Cory:
Unlock Your AI Assistant Now!
Abstract
Background: The impact of final kissing balloon inflation (FKB) in patients treated with an upfront provisional strategy for coronary bifurcation lesions is controversial.
Aims: We aimed to assess the impact of FKB on patient- and lesion-oriented outcomes in a large real-world cohort.
Methods: The ULTRA-BIFURCAT registry was obtained by patient-level merging the BIFURCAT and ULTRA registries. Pairs of patients were generated with propensity score matching (PSM). The primary outcome of interest was major adverse cardiac events (MACE) − a composite of all-cause death, myocardial infarction (MI), target lesion revascularisation (TLR) or stent thrombosis. A lesion-oriented composite outcome (LOCO) − a composite of target vessel MI (TVMI) or TLR − along with each single component of MACE represented the secondary outcomes. Subgroup analyses included the site of bifurcation (unprotected left main [ULM] vs non-ULM), side branch involvement (true bifurcation vs non-true bifurcation), side branch diameter and lesion length. Follow-up was censored at 800 days.
Results: A total of 5,607 patients undergoing a provisional stenting technique were selected for the present analysis. PSM generated 1,784 pairs. Between the matched patients with FKB versus no FKB, no significant difference in MACE was observed (9.0% vs 8.6%; p=0.68). FKB was associated with a lower rate of the LOCO (1.9% vs 2.9%; p=0.04) compared to the no FKB group, driven by lower rates of TVMI (0.2% vs 0.5%; p=0.03) and TLR (1.8% vs 2.6%; p=0.14). These results were confirmed in the subgroups of patients treated for bifurcations with side branches with a diameter >2.5 mm and for true coronary bifurcation lesions.
Conclusions: Among patients treated for coronary bifurcation lesions with provisional stenting, FKB had no significant impact on MACE but was associated with a mild reduction in the incidence of the LOCO.
Coronary bifurcations are prone to atherosclerosis due to unique local flow patterns and shear stress, making them one of the most challenging lesion subsets in interventional cardiology, with lower procedural success and higher long-term adverse events123. Despite significant interest, treatment of bifurcations with percutaneous coronary intervention (PCI) remains contentious, with various strategies proposed4. Several randomised trials have shown no advantage of 2-stent techniques over 1-stent techniques, regardless of lesion type3567. The DKCRUSH-II trial found no significant clinical differences at 6 months but did find differences in target lesion revascularisation (TLR) and target vessel revascularisation at 12 months, favouring the 2-stent strategy after systematic follow-up angiography at 8 months8.
A network meta-analysis comparing 5 bifurcation PCI techniques showed that the double-kissing crush strategy is beneficial for bifurcation lesions with side branch lesion lengths >10 mm, while no significant differences emerged between provisional and 2-stent techniques in other settings9. The DEFINITION-II trial also indicated better outcomes with a systematic 2-stent approach in complex bifurcations10. Overall, evidence suggests that provisional stenting is preferred for most bifurcations, while 2-stent strategies are better for complex lesions involving significant side branches.
Final kissing balloon inflation (FKB), involving simultaneous post-dilatation of both branches, aims to improve stent apposition and procedural success111213. FKB is considered essential for all bifurcations requiring side branch treatment, minimising distortion in the main vessel (MV) stent and bifurcation carina14. The impact of FKB in real-world practice, particularly with provisional stenting, remains debated, with recent studies showing conflicting outcomes15161718. However, the effectiveness of FKB and prevention of its potential adverse effects also depend on the manner in which it is performed19.
This study investigates the clinical implications of FKB in a large, unselected cohort of patients undergoing PCI for coronary bifurcation lesions with an upfront provisional stenting.
Methods
Study design and patient population
The COBIS III Registry (ClinicalTrials.gov: NCT03068494) enrolled 2,648 patients with coronary bifurcation lesions undergoing PCI with second-generation drug-eluting stents (DES) from January 2010 to December 2014. The RAIN registry (ClinicalTrials.gov: NCT03544294) included 2,889 patients treated with very thin-strut DES for coronary bifurcations and/or unprotected left main (ULM) lesions from June 2015 to December 2017. The ULTRA registry (ClinicalTrials.gov: NCT05205148) involved 2,036 patients treated with ultrathin-strut DES for complex coronary lesions from September 2016 to August 2021, with 1,293 treated for bifurcations20. These datasets were merged to create a unified registry with 6,830 patients (Figure 1).
PCI was performed according to guidelines from the Korean Society of Interventional Cardiology and the European Society of Cardiology. All patients received aspirin and a P2Y12 inhibitor per guidelines, with dual antiplatelet therapy (DAPT) duration and other therapies at the operator’s discretion. Bifurcation lesions were classified per the Medina classification, with true bifurcations defined as Medina 1.1.1, 1.0.1, or 0.1.1 lesions21. Data were collected using a web-based system, and follow-up data were obtained from medical records, visits, or phone contact. For the present analysis, only patients treated with an upfront provisional stenting strategy were included, while patients treated with an upfront 2-stent strategy (regardless of the adopted strategy) were excluded. The registry was designed to capture these different scenarios by requiring practitioners to declare their strategy using specific labels: upfront provisional, conversion from provisional to 2-stent, or upfront 2-stent. These labels were derived from clinical records, angiographic procedures, and, if necessary, direct consultation with the physician who performed the procedure. The decision to implant a second stent in the side branch, within the context of the provisional stepwise approach, was at the operating physician’s discretion. The included cohort was further classified into two groups based on the performance of FKB. A propensity score matching (PSM) analysis was performed to adjust for baseline and procedural characteristics.
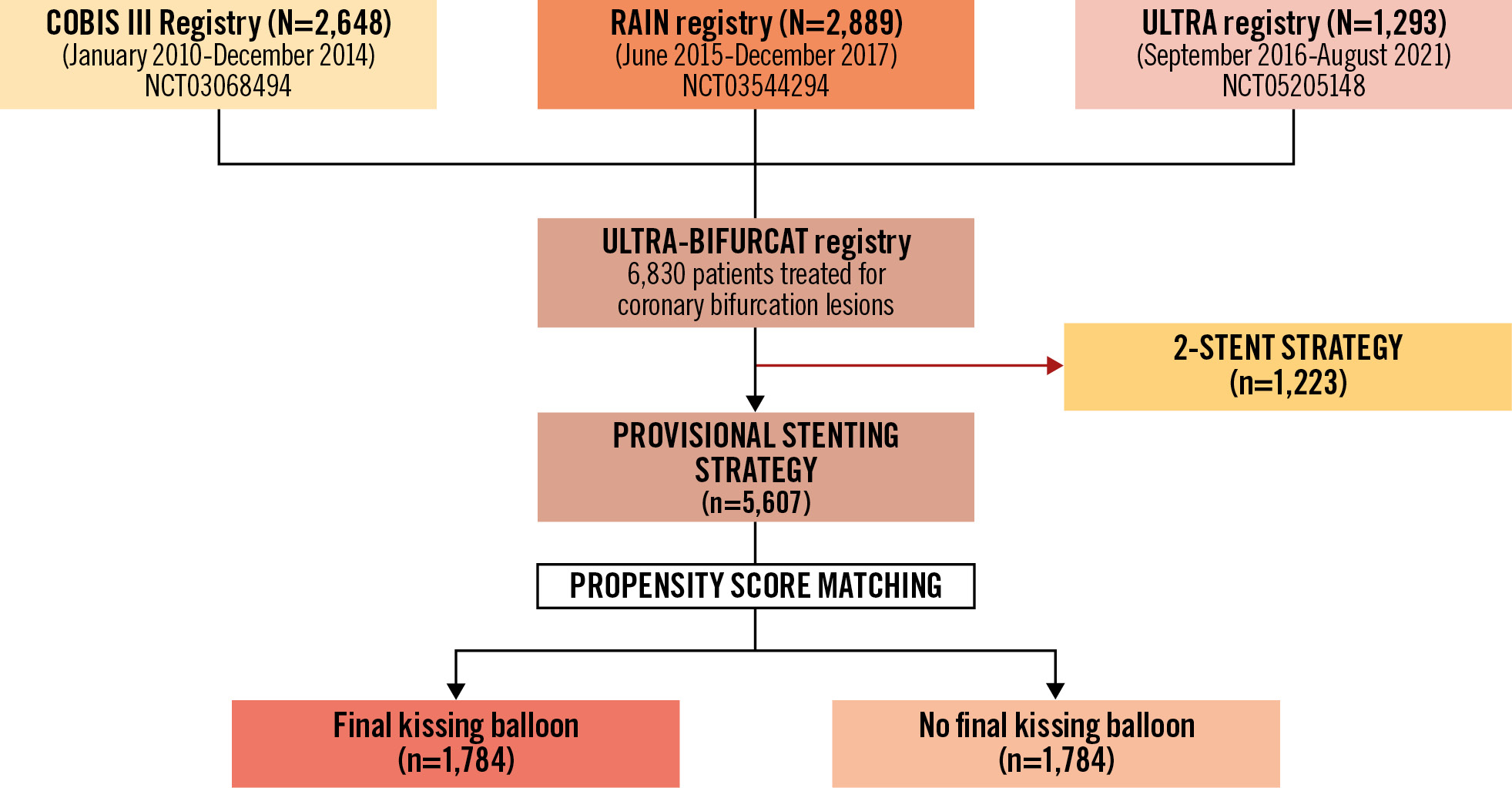
Figure 1. Study flowchart.
Clinical endpoints
The primary outcome was major adverse cardiac events (MACE): a composite of all-cause death, any myocardial infarction (MI), TLR or stent thrombosis (ST). A lesion-oriented composite outcome (LOCO) − a composite of target vessel MI (TVMI) or TLR − along with each component of MACE represented the secondary outcomes of interest. The target lesion was considered the treated coronary segment during the index procedure plus a distance of 5 mm from the stent edges or the balloon angioplasty site, applied for both the MV and side branch. The target vessel was defined as the entire major intervened coronary vessel, including side branches. TLR was defined as a repeat percutaneous intervention of the target lesion or bypass surgery of the target vessel performed for restenosis or other complications of the target lesion. TVMI was defined as an MI case with evidence of myocardial necrosis or direct evidence of invasive angiographic, electrocardiographic, or other imaging evidence supporting the involvement of the vascular territory of the previously treated target vessel22. Definitions of clinical endpoints used in the registries considered for this analysis are listed in Supplementary Appendix 1. Before PSM, a subgroup analysis was performed excluding patients who were ultimately treated with a 2-stent strategy. After PSM, subgroup analyses were performed according to the site of bifurcation (namely for bifurcations involving the ULM vs non-ULM), the involvement of a side branch (true bifurcations as per Medina definitions), side branch diameter, length of lesion and registries (COBIS III vs ULTRA and RAIN). All endpoints are patient based, reflecting the design of the registries to focus on overall clinical outcomes for the patients rather than individual lesion characteristics. Endpoints were primarily based on clinical outcomes. Routine angiographic follow-up was not performed for all patients; angiography was conducted as clinically indicated. Follow-up was censored at 800 days to ensure homogeneity among registries.
Statistical analysis
Continuous variables are expressed as mean±standard deviation or as median with interquartile range. Continuous variables were compared using the unpaired t-test or the Mann-Whitney U test in the prematched cohort and the paired t-test in the matched cohort. Categorical variables are reported as counts and percentages. Categorical variables were compared using Pearson’s χ2 test or Fisher’s exact test in the prematched cohort and the McNemar test in the matched cohort. To mitigate differences among patients included in the two subgroups of FKB versus no FKB, which are partially influenced by their inclusion in different registries across varying periods and potential selection bias, a propensity score (PS) was generated for each patient from a multivariable logistic regression model based on pretreatment covariates as independent variables with final kissing balloon inflation as a dependent outcome. Pairs of patients were derived using greedy 1:1 matching with a calliper of width equal to 0.2 of the standard deviation of the logit of the PS. The quality of the match was assessed by comparing selected pretreatment variables in PS-matched patients using the standardised mean difference, for which an absolute standardised difference of greater than 20% is suggested to represent meaningful covariate imbalance. All p-values<0.05 were considered to indicate statistical significance. Kaplan-Meier curves were generated in the PSM cohorts for the primary endpoint and compared with the log-rank test. All statistical analyses were performed using SPSS version 21 (IBM), and differences were considered significant at α=0.05.
Results
Of 6,830 patients included in the ULTRA-BIFURCAT registry, 5,607 were treated with an upfront provisional stenting strategy. Of these, 2,133 were treated with no FKB and 3,474 were treated with FKB (Figure 1). The baseline features of patients are listed in Table 1. Patients treated without FKB were characterised by a higher prevalence of common cardiovascular risk factors, such as hypertension, diabetes mellitus and dyslipidaemia, as compared to those treated with FKB. Patients in the no FKB group showed a higher prevalence of comorbidities such as chronic obstructive pulmonary disease (1.6% vs 0.9%; p<0.01), chronic kidney disease (17.1% vs 10.4%; p<0.001) and peripheral artery disease (2.3% vs 1.2%; p<0.001). Procedural and angiographic features are shown in Table 2. The use of intracoronary imaging was low overall but more frequent in the no FKB subgroup (34.3% vs 27.6%; p<0.001). The site and the complexity of the index bifurcation lesions were significantly different among the two groups, with more patients in the FKB group undergoing treatment of the distal left main artery (26.5% vs 18.4%; p<0.001) and for true coronary bifurcations (40.8% vs 36.3%; p=0.001). In the entire cohort, 82 patients were eventually treated with an additional side branch stent; this occurred more frequently in FKB group (1.8% vs 0.9%; p=0.005). PSM generated 1,784 pairs. Baseline and procedural features of the paired groups are summarised in Supplementary Table 1-Supplementary Table 2-Supplementary Table 3. A total of 1,142 (32%) of the selected patients were recruited in COBIS III, 1,764 (49%) in RAIN and 662 (18%) in ULTRA. No significant differences with respect to baseline characteristics were observed between the matched groups. Standardised mean differences of variables selected for the PSM are shown in Supplementary Table 4. Most patients were middle-aged (mean age 66.36±11.44 years old and 66.22±11.46 years old in the FKB and no FKB groups, respectively) and burdened by a relevant prevalence of cardiovascular risk factors. Left ventricular ejection fraction was, on average, preserved in both groups, and nearly half of both cohorts were treated for an acute coronary syndrome. The most frequently used DAPT regimen overall consisted of aspirin plus clopidogrel (up to 70% of patients) followed by aspirin and ticagrelor, with a median length of administration of 14.61±6.11 months, and there were no significant differences among the FKB versus no FKB PS-matched cohorts. As for the procedural features of the PS-matched cohorts, more than one-third of patients were treated for true coronary bifurcations (34.4% and 37.3% in the FKB and no FKB groups, respectively), with the left anterior descending/diagonal branches being the most frequent site of the bifurcation lesion (45.2% vs 48.9% in the FKB and no FKB groups, respectively). Both before and after PSM, XIENCE and XIENCE Alpine (both Abbott) were the most frequently implanted stents (up to 24%), followed by Orsiro (Biotronik; up to 23%) and Resolute/Resolute Onyx (Medtronic; up to 21%) (Supplementary Table 3).
Table 1. Baseline features.
| Overall (n=5,607) | FKB (n=3,474) | No FKB (n=2,133) | p-value | |
|---|---|---|---|---|
| Age, years | 66.00±11.35 | 65.87±11.29 | 66.23±11.46 | 0.24 |
| LVEF, % | 56.07±9.68 | 56.28±9.83 | 55.73±9.44 | 0.04 |
| Male | 4,311 (76.9) | 2,654 (76.4) | 1,657 (77.7) | 0.26 |
| Hypertension | 3,597 (64.2) | 2,146 (61.8) | 1,451 (68.1) | <0.001 |
| Hyperlipidaemia | 2,794 (49.8) | 1,628 (46.9) | 1,166 (54.7) | <0.001 |
| Diabetes | 1,746 (31.1) | 1,021 (29.4) | 725 (34.0) | <0.001 |
| Insulin dependent | 63 (1.1) | 23 (0.67) | 40 (1.9) | <0.001 |
| Smoker | 1,533 (27.4) | 965 (27.7) | 568 (26.6) | 0.06 |
| Previous smoker | 1,462 (26.1) | 929 (26.7) | 533 (25.0) | |
| Current smoker | 71 (1.3) | 36 (1.0) | 35 (1.6) | |
| CKD | 716 (13.0) | 354 (10.4) | 362 (17.1) | <0.001 |
| Previous PCI | 1,244 (22.2) | 738 (21.2) | 506 (23.7) | 0.03 |
| Previous CABG | 186 (3.3) | 108 (3.1) | 78 (3.7) | 0.27 |
| Previous MI | 975 (17.4) | 583 (16.8) | 392 (18.4) | 0.13 |
| Previous stroke | 53 (0.9) | 30 (0.9) | 23 (1.1) | 0.42 |
| Active cancer | 42 (0.7) | 19 (0.5) | 23 (1.1) | 0.02 |
| COPD | 65 (1.2) | 30 (0.9) | 35 (1.6) | 0.01 |
| History of major bleeding | 9 (0.2) | 2 (0.1) | 7 (0.3) | 0.01 |
| Multivessel disease | 521 (9.3) | 260 (7.5) | 261 (12.4) | <0.001 |
| PAD | 88 (1.6) | 40 (1.2) | 48 (2.3) | <0.001 |
| Indication for PCI | <0.001 | |||
| CCS | 983 (17.5) | 517 (14.9) | 466 (21.8) | |
| ACS | 2,427 (43.2) | 1,506 (43.9) | 897 (42.0) | |
| STE-ACS | 1,191 (21.2) | 792 (22.8) | 399 (18.7) | |
| NSTE-ACS | 1,236 (22.0) | 738 (21.2) | 498 (23.3) | |
| Other | 2,197 (39.2) | 1,427 (41.1) | 770 (36.1) | |
| Data are presented as mean±standard deviation or n (%). ACS: acute coronary syndrome; CABG: coronary artery bypass graft; CCS: chronic coronary syndrome; CKD: chronic kidney disease; COPD: chronic obstructive pulmonary disease; FKB: final kissing balloon inflation; LVEF: left ventricular ejection fraction; MI: myocardial infarction; NSTE-ACS: non-ST-segment elevation acute coronary syndrome; PAD: peripheral artery disease; PCI: percutaneous coronary intervention; STE-ACS: ST-segment elevation acute coronary syndrome | ||||
Table 2. Procedural features (overall population).
| Overall (n=5,607) | FKB (n=3,474) | No FKB (n=2,133) | p-value | |
|---|---|---|---|---|
| Arterial access | <0.001 | |||
| Radial | 3,722 (66.4) | 2,204 (63.4) | 1,518 (71.2) | |
| Femoral | 1,885 (33.6) | 1,270 (36.6) | 615 (28.8) | |
| Intracoronary imaging | 1,690 (30.1) | 939 (27.6) | 726 (34.3) | <0.001 |
| IVUS | 1,649 (29.6) | 934 (26.9) | 715 (33.5) | |
| OCT | 41 (0.6) | 23 (0.7) | 18 (0.8) | |
| Site of bifurcation | <0.001 | |||
| Distal LM | 1,311 (23.4) | 920 (26.5) | 391 (18.4) | |
| LAD-diag | 2,734 (48.8) | 1,683 (48.5) | 1,051 (49.3) | |
| LCx/OM | 1,077 (19.2) | 617 (17.8) | 460 (21.6) | |
| RCA/PDA-PL | 327 (5.8) | 203 (5.8) | 124 (5.8) | |
| Medina classification | <0.001 | |||
| 0.0.1 | 209 (3.7) | 110 (3.2) | 99 (4.7) | |
| 0.1.0 | 919 (16.5) | 657 (19.0) | 262 (12.3) | |
| 0.1.1 | 317 (5.7) | 197 (5.7) | 121 (5.7) | |
| 1.0.0 | 609 (10.9) | 322 (9.3) | 287 (13.5) | |
| 1.0.1 | 446 (8.0) | 250 (7.2) | 196 (9.2) | |
| 1.1.0 | 1,652 (29.6) | 948 (27.4) | 704 (33.1) | |
| 1.1.1 | 1,428 (25.6) | 971 (28.1) | 457 (21.5) | |
| True bifurcations | 2,192 (39.1) | 1,418 (40.8) | 774 (36.3) | 0.001 |
| Main branch diameter, mm | 3.15±0.57 | 3.16±0.60 | 3.13±0.51 | 0.02 |
| Main branch lesion length, mm | 25.27±11.42 | 25.40±11.72 | 25.08±10.92 | 0.31 |
| Side branch diameter, mm | 2.11±1.81 | 2.13±1.42 | 2.09±2.18 | 0.51 |
| Side branch lesion length, mm | 23.59±9.85 | 23.32±9.66 | 23.91±10.06 | 0.08 |
| Severe calcification | 189 (20.3) | 106 (22.1) | 83 (18.3) | 0.30 |
| Rotational atherectomy | 165 (2.9) | 60 (1.7) | 105 (4.9) | <0.001 |
| Diffuse disease | 1,748 (31.2) | 1,060 (30.5) | 688 (32.3) | 0.17 |
| Cardiogenic shock on admission | 14 (0.2) | 6 (0.2) | 8 (0.4) | 0.14 |
| Use of MCS | 0.57 | |||
| IABP | 4 (0.1) | 2 (0.1) | 2 (0.1) | |
| Impella | 2 (0.0) | 1(0.0) | 1 (0.0) | |
| Need for inotrope/vasopressors | 25 (0.4) | 11 (0.3) | 14 (0.6) | 0.27 |
| Additional side branch stent | 82 (2) | 63 (1.8) | 19 (0.9) | 0.005 |
| P2Y12 inhibitors | ||||
| Clopidogrel | 4,104 (73.6) | 2,612 (75.8) | 1,492 (70.2) | <0.001 |
| Ticagrelor | 1,455 (25.9) | 823 (23.9) | 622 (29.3) | |
| Prasugrel | 24 (0.4) | 13 (0.4) | 11 (0.5) | |
| DAPT duration, months | 15.46±6.80 | 16.36±7.18 | 14.00±5.86 | <0.001 |
| Data are presented as n (%) or mean±standard deviation. DAPT: dual antiplatelet therapy; diag: diagonal branch; FKB: final kissing balloon inflation; IABP: intra-aortic balloon pump; IVUS: intravascular ultrasound; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; MCS: mechanical circulatory support; OCT: optical coherence tomography; OM: obtuse marginal branch; PDA: posterior descending artery; PL: posterolateral branch | ||||
Outcomes
MACE occurred in 276 patients (7.9%) in the FKB group and 185 patients (8.7%) in the no FKB group (p=0.33). A significantly lower rate of MI was observed in the FKB group as compared with the no FKB group (1.8% vs 3.5%; p<0.001), partially driven by a lower rate of TVMI among patients in the FKB group (0.1% vs 0.7%; p<0.001). No significant differences between the two groups were observed with respect to all-cause death (FKB vs no FKB: 3.8% vs 4.3%; p=0.37) or TLR (FKB vs no FKB: 1.9% vs 2.4%; p=0.17). A numerically lower rate of ST, albeit not significant, was observed in the FKB group compared with patients not treated with FKB (0.7% vs 1.1%; p=0.06). As for the secondary composite endpoint of LOCO, a significantly lower rate was observed among patients treated with FKB as compared with those without FKB (1.9% vs 3.0%; p=0.013) (Table 3). After excluding patients with an additional side branch stent, the benefit of FKB persisted consistently for all outcomes (Supplementary Table 5).
After PSM, there were no significant differences in the primary composite outcome in the FKB and no FKB groups (9.0% vs 8.6%, respectively; p=0.68). Kaplan-Meier curves for the cumulative freedom from MACE are presented in Figure 2.
Patients treated with FKB were characterised by a significantly lower rate of any MI (2.0% vs 3.3%; p=0.02) and TVMI (0.1% vs 0.5%; p=0.03), and a lower, but not significant, rate of TLR (1.8% vs 2.6%; p=0.14) compared to those not treated with FKB. Overall, the LOCO occurred less frequently in the FKB group compared with the no FKB group (1.9% vs 2.9%; p=0.04).
No significant difference was observed between the two PS-matched cohorts with respect to all-cause death (5.1% vs 4.3%, in the FKB and no FKB groups, respectively; p=0.23). A marginally significant lower rate of ST was instead observed in the FKB group as compared with no FKB group (1.5% vs 0.6%, respectively; p=0.05) (Table 3).
Table 3. Long-term outcomes according to final kissing balloon inflation before and after propensity score matching.
| Outcomes | Crude analysis | Propensity score-matched analysis | ||||
|---|---|---|---|---|---|---|
| FKB (n=3,474) | No FKB (n=2,133) | p-value | FKB (n=1,784) | No FKB (n=1,784) | p-value | |
| MACE | 276 (7.9) | 185 (8.7) | 0.33 | 160 (9.0) | 153 (8.6) | 0.68 |
| All-cause death | 133 (3.8) | 92 (4.3) | 0.37 | 91 (5.1) | 76 (4.3) | 0.23 |
| Any MI | 64 (1.8) | 74 (3.5) | <0.001* | 36 (2.0) | 59 (3.3) | 0.02* |
| TLR | 66 (1.9) | 52 (2.4) | 0.17 | 33 (1.8) | 46 (2.6) | 0.14 |
| ST | 23 (0.7) | 24 (1.1) | 0.06 | 11 (0.6) | 22 (1.5) | 0.05* |
| TVMI | 3 (0.1) | 15 (0.7) | <0.001* | 2 (0.1) | 9 (0.5) | 0.03* |
| LOCO | 67 (1.9) | 63 (3.0) | 0.013* | 34 (1.9) | 52 (2.9) | 0.04* |
| Data are presented as n (%). *Indicates statistical significance. FKB: final kissing balloon inflation; LOCO: lesion-oriented composite outcome; MACE: major adverse cardiac events; MI: myocardial infarction; ST: stent thrombosis; TLR: target lesion revascularisation; TVMI: target vessel myocardial infarction | ||||||
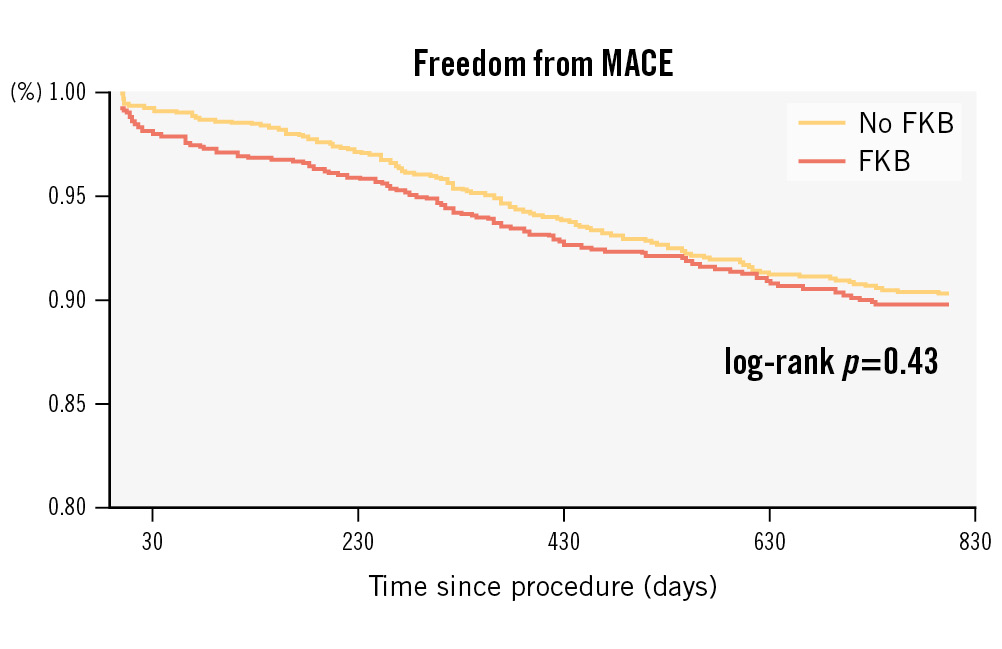
Figure 2. Kaplan-Meier analysis for freedom from MACE according to FKB in the propensity score-matched cohort. FKB: final kissing balloon inflation; MACE: major adverse cardiac events
Subgroup analyses
Results of the prespecified subgroup analysis, performed in the PS-matched cohorts, are graphically summarised in Figure 3. Among 1,279 patients treated for true coronary bifurcations (613 in the FKB group and 666 in the no FKB group), no significant differences were observed between the FKB and no FKB groups for the primary outcome (MACE: 9.1% vs 9.9%; p=0.64). FKB was associated with a lower rate of TLR (1.5% vs 3.2% in the FKB and no FKB groups, respectively; p=0.05) and of the LOCO (1.6% vs 3.6%; p=0.03). A lower rate of any MI was also observed in the FKB group compared with the no FKB group (2.1% vs 4.4%; p=0.02), while there were no significant differences for other secondary endpoints. Similar results were observed in the subgroup of patients treated for coronary bifurcations involving side branches with diameters >2.5 mm. A significantly lower rate of the LOCO was indeed observed among patients treated with FKB as compared with those without FKB (2.0% vs 4.4%; p=0.02). This difference was driven by significantly lower rates of TVMI (0.2% vs 1.5%; p=0.01) and lower, albeit not significant, rates of TLR (1.8% vs 3.3%; p=0.11). No significant differences were otherwise observed between FKB and no FKB in this subgroup with respect to the primary endpoint and other secondary outcomes. In the subgroup of patients treated for coronary bifurcations with side branch lesions >20 mm in length, no significant differences for any of the investigated outcomes were observed between FKB and no FKB. Among patients treated for bifurcations involving the unprotected left main, FKB was associated with a marginally significant reduction of ST (0.4% vs 1.7%; p=0.05), while no other significant differences were observed for the primary or other secondary endpoints of interest. Regarding analysis across different registries, FKB did not have an impact on MACE either for the COBIS III or the RAIN plus ULTRA registries (6% vs 8%; p=0.19, and 9% vs 10%; p=0.96, respectively), while the reduction of the LOCO was consistent (1.5% vs 3.6%; p=0.02, and 1.5% vs 3.1%; p=0.09, respectively).
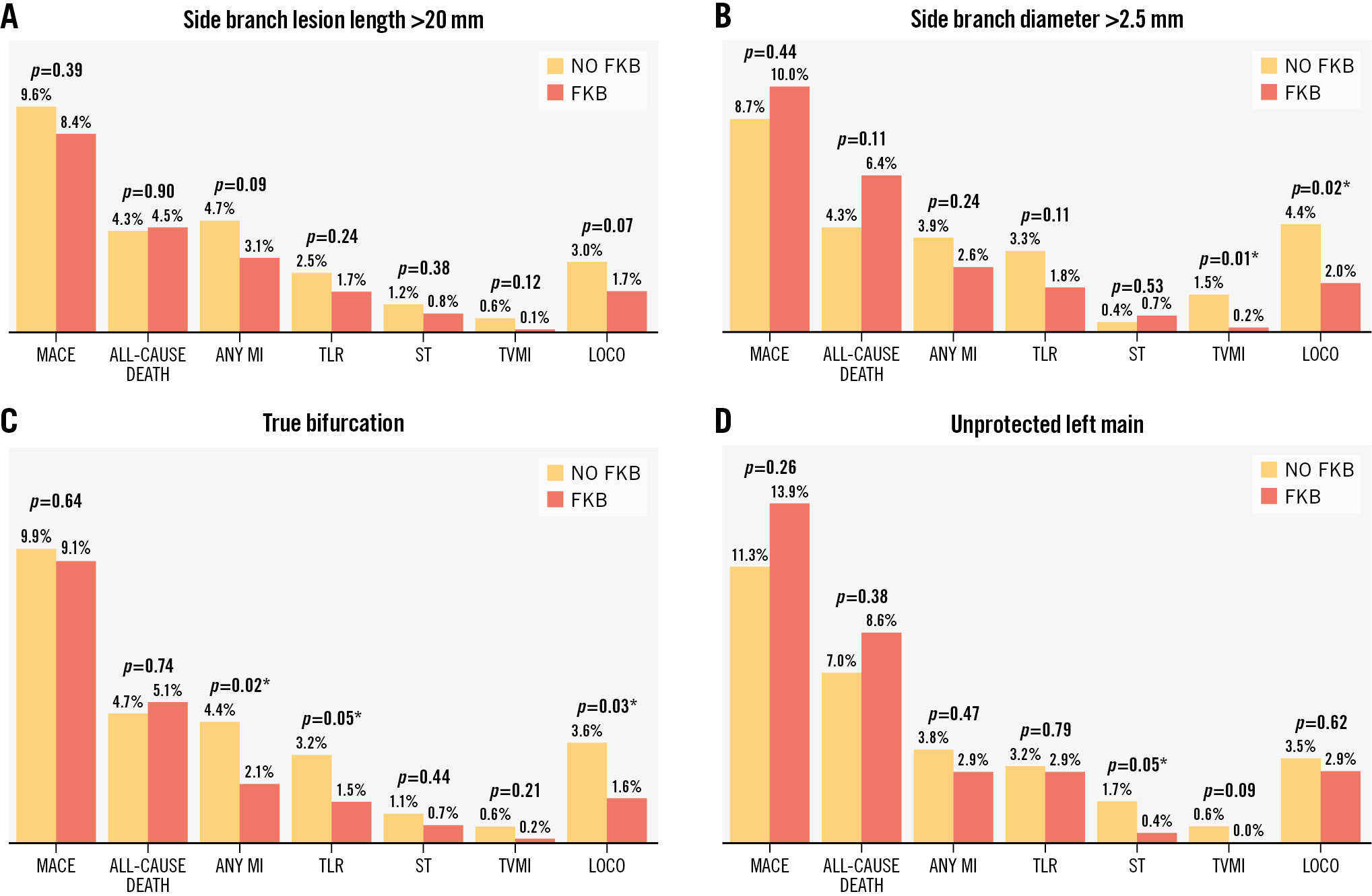
Figure 3. Subgroup analyses. Subgroup analyses performed in the PS-matched cohorts for side branch lesion length (A), side branch diameter (B), true bifurcation (C), and unprotected left main bifurcation (D). *Indicates statistical significance. FKB: final kissing balloon inflation; LOCO: lesion-oriented composite outcome; MACE: major adverse cardiac events; MI: myocardial infarction; ST: stent thrombosis; TLR: target lesion revascularisation; TVMI: target vessel myocardial infarction
Discussion
In this retrospective multicentre study, we assessed the impact of FKB in a large cohort of patients treated for coronary bifurcations using an upfront provisional stenting strategy. We generated 1,784 PS-matched pairs of patients and conducted event assessments over an 800-day follow-up period.
Our key findings are as follows (Central illustration):
• FKB did not significantly reduce MACE or all-cause mortality among patients treated with the provisional technique.
• FKB was associated with a reduction in a lesion-oriented composite outcome (TLR and TVMI) and a lower rate of any myocardial infarction compared to those not treated with FKB.
• The benefit of FKB was mainly seen in patients with side branches >2.5 mm in diameter and true coronary bifurcations.
The potential benefit of FKB with the provisional approach remains uncertain because of limited data. Although FKB has been considered effective for securing side branch patency after MV stenting23, recent studies have not shown clear clinical advantages for FKB in the 1-stent technique172425. In the COBIS III Registry, among 1,065 patients treated with a 1-stent technique, 329 were treated with FKB, while 736 were not. At a median follow-up of 22 months, most TLRs occurred in the MV rather than in the side branch, and no significant differences were observed between the groups in terms of rates of cardiac death, myocardial infarction, or stent thrombosis16. Similar findings were observed in the randomised CORPAL Kiss Trial over a 1-year follow-up26. In the Nordic Baltic Bifurcation Study III, 477 patients with a bifurcation lesion were randomised to receive FKB or not after MV stenting15. At the 6-month follow-up, the rates of MACE were similar (2.1% vs 2.5%; p=1.00). At the 8-month angiographic follow-up, there was a trend towards a lower rate of binary restenosis in the FKB group. Notably, FKB significantly reduced angiographic side branch restenosis, especially in true bifurcation lesions (7.6% vs 20.0%; p=0.02). Another meta-analysis confirmed that FKB significantly reduced the risk of side branch restenosis in the simple-strategy group27. However, some controversy regarding whether FKB reduces the risk of TLR still persists. Two reports indicated that the no-FKB strategy was associated with a lower risk of TLR compared with FKB while in the TAXUS PMS, FKB was an independent predictor of 3-year TLR1618. In contrast, the COBIS II study showed that rates of TLR were higher in the no FKB group than in the FKB group17. This study aimed to partially address the controversial evidence about the effectiveness of FKB in the context of provisional stenting. Taken together, our results align with the existing literature indicating that, over a medium-term follow-up, FKB may offer benefits in terms of lesion-associated outcomes without affecting “hard” clinical endpoints such as all-cause death or MACE151727. However, it should be noted that non-emergent TLR has been linked to all-cause mortality in a large meta-analysis, and a longer follow-up or larger sample size may reveal differences in hard clinical endpoints28.
It is worth noting that our study features a larger sample size and a generally longer follow-up compared to the above-mentioned registries and trials, which prevent direct comparisons. The ULTRA-BIFURCAT registry reflects real-world clinical practice across different centres and time periods, enhancing its generalisability. However, our findings might not be directly comparable to those from more controlled clinical trial settings, which often have strict inclusion criteria and planned angiographic follow-up.
While randomised controlled trials (RCTs) conducted thus far may not adequately reflect practice patterns in real-world clinical settings due to their small to medium sample sizes, limited follow-up periods, and strict protocols, we acknowledge that the observational, retrospective nature of our study and its reliance on multiple registries introduce potential biases and confounding factors (e.g., procedural and material changes over time, selection bias) that can only be partially managed with propensity score adjustment. To account for the heterogeneous scenarios of bifurcation lesions, several subgroup analyses were performed.
After PSM, more than one-third of patients were treated for true coronary bifurcations. Patients with true bifurcation lesions are known to be at a higher risk for procedural complications than patients with other types of bifurcation lesions21. As observed in our registry, more patients in the FKB group were treated for true coronary bifurcations. However, after PSM there was no significant difference in the primary outcome between the FKB and no FKB groups. Unlike the remainder of the population, both before and after propensity score matching, FKB was associated with a significantly lower rate of TLR, yet the absolute difference in TLR was relatively small. A lower rate of any MI and the LOCO was also observed in the FKB group as compared to the no FKB group, whereas no significant differences were found for other secondary endpoints.
The diameter and atherosclerotic burden of the side branch play a crucial role in managing bifurcation lesions. The side branch size, often called the “ostial” orifice, significantly impacts procedural success and long-term outcomes29. An appropriately sized side branch is essential for maintaining adequate blood flow. If the side branch is too small, it may be compromised during the main branch intervention, leading to ischaemia and reintervention. Conversely, a large side branch may correlate with a large proximal reference diameter in the main branch. During provisional and FKB techniques, meticulous attention to the side branch diameter is crucial. Proper sizing helps prevent dissections, reduces plaque shifting, and promotes successful stent deployment in both branches. Therefore, we conducted a subgroup analysis after PSM based on side branch dimensions, specifically considering diameters >2.5 mm and lesion lengths >20 mm. FKB reduced the LOCO and TVMI for side branches with diameters >2.5 mm, while a lower, albeit not significant, rate of the LOCO was observed for lesion lengths >20 mm treated with FKB. These results suggest that side branch features should be accurately assessed during PCI of coronary bifurcation, and our approach should be tailored accordingly. Of note, in our subgroup analysis of patients treated for ULM bifurcations, FKB was not associated with an incremental benefit. While the limited sample size of this subgroup should be considered in interpreting these findings, our results suggest that the relevance of the side branch (often left circumflex in the context of ULM bifurcations), rather than the site of the bifurcation itself, should be taken into account when deciding about FKB use in the context of provisional bifurcation stenting. The results of the currently ongoing CROSS-COBIS RCT (ClinicalTrials.gov: NCT05705362) are awaited and expected to provide insights into the impact of FKB on clinical outcome after treatment of non-left main coronary bifurcations.
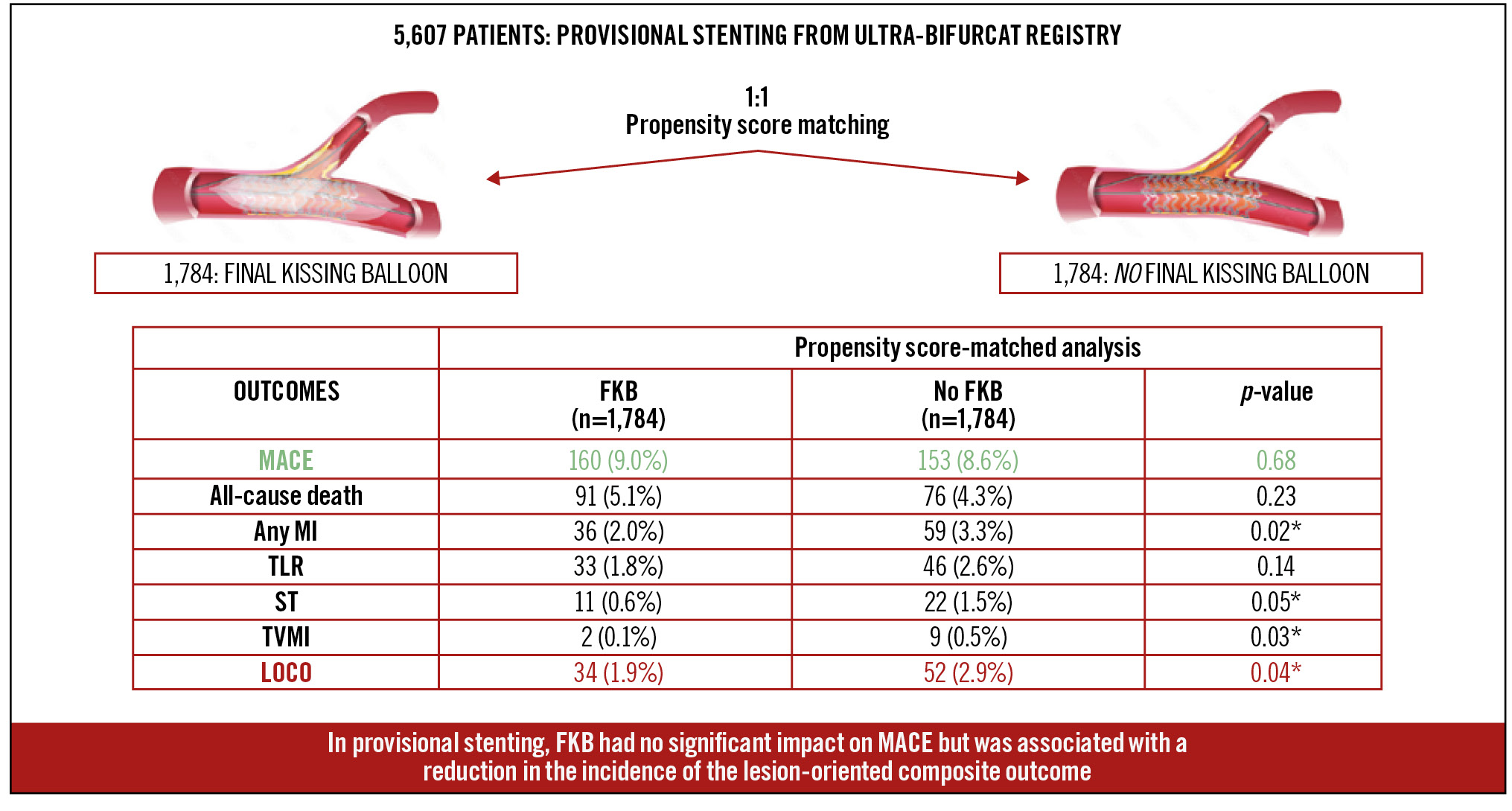
Central illustration. Final kissing balloon dilatation in patients with coronary bifurcation lesions treated with an upfront provisional stenting strategy. *Indicates statistical significance. FKB: final kissing balloon inflation; LOCO: lesion-oriented composite outcome; MACE: major adverse cardiac events; MI: myocardial infarction; ST: stent thrombosis; TLR: target lesion revascularisation; TVMI: target vessel myocardial infarction
Limitations
Several limitations should be acknowledged. While the sample size was large, the study design is retrospective with inherent limitations. This limitation may be partly balanced by the all-comer design with broad inclusion criteria and a 100% follow-up rate. Nevertheless, the study findings should be considered hypothesis-generating. A key limitation of our study is the use of endpoint definitions from the Academic Research Consortium-2 consensus document22, as the new definitions from the European Bifurcation Club were published after our registries were developed30. This temporal difference prevented the adoption of the latest terminologies and specific endpoints, such as the bifurcation-oriented composite endpoint. However, our endpoints related to the “index” lesion inherently include side branches. Additionally, while the new guidelines recommend separate trials for left main and non-left main bifurcations, our study addresses this by including a subgroup analysis for these bifurcations.
Despite the extensive adjustment with propensity score matching, which was overall effective (as shown in Supplementary Table 4), the retrospective nature of our study and the utilisation of multiple registries introduce potential biases and confounding. While PSM was employed to mitigate these biases, it cannot completely eliminate the impact of unknown or unmeasured variables. Therefore, our conclusions should be considered preliminary and interpreted with caution. In particular, we acknowledge that limited data were available with respect to the proximal optimisation technique (POT). Performing POT after FKB is recommended by European consensus for the treatment of coronary bifurcation lesions, although its impact on hard outcomes is uncertain4. In a previous manuscript19, we reported benefits of a short overlap between balloons. In the present analysis, which comprised a larger number of patients, we were not able to systematically obtain such data, yet we suppose that a short balloon overlap might even increase the clinical benefit of FKB that was observed in the present study. Finally, all evaluated endpoints are patient based, according to the design of the registries. While this approach enhances the clinical relevance of our findings, the absence of a lesion-level analysis may be regarded as a limitation.
Conclusions
Among the patients of this large, real-world registry, treated with a provisional stenting technique for coronary bifurcation lesions and assessed during medium-term follow-up, FKB was not associated with a significant reduction of MACE but was associated with a significant reduction of lesion-associated adverse outcomes, such as TLR and TVMI. Subgroup analyses of patients who were treated for true coronary bifurcation lesions and for lesions with major side branches revealed similar results. Our results should be interpreted with caution due to the limitations inherent in the observational and retrospective nature of the data derived from the merging of three different registries, highlighting the need for confirmation in a dedicated prospective study.
Impact on daily practice
Current interventional cardiology practice suggests provisional stenting as the preferred approach for most coronary bifurcation lesions, with a 2-stent strategy reserved for complex cases. Final kissing balloon inflation (FKB) is often employed to optimise stent apposition and minimise side branch compromise, especially in 2-stent techniques. The results of this multicentre retrospective study, pooling patient-level data from three large registries, offer real-world evidence on the effectiveness of FKB among patients treated with a provisional stenting technique. While FKB did not reduce major adverse cardiac events, it showed promise in reducing lesion-associated adverse outcomes, such as target lesion revascularisation and target vessel myocardial infarction.
Guest Editor
This paper was guest edited by Franz-Josef Neumann, MD, PhD; Department of Cardiology and Angiology, University Heart Center Freiburg - Bad Krozingen, Bad Krozingen, Germany.
Acknowledgements
Prof. J. Escaned is supported by the Intensification of Research Activity project INT22/00088 from the Spanish Instituto de Salud Carlos III.
Conflict of interest statement
C. von Birgelen indicated previous institutional research funds to the research department of Thoraxcentrum Twente from Abbott, Biotronik, Boston Scientific, and Medtronic. R. Piccolo reports personal fees from Biotronik, Amarin, Abiomed, Chiesi, and Medtronic, outside the submitted work. G. Patti indicated speaker/consultant fees from Abbott, AstraZeneca, Sanofi, Amgen, Menarini, Bayer, Pfizer, BMS, Daiichi Sankyo, PIAM, Malesci, Sigma-Tau, Chiesi, Medtronic, MSD, Boehringer Ingelheim, and Servier, outside the submitted work. J. Escaned indicated speaker/advisory member fees from Abbott, Abiomed, Boston Scientific, Medis, Philips, and Shockwave Medical, outside the submitted work. G. Campo reports grants from SMT, Siemens, and Medis, outside the submitted work. D. Capodanno reports personal fees from Abbott, Novo Nordisk, Sanofi, Terumo, and Chiesi; institutional fees from Medtronic; and participation on a data safety monitoring board or advisory board with MedAlliance, all outside the submitted work. C.-W. Nam reports institutional research grant from Abbott. The other authors have no conflicts of interest to declare. The Guest Editor reports consultancy fees from Novartis and Meril Life Sciences; speaker honoraria from Boston Scientific, Amgen, Daiichi Sankyo, and Meril Life Sciences; speaker honoraria paid to his institution from BMS/Pfizer, Daiichi Sankyo, Boston Scientific, Siemens, and Amgen; and research grants paid to his institution from Boston Scientific and Abbott.
Supplementary data
To read the full content of this article, please download the PDF.