Cory:
Unlock Your AI Assistant Now!
Quantitative flow ratio (QFR) has been validated as a wire-free, angiography-based method for the haemodynamic assessment of coronary stenoses1. Among the most important technical requirements for QFR calculation is the absence of arrhythmias, which imply variations in beat-to-beat coronary diastolic filling patterns. In previous studies, 8% of patients were excluded from QFR calculation due to arrhythmias2. No study has so far attempted to validate QFR in patients with arrhythmias. Therefore, we sought to compare the diagnostic performance of QFR in patients with arrhythmias against wire-based physiology indices such as fractional flow reserve (FFR) or non-hyperaemic pressure ratios (NHPR), which are regarded as gold standards in determining the haemodynamic relevance of coronary stenoses.
A total of 214 vessels (81 assessed with FFR, 133 with NHPR) in 161 consecutive patients with chronic coronary syndrome and arrhythmias (defined as atrial fibrillation [AFib] or extrasystole >20% of beats) during coronary angiography who had undergone assessment of at least 1 stenosis with FFR or NHPR across 3 European sites were retrospectively included. These measures were not included in prior studies. The presence of arrhythmia at the time of angiography was mandatory, either in terms of documented AFib or at least 20% extrasystole burden. Furthermore, results were compared with a previously published control cohort of patients without arrhythmias2.
The study was approved by local ethics committees. QFR was measured with dedicated software (QFR v.2.1.44.4 [Medis Medical Imaging]), as previously detailed3, by experienced analysts blinded to the FFR/NHPR assessments.
The diagnostic accuracy of QFR was assessed by receiver operating characteristic (ROC) area under the curve (AUC) and compared with wire-based physiology as the gold standard. The ROC AUC was also assessed through subgroups prespecified in the study protocol, including arrhythmia type, lesion location (left anterior descending artery [LAD] vs other vessels) and type of invasive assessment. No correction was performed for multiple lesions within individual patients. Statistical significance was defined by p≤0.05. Analyses were performed using SPSS Statistics, version 26.0 (IBM).
In the overall cohort (n=214 vessels), the mean QFR was 0.860±0.094. Physiology-based ischaemia (i.e., FFR ≤0.80 or NHPR ≤0.89) was documented in 53 (24.8%) lesions. When compared with wire-based physiology, QFR showed an excellent diagnostic performance for detecting flow-limiting coronary lesions with an AUC of 0.931 (95% confidence interval [CI]: 0.889-0.974; p<0.001) (Figure 1A). The established QFR cutoff of 0.80 yielded 83.0% sensitivity, 92.5% specificity, and 78.6% positive and 92.5% negative predictive values. The diagnostic accuracy of QFR in this population was comparable (p=0.990) with findings obtained in a previously published cohort of patients without arrhythmias (AUC: 0.932, 95% CI: 0.902-0.962)2. The average flow velocity (16.2±6.0 cm/s) was slightly lower compared with previously analysed vessels in patients without arrhythmias (17.8±7.0 cm/s; p=0.03)2. Prespecified subgroup analyses revealed consistent findings across patients with or without AFib or LAD or non-LAD lesions (Figure 1B). A significant interaction between QFR diagnostic accuracy and the type of wire-based assessment was found (AUC for lesions explored with FFR: 0.997, 95% CI: 0.988-1.000; AUC for NHPR: 0.855, 95% CI: 0.740-0.970; p for interaction=0.002), suggesting that QFR is a better predictor of FFR than NHPR4 (Figure 1B).
To the best of our knowledge, this is the first study demonstrating the excellent diagnostic accuracy of QFR among patients with cardiac arrhythmias. This confirms the preliminary findings from a previous small study involving a subset of 25 lesions from 22 AFib patients4. Our findings are reassuring on the previously raised concerns of the impact of arrhythmia on diastolic coronary filling, which in turn might affect the reliability of the three-dimensional vessel reconstruction necessary for QFR computation. The slightly lower flow velocity, compared to similar patients without arrhythmias, did not affect the diagnostic accuracy of QFR in our study.
The diagnostic accuracy of QFR remained consistent irrespective of arrhythmia type and the involved vessel (LAD vs non-LAD). The enhanced association of QFR with FFR rather than NHPR values may be explained by the increased beat-to-beat variability and limited reproducibility of NHPR compared with FFR in patients with AFib5, but this also fits with prior data showing a higher correlation of QFR with FFR rather than with NHPR4.
These findings should be interpreted in light of some limitations. Our study is a retrospective data analysis, and we did not collect patient outcomes. Therefore, a prospective validation study remains desirable. In spite of a very high diagnostic accuracy in both AFib (AUC: 0.906) and extrasystole (AUC: 0.956) patients, the study population was predominantly composed of AFib patients; therefore, generalisability of the findings to patients with extrasystole might require further investigation. We did not include a matched cohort of patients who had undergone wire-based assessments without arrhythmias. However, we compared the observed diagnostic accuracy of QFR in arrhythmia patients with prior findings obtained in a comparable patient cohort.
In conclusion, we found that QFR accurately predicts wire-free coronary lesion measures for haemodynamic relevance in patients with atrial fibrillation or extrasystole.
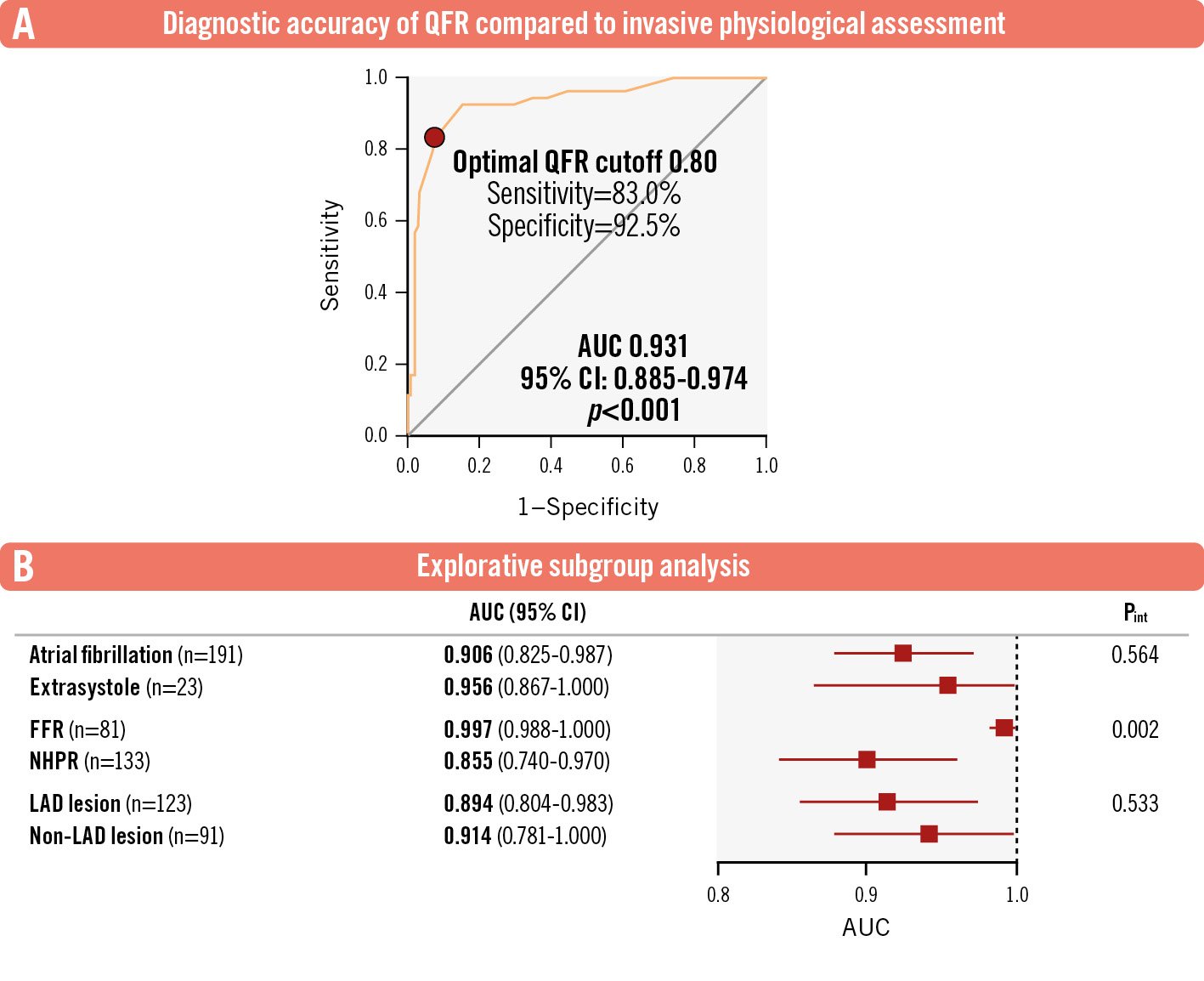
Figure 1. Diagnostic accuracy of quantitative flow ratio (QFR) in patients with arrhythmias. A) Graph depicting the excellent diagnostic accuracy of QFR in detecting the haemodynamic relevance of a coronary lesion (defined according to clinically established thresholds for FFR/NHPR) in patients with arrhythmias. B) Forest plot of AUCs for different subgroups. AUC: area under the curve; CI: confidence interval; FFR: fractional flow reserve; LAD: left anterior descending artery; NHPR: non-hyperaemic pressure ratio; Pint: p for interaction
Conflict of interest statement
M. Valgimigli has received personal fees from AstraZeneca; has received grants and personal fees from Terumo; and has received personal fees from Alvimedica/CID, Abbott, Daiichi Sankyo, Bayer, CoreFlow, Idorsia Pharmaceuticals Ltd, Departement Klinische Forschung of Universität Basel, Bristol-Myers Squibb, Medscape, Biotronik, and Novartis, outside the submitted work. The other authors have no conflicts of interest to declare relevant to the contents of this paper.