Table 2. The additional time required to apply the full AID-ANGIO strategy was calculated as the difference in procedural time between patients in whom a diagnosis was made on ICA alone and those in whom thermodilution and acetylcholine testing were performed.
Study endpoints
The primary endpoint of the study was the proportion of patients in whom a cause of myocardial ischaemia was identified with ICA alone, as well as with the support of the AID strategy. Secondary endpoints included the proportion of patients in whom non-obstructive causes of myocardial ischaemia were identified, as well as the proportion of cases in which the AID strategy led to a change from the initial therapeutic plan, which was based on clinical information and ICA alone. The study did not aim to assess clinical outcomes associated with assigned therapeutic strategies.
Statistics
Quantitative variables are expressed as median and interquartile range (IQR) or mean and standard deviation. Categorical variables are expressed as frequencies and percentages and were compared with the chi-square test. All tests were 2-sided, and differences were considered statistically significant with p-values<0.05. Statistical analyses were performed using the Stata IC12.1 statistical software package (StataCorp).
Results
Study population
The study was conducted between June 2022 and December 2023. Supplementary Table 3 shows the dates each hospital participated in the study. Out of 365 consecutive patients with CCS referred for ICA, 317 patients who fulfilled the inclusion criteria were prospectively enrolled, comprising the study population. The causes for the exclusion of the 48 remaining patients (13.2%) are summarised in Supplementary Table 4.
Baseline characteristics
The patient population included a relevant number of female patients (44.2%). The mean age was 66 (IQR 58-73) years, and 61.2% had undergone a non-invasive ischaemia test or CCTA. Other baseline characteristics, including angina-related quality of life, assessed with the Seattle Angina Questionnaire (SAQ), and the results from non-invasive ischaemia tests are summarised in Table 1.
Table 1. Baseline characteristics of the study population.
| Characteristics | N=317 |
|---|---|
| Age, years | 66 (58-73) |
| Female sex | 140 (44.2) |
| Hypertension | 197 (62.2) |
| Dyslipidaemia | 208 (65.6) |
| Diabetes | 92 (29.0) |
| Insulin dependent | 15 (16.3) |
| Active smoker | 49 (15.5) |
| Former smoker | 103 (32.5) |
| Body mass index, kg/m² | 27.67 (25.0-30.2) |
| Family history of CAD | 23 (7.3) |
| Peripheral vascular disease | 15 (4.7) |
| Chronic kidney disease | 18 (5.6) |
| eGFR, mL/min/1.73 m² | 84.2 (69.6-94.2) |
| Previous MI | 50 (15.8) |
| Previous PCI | 57 (18.0) |
| Previous ICA | 112 (35.3) |
| Symptoms | |
| Exertional angina CCS | 185 (58.4) |
| I | 17 (8.3) |
| II | 142 (76.8) |
| III | 26 (13.8) |
| Episodes of angina at rest | 47 (14.8) |
| Atypical chest pain | 62 (19.6) |
| Dyspnoea | 57 (18.0) |
| Symptom assessment | 265 (83.6) |
| SAQ - Physical limitation | 75.0 (60.0-88.9) |
| SAQ - Angina stability | 50.0 (33.3-66.7) |
| SAQ - Angina frequency | 75.0 (66.7-83.3) |
| SAQ - Treatment satisfaction | 81.0 (66.7-90.5) |
| SAQ - Quality of life | 53.3 (40.0-66.7) |
| SAQ - Overall score | 71.7 (61.6-78.8) |
| Complementary tests | |
| LVEF on TTE, % | 60 (55-65) |
| Exercise ECG test | 131 (41.3) |
| Positive result | 91 (69.4) |
| Stress echocardiography | 55 (17.4) |
| Positive result | 36 (65.5) |
| SPECT | 34 (10.7) |
| Positive result | 25 (73.5) |
| Stress MRI | 1 (0.3) |
| Positive result | 1 (100) |
| CCTA | 47 (14.8) |
| Data are presented as median (IQR) or n (%). CAD: coronary artery disease; CCS: Canadian Cardiovascular Society; CCTA: coronary computed tomography angiography; ECG: electrocardiography; eGFR: estimated glomerular filtration rate; ICA: invasive coronary angiography; IQR: interquartile range; LVEF: left ventricular ejection fraction; MI: myocardial infarction; MRI: magnetic resonance imaging; PCI: percutaneous coronary intervention; SAQ: Seattle Angina Questionnaire; SPECT: single-photon emission computed tomography; TTE: transthoracic echocardiography | |
Angiography-based diagnosis
Based on angiography alone, clinical cardiologists identified obstructive CAD with angiographically severe stenoses in 102 (32.2%) patients, of whom 22 (21.6%) concomitantly presented intermediate-grade stenoses. Likewise, 74 patients (23.3%) had intermediate-grade or ambiguous stenoses, and 141 (44.5%) presented no angiographic stenoses, precluding a definite diagnosis. However, taking into account the clinical history and the results of non-invasive tests, suspected diagnoses of obstructive CAD, INOCA, and chest pain of non-ischaemic origin were reached in 126 (39.7%), 165 (52.1%) and 26 (8.2%) patients, respectively. Further information regarding tentative diagnosis and therapeutic plan by the clinical cardiologists is summarised in Supplementary Table 5-Supplementary Table 6-Supplementary Table 7-Supplementary Table 8.
Primary and secondary study endpoints
With the support of the AID strategy, a cause of myocardial ischaemia was identified in 267 (84.2%) of the patients, which represents an additional 47.9% of patients with an identified cause of myocardial ischaemia, compared to ICA alone (p<0.001). Overall, the implementation of the AID strategy resulted in a 2.6-fold increase in the diagnostic yield of ICA (84.2% vs 32.2%) (Central illustration).
Obstructive CAD was diagnosed in 124 (39.1%) patients, of whom 35 (28.2%) presented with intermediate-grade stenoses with significant RFR and/or FFR values. The distribution of obstructive lesions is summarised in Supplementary Table 9. INOCA was diagnosed in 143 (45.1%) patients of the study population, including microvascular dysfunction in 32 cases (22.4%), vasomotor disorders in 78 (54.5%), and a mixed endotype in 33 patients (23.1%). Among those patients diagnosed with vasomotor disorders, 55.9% presented with epicardial spasm, whereas the rest (44.1%) presented with microvascular spasm. Only 50 patients (15.8%) presented no evident cause of myocardial ischaemia (Figure 2). Information regarding the invasive functional test is summarised in Supplementary Table 10.
Application of the AID strategy, in addition to the clinical information and ICA, resulted in a change in the initial therapeutic plan in 190/317 cases (59.9%), including the avoidance of unnecessary PCI in 19 (20.4%) of patients (Figure 3). Moreover, out of the 165 cases in whom the clinical cardiologist proposed INOCA during the tentative diagnosis, an incorrect diagnosis was made in 78.2% of cases, either because INOCA was not confirmed by the AID strategy (35.7%) or because the wrong endotype was identified in the initial plan (64.3%) (Figure 4). Further details regarding these changes are summarised in Supplementary Table 11-Supplementary Table 12-Supplementary Table 13 and Supplementary Figure 1. Overall, the application of the full AID strategy, including CFR and IMR measurements and acetylcholine testing, resulted in a median additional time of 15 minutes, compared to ICA alone (Supplementary Table 14).
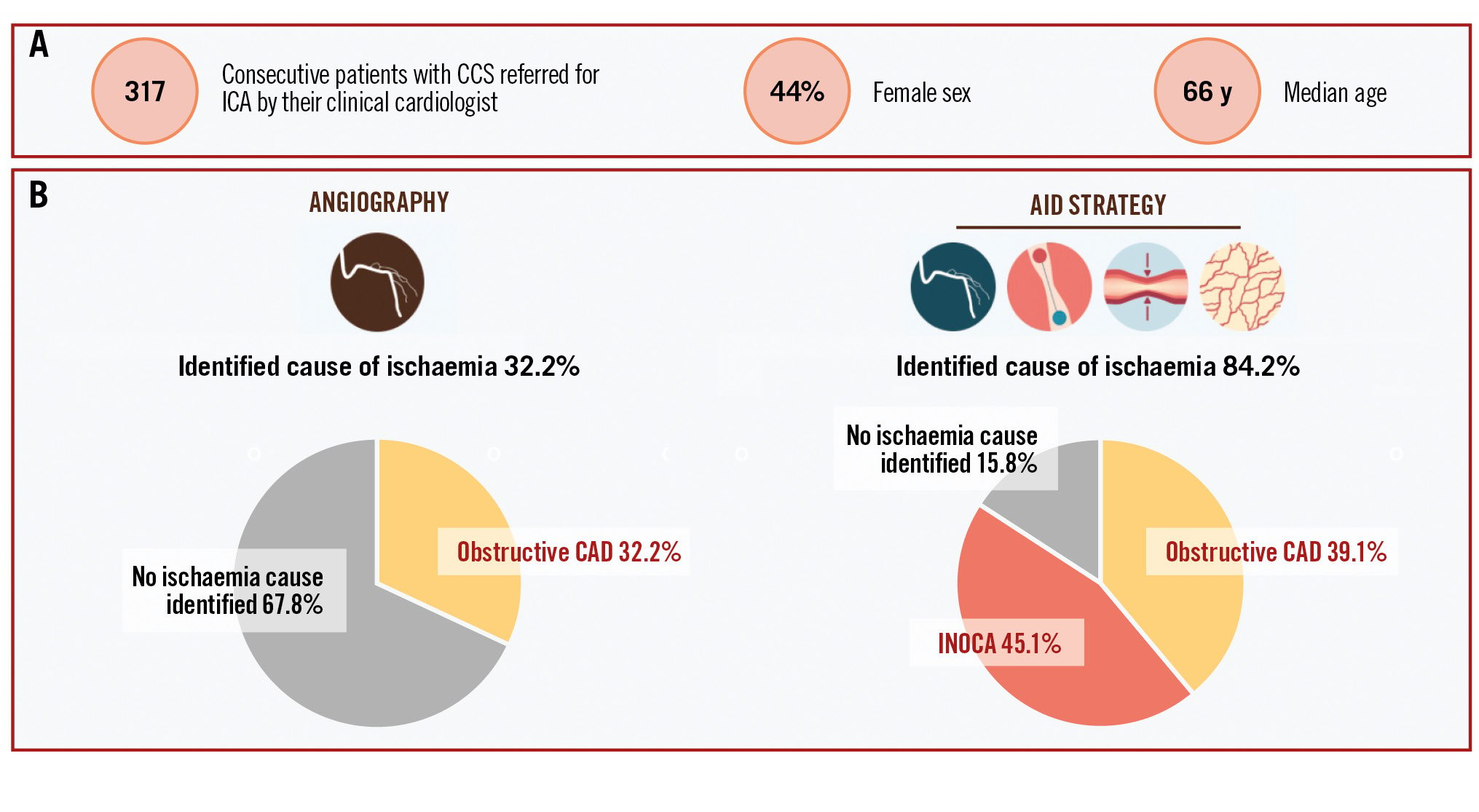
Central illustration. The AID-ANGIO study: characteristics and main results. A) Baseline patient characteristics. B) ICA alone identified a cause of myocardial ischaemia in 32.2% of the patients. The AID strategy identified a cause of myocardial ischaemia in 84.2% of the patients, which represents a 2.6-fold increase in the diagnostic yield. INOCA was the most prevalent cause of myocardial ischaemia (45.1%). AID: advanced invasive diagnosis; CAD: coronary artery disease; CCS: chronic coronary syndrome; ICA: invasive coronary angiography; INOCA: ischaemia with non-obstructive coronary arteries
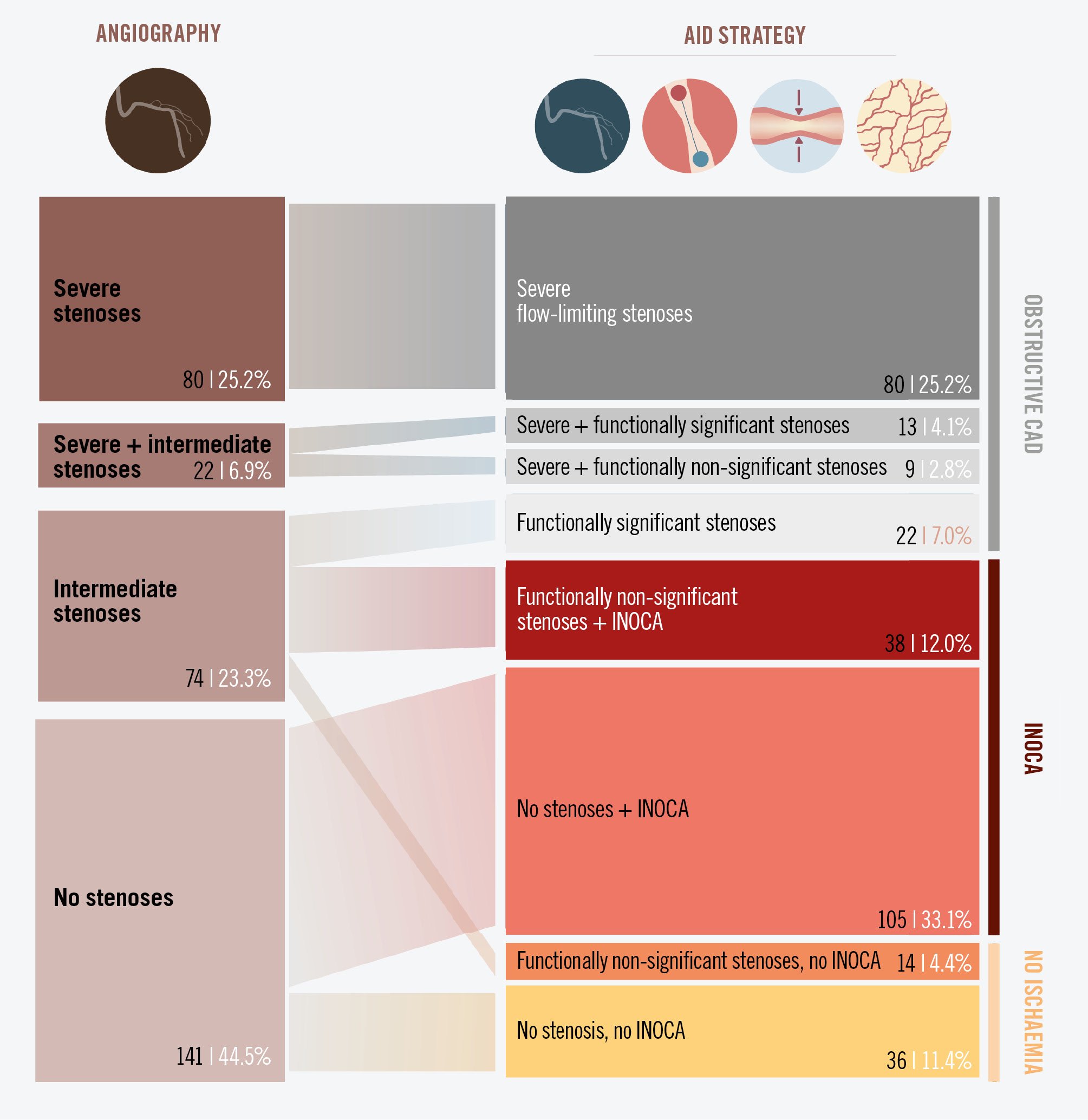
Figure 2. Diagnostic yield of ICA and the AID strategy. The left column shows the number of patients with severe- and intermediate-grade stenoses and those with angiographically normal coronary arteries. The right column shows the final diagnosis, based on the AID strategy. AID: advanced invasive diagnosis; CAD: coronary artery disease; ICA: invasive coronary angiography; INOCA: ischaemia with non-obstructive coronary arteries
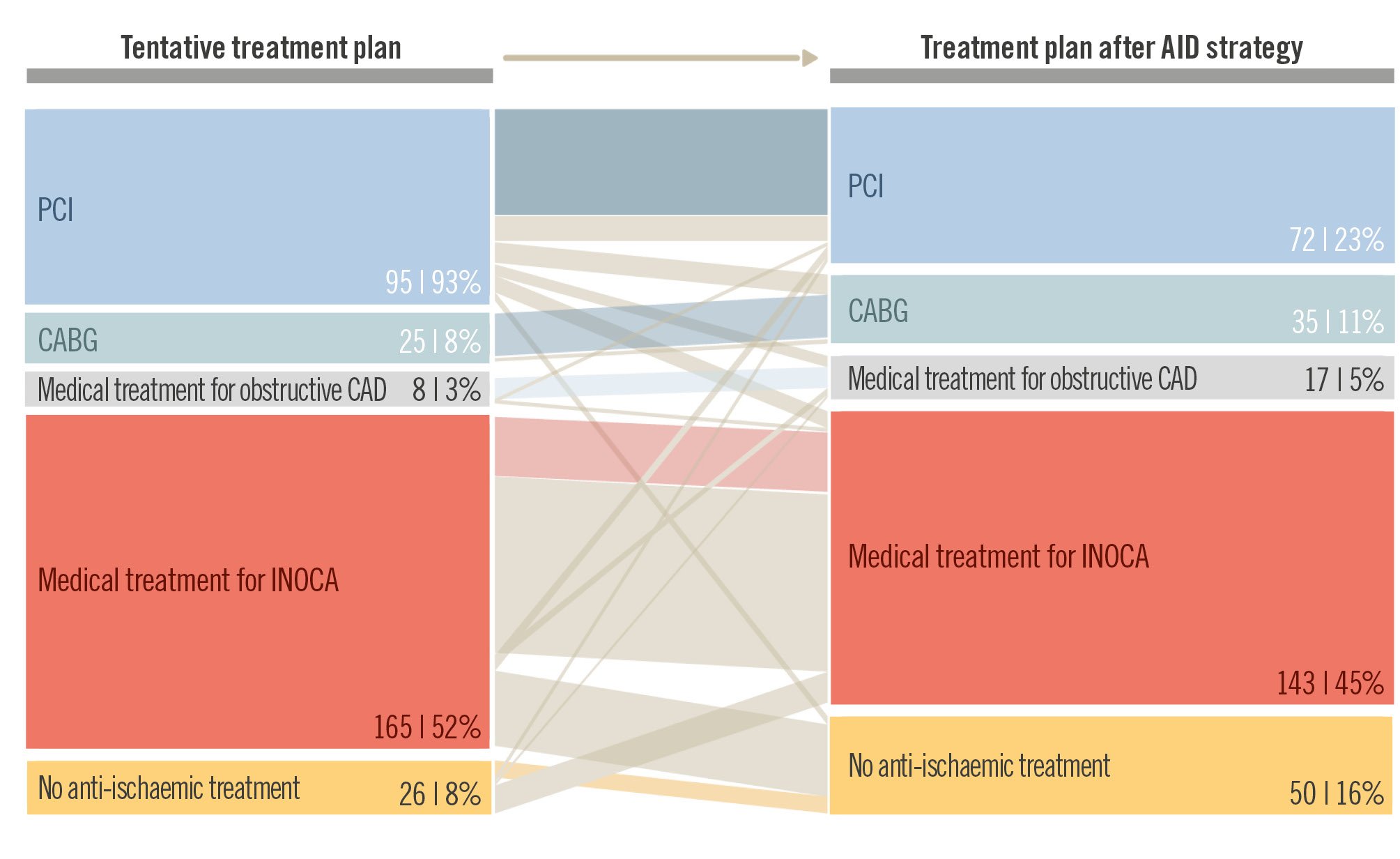
Figure 3. Impact of the AID strategy on clinical decision-making. The tentative therapeutic plan (left column), which had been laid out by clinical cardiologists based on angiography and clinical information alone, changed after the application of the AID strategy (right column). Linking bars with the same colour indicate no change in the treatment plan. Light grey linking bars indicate a modification of treatment, even inside the same treatment category (for example, change in PCI targets or INOCA endotype). AID: advanced invasive diagnosis; CABG: coronary artery bypass graft; CAD: coronary artery disease; INOCA: ischaemia with non-obstructive coronary arteries; PCI: percutaneous coronary intervention
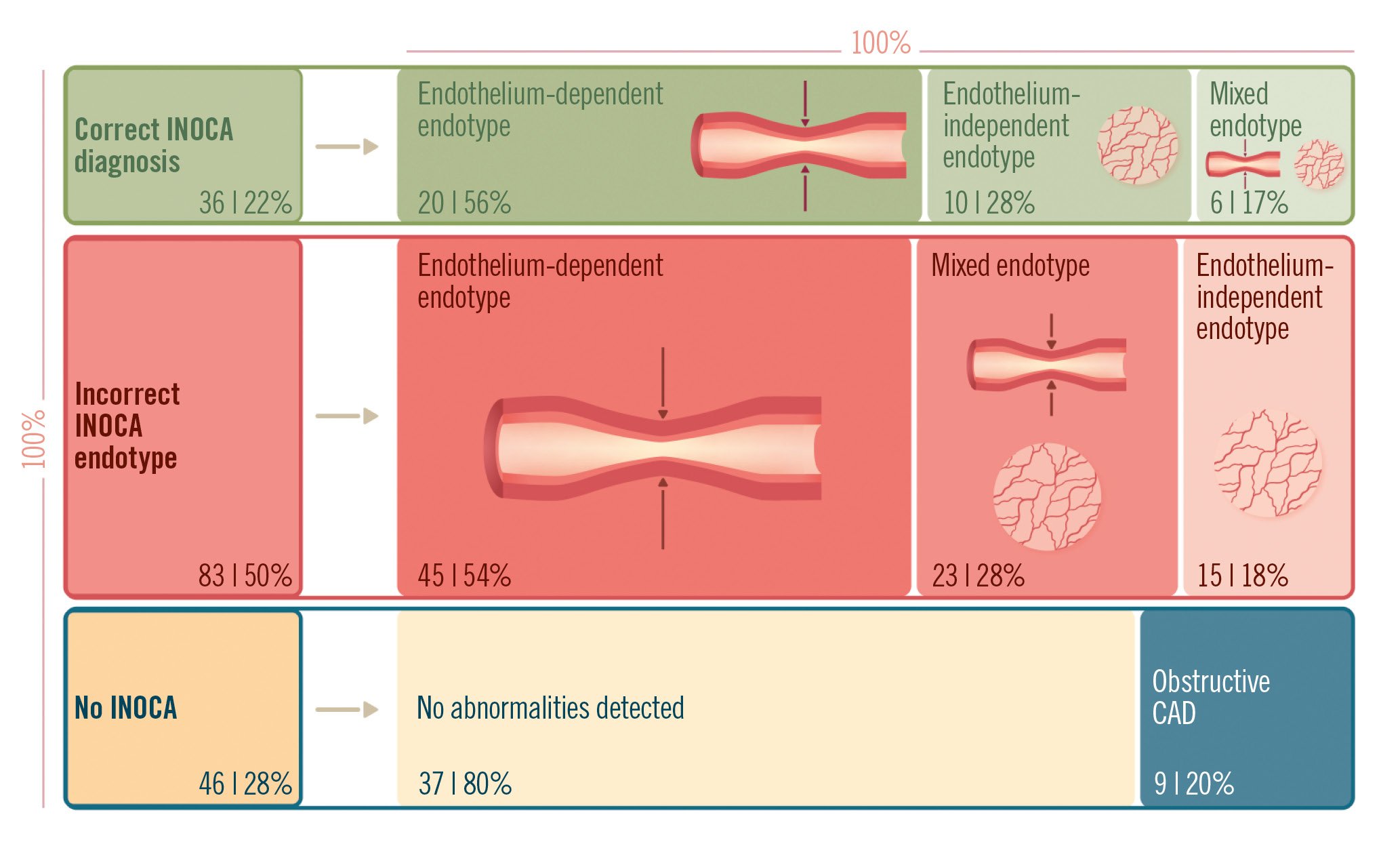
Figure 4. Final diagnosis and therapeutic plan in patients in whom INOCA was initially suspected. Among patients in whom the clinical cardiologist initially suspected INOCA, a correct diagnosis was made in 22% according to the findings in the AID strategy. In the remaining cases, the initial diagnosis was erroneous because of different INOCA endotypes, normal coronary function, or underestimation of obstructive disease. AID: advanced invasive diagnosis; CAD: coronary artery disease; INOCA: ischaemia with non-obstructive coronary arteries
Adverse events and complications
Overall, the systematic application of the AID strategy was safe. Among patients undergoing assessment with a pressure guidewire, 2 cases of iatrogenic coronary artery dissection occurred (0.9%), which was guide catheter related in one case and wire related in the other; both were successfully managed with coronary stenting. Development of transient atrial fibrillation was documented in 8 (4.3%) cases in response to the administration of acetylcholine and in 1 (0.5%) case in response to adenosine. Also, 1 (0.5%) case of ventricular fibrillation occurred in response to acetylcholine in a patient who developed extensive epicardial spasm and ischaemia; this was successfully managed with electrical cardioversion and intracoronary nitrates. There were no deaths. Detailed information on all safety aspects is provided in Supplementary Table 15.
Discussion
Although ICA continues to be the most commonly used technique for the diagnosis of CAD, our findings show a large discrepancy between its invasive nature and the amount of information it delivers. The low diagnostic yield of ICA in our study was mainly due to the frequent existence of non-obstructive causes of myocardial ischaemia but also to the uncertainty surrounding the relevance of intermediate stenoses. Application of a prespecified structured diagnostic approach at the time of ICA led to a significant change in the initial therapeutic plan, which had been laid out by the clinical cardiologist on the grounds of angiography and available clinical information. This approach also led to a significant change in the therapeutic management applied to patients in whom INOCA was initially suspected.
The AID strategy is based on recommendations made by European and American guidelines for the invasive assessment of intermediate stenoses and non-obstructive causes of ischaemia. By enrolling an all-comer population of patients with CCS, the AID-ANGIO study provided valuable insights into the prevalence of obstructive CAD, as well as vasomotor disorders and CMD in real-world patients referred for ICA. The study was performed in a well-balanced population in terms of sex (44.2% female), with exertional angina as the most prevalent symptom, and an SAQ angina frequency score of 75.0 points, denoting more symptomatic patients than in the ISCHEMIA trial (81.4 points)18.
The distribution of coronary abnormalities in our all-comers population is of interest when revisiting the value of other diagnostic tools in patients with CCS. CCTA, an increasingly used diagnostic tool, has the advantages of non-invasiveness and allowing functional stenosis analysis (i.e., FFR derived from CCTA [FFR-CT])19. Yet, CCTA cannot diagnose INOCA2021, which occurred in 45.1% of our patients. Non-invasive ischaemia tests capable of measuring CFR, like positron emission tomography or cardiac magnetic resonance, are valuable in diagnosing CMD. In fact, ischaemic ECG changes and/or anginal symptoms in exercise stress tests have been recently described as having excellent sensitivity and positive predictive values to detect CMD. Yet these tests cannot diagnose vasomotor disorders, which we observed in 35.0% of patients in our study population.
Overall, ICA alone demonstrated obstructive CAD in only 32.2% of patients with at least one severe stenosis, a figure similar to that reported in the reference study by Patel et al1. Of note, the AID strategy also provided additional information in patients who presented with intermediate-grade stenoses (21.6%), leading to several changes in the revascularisation plan, including in 27 patients with multivessel disease; this mirrors the findings from previous studies such as FAME22 and SYNTAX II23. Pressure guidewire interrogation also influenced the decision to perform revascularisation in patients with a single intermediate-severity stenosis, with a further 17.9% allocated to medical treatment after application of the AID strategy.
A key finding of our study is the high prevalence of INOCA in patients with CCS, which occurred in 45.1% of patients. Importantly, INOCA was diagnosed not only in patients with angiographically normal vessels but also in patients with functionally non-significant stenoses, with a similar incidence in both scenarios (74.4% and 73.0%, respectively). We also found that inferring the INOCA endotype from ICA and clinical information was not feasible (Figure 4), a critical aspect in determining effective medical treatment to improve symptom control and quality of life11. Recent research has revealed that, contrary to the general belief, vasomotor disorders are triggered by physical exercise24, and intracoronary testing is superior to clinical suspicion for their diagnosis20. Establishing the presence of INOCA at the time of ICA may avoid additional diagnostic tests, thereby reducing healthcare costs252627.
Based on the substantial improvement in diagnostic yield and the impact on clinical decision-making, as discussed above, we believe that application of the predefined AID strategy should be considered in all patients with CCS referred for ICA. Our proposal is that clinical and interventional cardiologists integrate clinical and invasive data for decision-making as part of an Ischaemia Team. Overall, intracoronary instrumentation was performed in 74.8% of patients to investigate obstructive and non-obstructive causes of ischaemia. When INOCA was suspected, operator adherence to testing the endothelium-dependent (acetylcholine) and -independent (adenosine) pathways was very high (around 97% in both cases) (Supplementary Table 10). In agreement with previous studies, complications were extremely rare and were successfully managed in the catheterisation laboratory2829.
Limitations
In aiming for a widespread applicability of the AID strategy and its integration into the workflow of the catheterisation laboratory, several simplifications were introduced in the diagnostic algorithm. First, patients with angiographically or functionally severe stenoses did not undergo functional testing to rule out INOCA, even though both conditions may occasionally coexist. Currently, pressure guidewire interrogation of angiographically severe stenoses is not recommended in clinical practice guidelines. Second, in agreement with consensus documents15, intracoronary testing for INOCA was performed preferentially in the left coronary artery. Third, during acetylcholine testing, assessment of endothelial function − combining mechanical infusion of acetylcholine and quantitative angiography to accurately assess changes in vessel diameter, as suggested elsewhere − was not performed30. Fourth, a simplified washout of antianginal medication (>12 hours before ICA) was permitted on the grounds of persistent symptoms under such treatment.
Conclusions
The application of a structured invasive diagnostic strategy in patients with CCS referred for ICA, compared with ICA alone, was associated with a 2.6-fold increase in the identification of a cause for myocardial ischaemia, which, very frequently, was of a non-obstructive origin. The information delivered by the AID strategy had a major impact on the final therapeutic plan for patients with obstructive and non-obstructive myocardial ischaemia.
Impact on daily practice
There is a large discrepancy between the invasiveness of invasive coronary angiography (ICA) and the limited diagnostic information it delivers in chronic coronary syndromes. The advanced invasive diagnosis strategy is a compendium of current recommendations by European and American clinical practice guidelines which allows the identification of an actionable cause of myocardial ischaemia in more than 80% of patients. Ischaemia with non-obstructive coronary arteries, which is the most prevalent cause of myocardial ischaemia, cannot be diagnosed based on ICA or clinical information alone.
Acknowledgements
We thank Mrs Silvia Travieso for the image editing in this manuscript.
Funding
The AID-ANGIO study was sponsored by the Fundación Interhospitalaria para la Investigación Cardiovascular (Madrid, Spain), which receives unrestricted research support from Abbott.
Conflict of interest statement
A. Jerónimo is supported by Sociedad Española de Cardiología through a mobility grant (SEC/PRS-MOV-INT 24). N. Gonzalo has received speaker and consultancy fees from Abbott, Boston Scientific, and Philips. J. Escaned is supported by the Intensification of Research Activity project INT22/00088 from Spanish Instituto de Salud Carlos III; and declares having served as speaker and advisory board member for Abbott and Philips. The other authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.