Cory:
Unlock Your AI Assistant Now!
Ten years ago, the first studies on subclinical leaflet thrombosis (SLT) following transcatheter aortic valve implantation (TAVI) were reported. It was detected as hypoattenuated leaflet thickening (HALT) with or without reduced leaflet mobility (hypoattenuation affecting mobility [HAM]) on post-TAVI cardiac computed tomography (CT) scans1. A decade and multiple studies later, SLT remains a clinical conundrum due to its high incidence, dynamic clinical course, uncertain prognostic impact and challenging treatment strategies.
Certain subsets of patients, such as those undergoing valve-in-valve (ViV) TAVI procedures, are at an elevated risk for developing SLT, which may lead to thromboembolic events and premature structural valve deterioration (SVD)2. This concern is accentuated by the expansion of TAVI and ViV TAVI towards younger patients with longer life expectancies.
In this issue of EuroIntervention, Nagasaka et al present a timely study evaluating SLT in 117 patients who underwent ViV TAVI with a balloon-expandable valve (BEV)3. Four-dimensional CT, performed 1 month post-implantation, was used to detect SLT and to evaluate the BEV stent frame geometry and its relationship with the surrounding aortic root. Haemodynamic and clinical outcomes were available for up to 3 years post-procedure. HALT, detected in nearly 1 in 3 patients (31.6%), was associated with an increase in the composite outcome of all-cause mortality, stroke and heart failure hospitalisation (odds ratio [OR] 2.31; p=0.04) at 3-year follow-up. On multivariate analysis, the absence of oral anticoagulant therapy (OR 3.57; p=0.037) and BEV stent frame underexpansion (OR 2.46; p=0.18) were shown to be significant predictors for developing HALT. Importantly, no other clinical, anatomical or procedure-related factors were associated with the development of HALT.
Key limitations of this study include the relatively small sample size as well as the single timepoint used to evaluate HALT, which is known to have a dynamic temporal course. Additionally, evaluation of HALT was limited to the BEV leaflets, potentially underestimating the true prevalence of thrombosis in the aortic root complex, which may include supra-, sub- and perivalvular thrombosis. Finally, it should be noted that the conclusions from this study are only applicable to the use of BEV for ViV TAVI.
Nevertheless, restricting the study to a single transcatheter aortic valve (TAV) type represents a potential strength, as HALT outcomes can be influenced by the TAV design. This allows for a more granular and in-depth analysis of the impact of TAV design and geometry on HALT. The authors should be commended for undertaking a comprehensive evaluation of TAV stent frame expansion and eccentricity across seven different levels of the BEV stent frame.
Based on this analysis, the authors demonstrated that increased HALT was observed in the presence of TAV underexpansion, which is consistent with prior post-TAVI CT studies in native anatomies45. Computational modelling and bench studies have shown how TAV underexpansion can alter blood flow dynamics and cause turbulent flow within the aortic root. This, in turn, can lead to reduced washout in the aortic sinuses, consequently triggering platelet activation and thrombus formation6. TAV underexpansion can also lead to leaflet pinwheeling, which has been associated with an increased risk of HALT45, worse valve haemodynamics and, therefore, potentially increased leaflet stresses and premature SVD. In the recent ACURATE IDE randomised controlled trial, TAV underexpansion was associated with a 2-fold increased risk of all-cause mortality and a 3-fold increased risk of stroke7. Similarly, amongst bicuspid aortic stenosis patients treated with a BEV, TAV underexpansion and eccentricity were associated with increased rates of leaflet thrombosis and all-cause mortality in a study led by the same research group8. Furthermore, the investigators demonstrated the reduced prevalence of HALT after ViV TAVI amongst patients taking oral anticoagulant treatment, which is consistent with prior studies and existing evidence9.
In conclusion, these data highlight the importance of recognising and correcting TAV underexpansion, particularly in certain subsets of patients such as ViV TAVI, where there is an increased predisposition for developing SLT. Importantly, correcting valve underexpansion should be considered a key part of an overall holistic strategy focused on minimising the occurrence of SLT (Figure 1) and its potential clinical consequences for patients undergoing ViV TAVI.
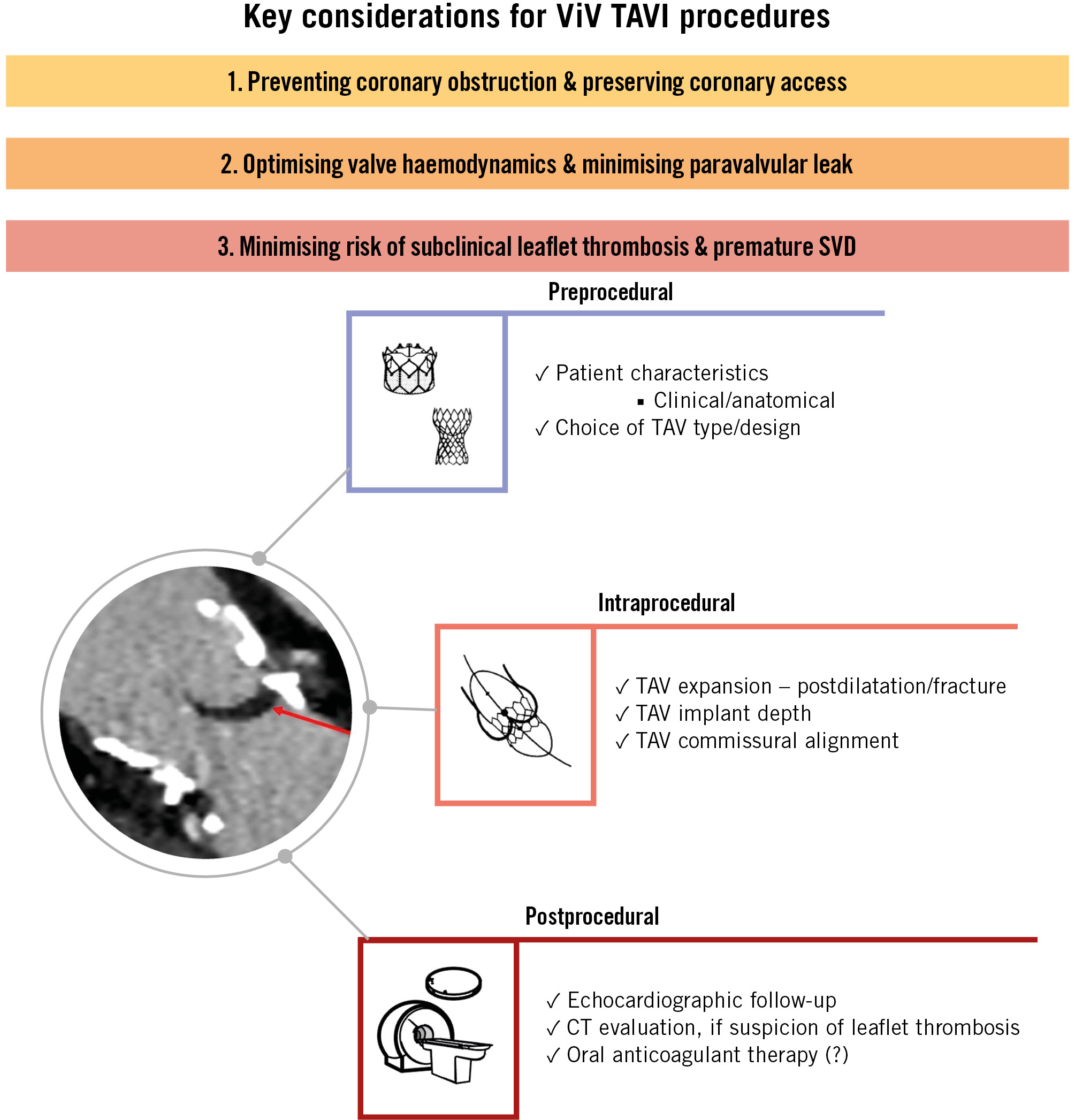
Figure 1. Key considerations for ViV TAVI procedures. The risk management of subclinical leaflet thrombosis following ViV TAVI is multifactorial. CT: computed tomography; SVD: structural valve deterioration; TAV: transcatheter aortic valve; TAVI: transcatheter aortic valve implantation; ViV: valve-in-valve
Conflict of interest statement
A. Khokhar received speaker fees from Abbott and Boston Scientific. O. De Backer received institutional research grants and consulting fees from Abbott, Boston Scientific, and Medtronic.