Cory:
Unlock Your AI Assistant Now!
Abstract
BACKGROUND: Controlled antegrade and retrograde subintimal tracking (CART) is rarely performed in contemporary chronic total occlusion (CTO) percutaneous coronary intervention (PCI).
AIMS: We aimed to analyse the indications, procedural characteristics, and outcomes of CART at a high-volume CTO programme.
METHODS: We included all patients undergoing a retrograde CTO PCI in which CART was performed at our institution between January 2019 and November 2023. The primary endpoint was technical success.
RESULTS: Of 1,582 CTO PCI, the retrograde approach was performed in 603 procedures (38.1%), and CART was used in 45 cases (7.5%). The mean age was 69.1±10.3 years, 93.3% were male, and prior coronary artery bypass graft surgery was present in 68.9%. The most common target CTO vessel was the right coronary artery (48.9%). Anatomical complexity was high (Multicentre CTO Registry of Japan [J-CTO] score of 3.6±0.9). The most common collateral used for CART was a saphenous vein graft (62.2%). Advanced calcium modification was required in 15.6% of cases. CART was successful in 73.3%. Technical and procedural success was 82.2%. Coronary perforation was diagnosed in 4 subjects (8.9%), but only 1 patient (2.2%) suffered tamponade and required pericardiocentesis. No other in-hospital major adverse cardiac events were diagnosed.
CONCLUSIONS: CART is a useful technique in selected, very complex CTOs tackled with the retrograde approach. Success rates were high, while complication rates were low, considering the high anatomical complexity and baseline patient risk.
The retrograde approach has allowed a remarkable improvement in the success rates of chronic total occlusion (CTO) percutaneous coronary intervention (PCI) over the last 20 years12. After collateral channel crossing, the most crucial aspect of the retrograde approach is creating the connection between the antegrade and retroÂgrade systems. Currently, the most common technique to achieve this goal is reverse controlled antegrade and retrograde subintimal tracking (reverse CART)3, which gained widespread adoption after the introduction of the Corsair (Asahi Intecc) microcatheter in 20101. This technique involves the inflation of a balloon over an antegrade guidewire, followed by retrograde crossing of the occlusion into the antegrade guide. However, in a non-negligible proportion of cases, this manoeuvre fails to create a connection between the retrograde and antegrade gear or is impossible to perform (e.g., aorto-ostial CTO, excessive tortuosity of the retrograde channel with subsequent inability to torque retrograde wires, impenetrable CTO). In this context, the original CART technique (which involves retrograde ballooning of the occlusion followed by antegrade wiring of the distal true lumen)4 might represent a useful alternative. However, CART is currently the less utilised (from 2.0% to 10.4%) retrograde crossing technique across large multicentre registries356. Moreover, no recent study has analysed the indications, procedural characteristics, and outcomes of this technique. The aim of this study is to fill this gap in knowledge.
Methods
STUDY POPULATION
All patients who underwent CTO PCI between January 2019 and November 2023 at our high-volume, three-operator programme (University of Washington Medical Center, Seattle, WA, USA) were screened for inclusion. Cases in which the retroÂgrade approach was performed and CART was attempted represented the study population. This study was approved by our institutional review board.
DEFINITIONS
CTO was defined according to the CTO Academic Research Consortium definition (absence of antegrade flow through an occlusive lesion [100% stenosis] with a presumed or documented duration of ≥3 months)7.
CART success was defined as the antegrade crossing of a wire into the distal true lumen, following retrograde balloon inflation at the occlusion level. Technical success was defined as the successful recanalisation of the CTO vessel with <30% residual stenosis and a final Thrombolysis in Myocardial Infarction 3 flow8. Procedural success was defined as technical success in the absence of in-Âhospital major adverse cardiac events (MACE: death, myocardial infarction9, tamponade requiring pericardiocentesis or surgery, stroke, or recurrent symptoms requiring urgent repeat target vessel revascularisation with PCI or surgery)8. Calcification was assessed by angiography and defined as mild (spots), moderate (involving ≤50% of the reference lesion diameter), or severe (involving ≥50% of the reference lesion diameter).
To evaluate CTO anatomical complexity, we calculated the Multicentre CTO Registry of Japan (J-CTO) score as described by Morino et al10, and the Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (PROGRESS-CTO) anatomical score as described by Christopoulos et al11. The PROGRESS-CTO complication scores were calculated as described by Simsek et al12, and the PROGRESS-CTO perforation score as described by Kostantinis et al13.
STATISTICAL ANALYSIS
Continuous variables are presented as mean±standard deviation. Categorical variables are presented as absolute numbers and percentages. The Chi-square test was used for comparisons between categorical variables.
Results
Of a total of 1,582 CTO PCI performed during the study period, retrograde crossing was attempted in 603 cases (38.1%). CART was performed in 45 procedures (7.5% of retrograde cases).
BASELINE CLINICAL CHARACTERISTICS
The baseline clinical characteristics of the study population are summarised in Table 1. The mean age was 69.1±10.3 years, 93.3% of the patients were male, and the mean left ventricular ejection fraction was 53.6±10.1%. There was a high prevalence of comorbidities with almost half of the population having diabetes (48.9%) and the vast majority having prior PCI (84.4%) and prior coronary artery bypass grafting (CABG: 68.9%).
Table 1. Clinical characteristics of patients undergoing CART.
| Variables | n=45 |
|---|---|
| Age, years | 69.1±10.3 |
| Male | 42 (93.3) |
| Hypertension | 44 (97.8) |
| Dyslipidaemia | 41 (91.1) |
| Diabetes mellitus | 22 (48.9) |
| Atrial fibrillation | 8 (17.8) |
| Prior PCI | 38 (84.4) |
| Prior CABG | 31 (68.9) |
| eGFR, ml/min/1.73 m2 | 55.5±10.4 |
| Dialysis | 1 (2.2) |
| Left ventricular ejection fraction, % | 53.6±10.1 |
| Data are presented as n (%) or mean±standard deviation. CABG: coronary artery bypass grafting; CART: controlled antegrade and retrograde subintimal tracking; eGFR: estimated glomerular filtration rate; PCI: percutaneous coronary intervention | |
ANGIOGRAPHIC AND PROCEDURAL DATA
The angiographic characteristics of the study population are summarised in Table 2. The most common target CTO vessel was the right coronary artery (48.9%). There was a high prevalence of blunt stump (93.3%), proximal cap ambiguity (93.3%), tortuosity (44.4%), lesion length >20 mm (95.6%), and previously unsuccessful attempts (28.9%). Accordingly, the overall anatomical complexity was very high (J-CTO score 3.6±0.9 and PROGRESS-CTO anatomical score 1.9±0.7). Importantly, the risks of complications as assessed with the PROGRESS-CTO complication scores were high (4.8±0.7 for MACE, 3.0±0.7 for death, 3.8±0.5 for pericardiocentesis, 1.8±0.7 for acute myocardial infarction [MI], and 4.6±0.5 for perforation). These corresponded to an average risk of MACE of 5.1%, 1.5% for death, 3.2% for pericardiocentesis, 1.2% for MI. Moderate/severe CTO calcification was present in 95.6% of patients, and 7 (15.6%) of them required aggressive plaque modification: rotational atherectomy was performed in 4 (8.9%), laser atherectomy in 2 (4.4%), and intravascular lithotripsy (IVL) in 1 (2.2%). The mean contrast volume was 138±48 ml, fluoroscopy time was 59.5±22.3 min, air kerma was 1.1±0.6 Gy, and kerma area product was 158±95 Gy.cm2.
Table 2. Angiographic characteristics of patients undergoing CART.
| Variables | n=45 |
|---|---|
| CTO vessel | |
| Left anterior descending | 13 (28.9) |
| Circumflex | 10 (22.2) |
| Right coronary | 22 (48.9) |
| Moderate/severe proximal tortuosity | 30 (66.7) |
| Proximal cap ambiguity | 42 (93.3) |
| Blunt stump | 42 (93.3) |
| Length >20 mm | 43 (95.6) |
| Tortuosity | 20 (44.4) |
| Moderate/severe calcification | 43 (95.6) |
| Retry | 13 (28.9) |
| In-stent CTO | 11 (24.4) |
| J-CTO score | 3.6±0.9 |
| J-CTO score ≥2 | 44 (97.8) |
| PROGRESS-CTO anatomical score | 1.9±0.7 |
| PROGRESS-CTO MACE score | 4.8±0.7 |
| PROGRESS-CTO death score | 3.0±0.7 |
| PROGRESS-CTO pericardiocentesis score | 3.8±0.5 |
| PROGRESS-CTO MI score | 1.8±0.7 |
| PROGRESS-CTO perforation score | 4.6±0.5 |
| Data are presented as n (%) or mean±standard deviation. CART: controlled antegrade and retrograde subintimal tracking; CTO: chronic total occlusion; J-CTO: Multicentre CTO Registry of Japan; MACE: major adverse cardiac events; MI: myocardial infarction; PROGRESS-CTO: Prospective Global Registry for the Study of Chronic Total Occlusion Intervention | |
CART TECHNIQUE CHARACTERISTICS
CART was used as the primary retrograde crossing strategy in 42.2% of cases. CART indications were impenetrable CTO in the antegrade direction (86.7%), failed reverse CART (28.9%), and flush aorto-ostial occlusion (11.1%) (Figure 1). CART was performed with over-the-wire balloons in 15.6%, while the remainder were performed with conventional monorail balloons. The most common balloon size was 3.0 mm (40.0%), but a wide variety of balloon sizes were used (ranging from 1.5 to 4.0 mm) (Figure 2). The collaterals used for CART were saphenous vein grafts (SVG) (62.2%), septal collaterals (24.4%), contralateral epicardial collaterals (6.7%), and ipsilateral epicardial collaterals (6.7%) (Figure 3). Excluding cases where epicardial collaterals were used for the retrograde approach, collateral (septal or graft) predilatation prior to performing CART was necessary in 6/39 cases (15.4%).
CART was successful in 33 (73.3%) cases. Even when it was not successful (12 cases), CART facilitated advancing retroÂgrade gear to successfully perform reverse CART in 5 cases (41.7%). Figure 4 presents a typical case example of CART.
Analysing the outcomes of our cohort according to the collateral channel used, we found that technical and procedural success was achieved in 24/28 patients (85.7%) in the SVG group and in 13/17 patients (76.5%) in the non-SVG group (septal and epicardial collaterals; p=0.43).
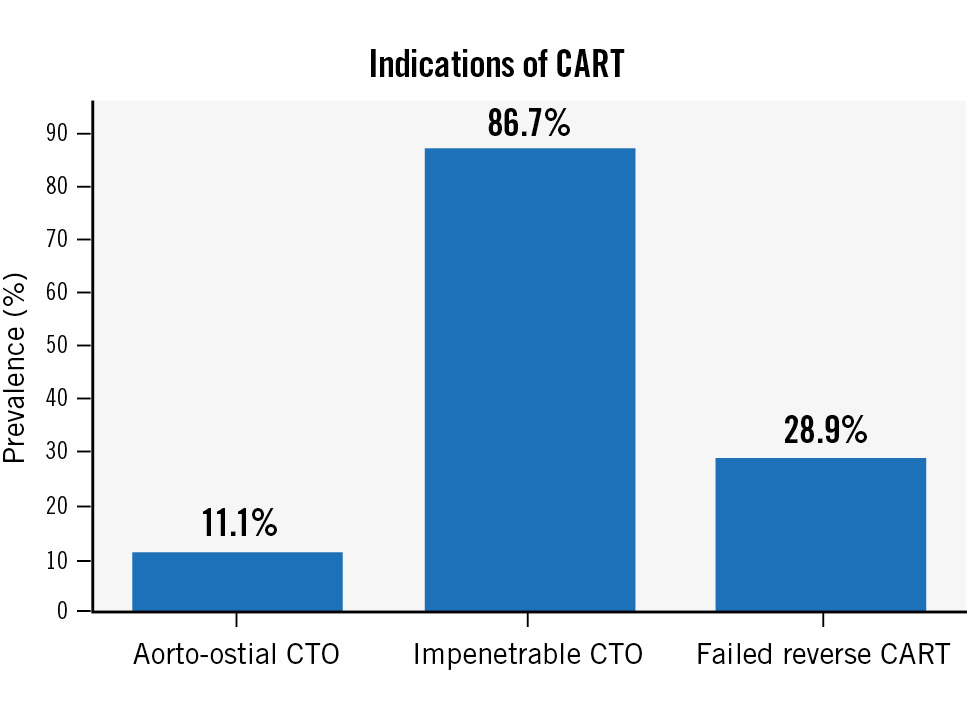
Figure 1. Indications of CART. CART: controlled antegrade and retrograde subintimal tracking; CTO: chronic total occlusion
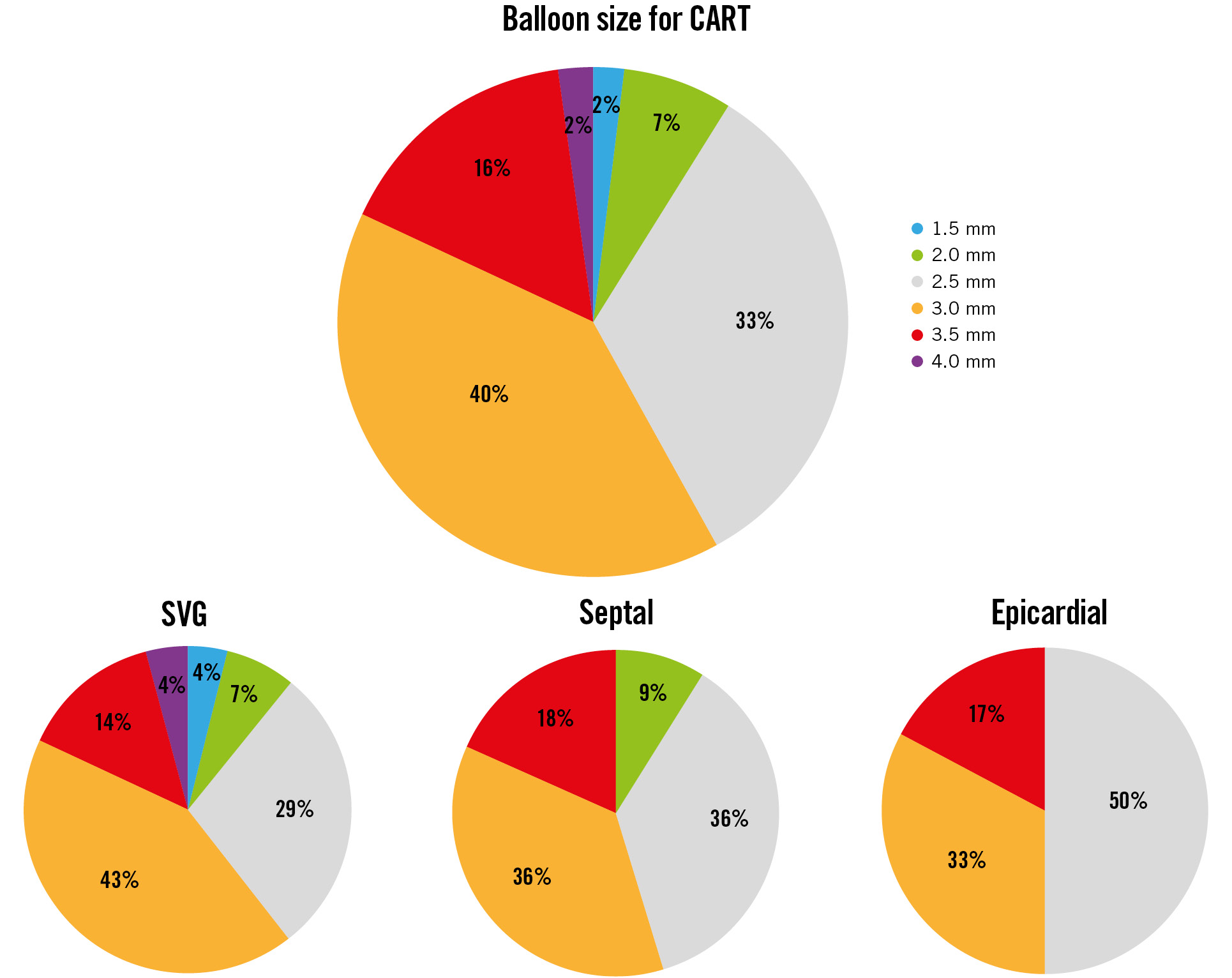
Figure 2. Balloon size used for CART. CART: controlled antegrade and retrograde subintimal tracking; SVG: saphenous vein graft
Figure 3. Collaterals used for CART. CART: controlled antegrade and retrograde subintimal tracking; SVG: saphenous vein graft
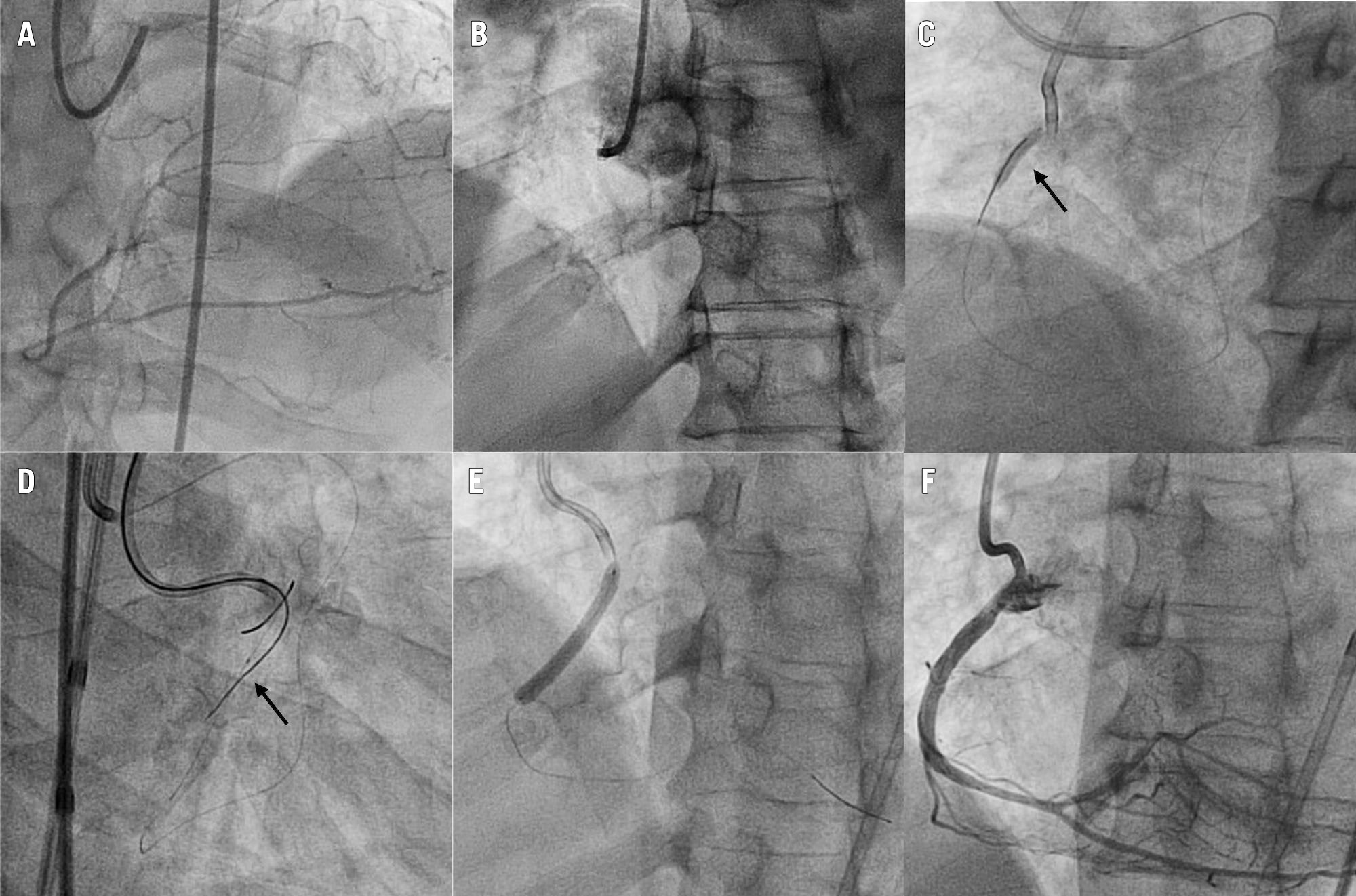
Figure 4. Case example: CART for flush ostial CTO of the right coronary artery. A) Extensive septal collateralisation from the left anterior descending artery. B) Flush ostial RCA CTO. C) Using an antegrade AL 0.75 and a retrograde EBU 3.5 guide set-up, a 3.0x20 mm balloon (arrow) is advanced from retrograde via the septal collaterals and inflated in the proximal RCA. D) After balloon deflation, a Gladius Mongo (Asahi Intecc) (arrow) can be advanced antegradely into the distal true lumen. E) Stenting. F) Final angiographic result. AL: Amplatz left; CART: controlled antegrade and retrograde subintimal tracking; CTO: chronic total occlusion; EBU: Extra Backup; RCA: right coronary artery
IN-HOSPITAL OUTCOMES
In-hospital outcomes are presented in Table 3. Both technical and procedural success were observed in 37 patients (82.2%). Four patients (8.9%) suffered coronary perforations: two (4.4%) were Ellis type 1 perforations of the distal vessel and were successfully treated with balloon occlusion and protamine; the remaining two (4.4%) were Ellis type 3 perforations of the target CTO vessel which required covered stents. One of these two patients (2.2%) suffered tamponade, which required pericardiocentesis. There were no in-hospital deaths or other MACE.
Table 3. Clinical outcomes of patients undergoing CART.
| Variables | n=45 |
|---|---|
| CART success | 33 (73.3) |
| Technical success | 37 (82.2) |
| Procedural success | 37 (82.2) |
| Coronary perforation | 4 (8.9) |
| MACE | 1 (2.2) |
| Death | 0 (0) |
| MI | 0 (0) |
| Tamponade requiring pericardiocentesis | 1 (2.2) |
| Stroke | 0 (0) |
| Urgent revascularisation | 0 (0) |
| Data are presented as n (%). CART: controlled antegrade and retrograde subintimal tracking; MACE: major adverse cardiac events; MI: myocardial infarction | |
Discussion
The main findings of our study are summarised in the Central illustration: 1) CART was used in 7.5% of retrograde CTO PCI; 2) despite high lesion complexity, CART, technical, and procedural success rates were high (73.3%, 82.2%, and 82.2%, respectively); 3) CART was performed via an SVG in almost two-thirds of cases; 4) despite the high complexity of these patients and lesions, the procedures were remarkably safe, with no deaths and lower than estimated overall procedural complications.
To the best of our knowledge, this is the first report on the indications, procedural characteristics, and outcomes of CART in contemporary retrograde CTO PCI. After its introduction in 2006 by Surmely et al4, CART was initially used with good results14. This technique was successful in 40.8% of retrograde CTO recanalisations in a single-centre report by Rathore and colleagues14. However, the retrograde approach evolved over the following years, and new devices were introduced. In particular, 2010 saw the introduction of the Corsair microcatheter which, with its ability to dilate retrograde channels, allowed a remarkable increase in the success rates of retrograde CTO recanalisation. This was mainly mediated by the introduction of reverse CART: balloon dilatation of the occlusion could now be performed antegradely, as retrograde wire manipulation and collateral channel and occlusion crossing were greatly facilitated by the use of dedicated microcatheters1. As a consequence, CART use dropped significantly, and reverse CART became the dominant retrograde CTO crossing technique356.
Nowadays CART is the least used technique in the PROGRESS-CTO3, EuroCTO5, and Japanese6 registries, comprising 2.0%, 10.4%, and 4.6% of all retrograde cases, respectively. In our series, CART was used in a higher proportion of cases (7.5%), compared with the PROGRESS-CTO and Japanese registries, and slightly less often than in the EuroCTO experience. In fact, despite the generalised decrease in its use, CART remains a useful technique in certain angiographic scenarios, such as impenetrable CTO in the antegrade direction (86.7% in our series), failure of reverse CART (28.9%), and aorto-ostial occlusions (11.1%). Another possible indication is when the operator runs out of retrograde microcatheter length before reaching the antegrade system (e.g., after reverse CART). Although this issue is mitigated by the systematic use of short retrograde guides (90 cm or less) and antegrade guide catheter extensions (and we did not encounter this situation in our practice), CART would be a valuable option in such scenarios.
Bypass grafts facilitate the retrograde approach, and this is particularly relevant in case balloons must be advanced through the collateral channels. Indeed, prior CABG was present in 68.9% of cases and SVGs were the most common (62.2%) retrograde conduits in our series. This differs from general retrograde CTO PCI series, where septal collaterals represent the most frequently used channels (~60% of cases)356. The markedly higher prevalence of CABG in our series (68.9% vs 15.4-42.5%356) might also explain the slightly higher prevalence of males (93.3%) compared with data from the literature (81-85%)1516.
However, using SVGs as retrograde conduits is not always ideal, specifically in case of steep angulation (>90 degrees) of the distal graft anastomosis. In such a scenario, the balloon shaft might not be able to negotiate the angle, with subsequent prolapse of the retrograde wire, or sometimes balloon shaft kink and subsequent inability to inflate the balloon.
The CART success rate was 73.3% in our study, which is higher than previously reported14, and is likely due to the current availability of superior microcatheters and wires, as well as the fact that experience with the retrograde approach has matured over the last 15 years. In almost half of the cases where CART failed, it still facilitated subsequent successful attempts at reverse CART by modifying the occlusive plaque. We found high rates of technical and procedural CTO PCI success (82.2% for both), which is remarkable considering the elevated complexity of these occlusions (mean J-CTO score 3.6±0.9 and all but one patient had a J-CTO score ≥2). In addition, we only experienced 1 MACE (2.2%; due to tamponade) in our series, which is reassuring, considering the high baseline risk of our patient population as estimated with the PROGRESS-CTO complication scores12 (MACE risk was estimated at 5.1%, and tamponade requiring pericardiocentesis at 3.2%).
Another testimony to the high complexity of these lesions is provided by the higher use of plaque modification techniques (15.6%) compared to the literature. In the series by Xenogiannis et al17, Azzalini et al18, and Kostantinis et al19, rotational atherectomy was used in 3.2%, 3.5%, and 7.3% of patients, respectively. IVL has recently been introduced, and its use is rapidly increasing (3.4%)19. Laser atherectomy (which is used mainly for device-uncrossable plaques and whose availability is limited) is employed in 3.4% of cases19. In our experience, the dominant plaque modification technique was rotational atherectomy (8.9%), while laser atherectomy (4.4%) and IVL (2.2%) were used in the remainder.
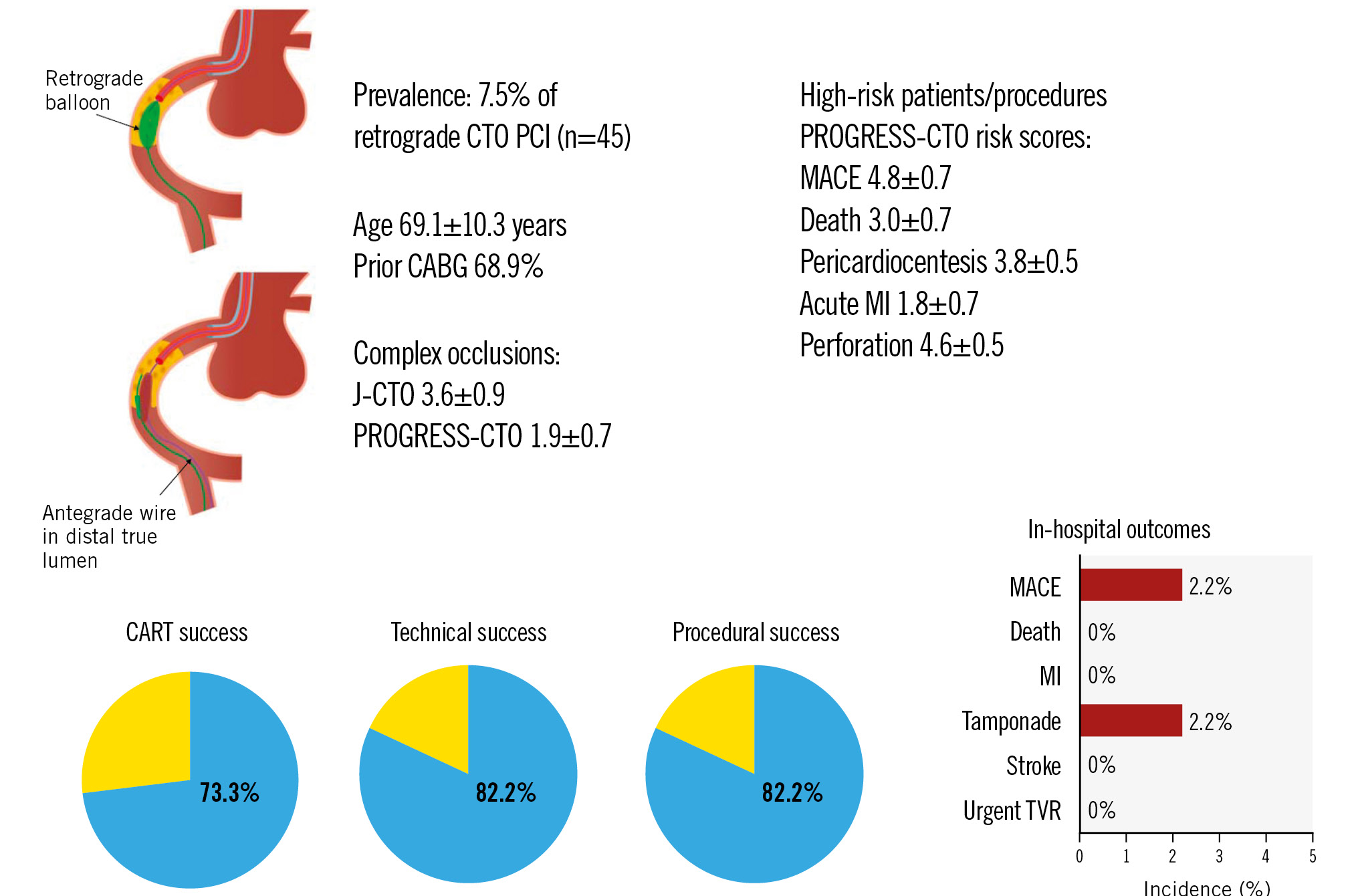
Central illustration. CART in contemporary CTO PCI. CABG: coronary artery bypass grafting; CART: controlled antegrade and retrograde subintimal tracking; CTO: chronic total occlusion; J-CTO: Multicentre CTO Registry of Japan; MACE: major adverse cardiac events; MI: myocardial infarction; PCI: percutaneous coronary intervention; PROGRESS-CTO: Prospective Global Registry for the Study of Chronic Total Occlusion Intervention; TVR: target vessel revascularisation
Limitations
Our study presents several limitations. First, it is an observational registry, with all the inherent bias ascribed to this kind of design. Second, clinical events were not adjudicated by an independent committee. Third, core laboratory adjudication of the angiograms was not available. Fourth, operators at our high-volume centre are highly experienced in CTO PCI, which could limit the applicability of these results to other centres/operators. In fact, advancing retrograde balloons through tortuous channels (particularly epicardial collaterals) is not devoid of risks, and the operator should be able to understand when excessive resistance to balloon advancement is heralding impending collateral perforation.
Conclusions
CART represents a valuable option to tackle very complex CTOs with the retrograde approach. In particular, this technique is useful in case of aorto-ostial occlusions, inability to torque retrograde wires due to excessive tortuosity of the retrograde channel, impenetrable CTOs from the antegrade direction, and failure of reverse CART. In our experience, CART was highly successful and allowed the recanalisation of very complex occlusions with low complication rates. Experience from contemporary multicentre registries is warranted to confirm and extend our findings.
Impact on daily practice
Reverse controlled antegrade and retrograde subintimal tracking (CART) is currently the most common crossing technique performed during retrograde chronic total occlusion (CTO) percutaneous coronary intervention (PCI). However, this technique fails or cannot be performed in a non-negligible proportion of cases. In such instances, CART is an appealing alternative. Our study provides a characterisation of CART in contemporary CTO PCI. CART was used in very challenging CTOs, most commonly via a saphenous vein graft. Success rates were high, and the safety profile of these procedures was favourable. Data from contemporary multicentre registries are needed to confirm and extend our findings.
Conflict of interest statement
K.E. Kearney received consulting fees from Abiomed, Abbott, Boston Scientific, Medtronic, Teleflex, and Cardiovascular Systems Inc. W.L. Lombardi received consulting fees from Asahi Intecc, Abiomed, Boston Scientific, Medtronic, Siemens, and Teleflex; receives royalties from Asahi Intecc; owns equity in Reflow Medical; and his spouse is a Reflow Medical employee. L. Azzalini received consulting fees from Teleflex, Abiomed, GE HealthCare, Abbott, Reflow Medical, and Cardiovascular Systems Inc; serves on the advisory board of Abiomed and GE HealthCare; and owns equity in Reflow Medical. S. Moscardelli has no conflicts of interest to declare.