Cory:
Unlock Your AI Assistant Now!
Abstract
BACKGROUND: The hyperaemic stenosis resistance (HSR) index was introduced to provide a more comprehensive indicator of the haemodynamic severity of a coronary lesion. HSR combines both the pressure drop across a lesion and the flow through it. As such, HSR overcomes the limitations of the more traditional fractional flow reserve (FFR) or coronary flow reserve (CFR) indices.
AIMS: We aimed to identify the diagnostic and prognostic value of HSR and evaluate the clinical implications.
METHODS: Patients with chronic coronary syndromes (CCS) and obstructive coronary artery disease were selected from the multicentre ILIAS Registry. For this study, only patients with combined Doppler flow and pressure measurements were included.
RESULTS: A total of 853 patients with 1,107 vessels were included. HSR more accurately identified the presence of inducible ischaemia compared to FFR and CFR (area under the curve 0.71 vs 0.66 and 0.62, respectively; p<0.005 for both). An abnormal HSR measurement was an independent and important predictor of target vessel failure at 5-year follow-up (hazard ratio 3.80, 95% confidence interval: 2.12-6.73; p<0.005). In vessels deferred from revascularisation, HSR seems to identify more accurately those vessels that may benefit from revascularisation rather than FFR and/or CFR.
CONCLUSIONS: The present study affirms the theoretical advantages of the HSR index for the detection of ischaemia-Âinducing coronary lesions in a large CCS population. (Inclusive Invasive Physiological Assessment in Angina Syndromes Registry [ILIAS Registry], ClinicalTrials.gov: NCT04485234)
Physiology-guided revascularisation improves decision-making in patients with intermediate coronary lesions and is recommended by contemporary clinical guidelines1. Although several indices exist to assess the haemodynamic severity of a coronary lesion, the pressure-derived fractional flow reserve (FFR) has governed clinical research and practice2. An FFR-guided approach has proven its value over angiography alone, and lesions deemed haemodynamically significant by FFR seem to benefit from revascularisation in addition to optimal medical therapy (OMT)3.
Nevertheless, it is frequently overlooked that FFR is an estimate of the actual flow impairment of a stenosis. Most importantly, FFR is subject to the confounding impact of flow disturbances originating from the microcirculation and its reserve vasodilator capacity45. As such, FFR only partially describes the haemodynamic significance of a coronary lesion, and discordance with direct measurements of the vasodilator capacity, like the coronary flow reserve (CFR), is frequently present and prognostically important6.
The hyperaemic stenosis resistance (HSR) index − the ratio between the pressure drop across a coronary lesion and the throughflow during maximal hyperaemia − was introduced to provide a more comprehensive indicator of the haemodynamic severity of a coronary lesion7. The theoretical advantages of HSR over FFR were proven by the initial reports, showing a superior predictive power for assessment of the functional severity of a coronary lesion7. Data on the diagnostic and prognostic value of HSR, however, remain scarce.
The aim of this study was to evaluate the diagnostic and prognostic characteristics of HSR and to assess its clinical value in guiding revascularisation decision-making.
Methods
STUDY POPULATION
The study population was derived from the Inclusive Invasive Physiological Assessment in Angina Syndromes (ILIAS) Registry. The ILIAS Registry is a retrospective, global, multicentre initiative pooling lesion-level coronary pressure and flow data, as well as vessel-level clinical outcome data. All studies included were approved by local medical ethics committees. The registry is composed of 20 expert medical institutes from the Netherlands, Republic of Korea, Japan, Spain, Denmark, Italy and the USA. All data were gathered according to local study protocols between 1998 and 2018. Patients with a stable angina indication for invasive coronary angiography (ICA) and who had had a comprehensive invasive physiological assessment of at least one native coronary artery were enrolled in the registry. Patients with haemodynamic instability, significant valvular pathology and prior coronary artery bypass graft surgery, as well as patients with acute coronary syndromes, were excluded. For the current analysis, only patients with Doppler-derived measurements of coronary pressure and flow were included. Individual vessel-level data for pooled analysis were collected using standardised spreadsheets and a fully compliant cloud-based clinical data platform (Castor EDC; Castor). Standardised definitions were used for all variables.
The ILIAS Registry was registered at ClinicalTrials.gov: NCT04485234.
CORONARY ANGIOGRAPHY AND PHYSIOLOGICAL ASSESSMENT
Coronary angiography and intracoronary physiological assessments were performed in all institutions using standard techniques. After diagnostic coronary angiography, invasive physiological indices were measured using either separate pressure- (PressureWire; RADI Medical – now Abbott) and Doppler velocity sensor-equipped coronary guidewires (FloWire; EndoSonics – now Philips/Volcano) or a dual pressure- and Doppler flow velocity-equipped guidewire (ComboWire; Volcano – now Philips/Volcano). Intracoronary nitrate (100 or 200 μg) was administered before physiological measurements. Baseline (bAPV) and hyperaemic average peak flow velocities (hAPV) were labelled baseline and hyperaemic flow, respectively. Hyperaemia was induced by intravenous infusion of adenosine (140 μg/kg per min) or intracoronary bolus injection of adenosine (20-200 mcg)89.
The FFR was calculated as the ratio of mean distal to mean aortic pressure during hyperaemia. The CFR was calculated as the ratio of the hAPV to bAPV. The HSR was calculated by the pressure gradient across a stenosis (aortic pressure [Pa]−distal pressure [Pd]) divided by the hAPV.
TREATMENT AND CLINICAL FOLLOW-UP
Percutaneous coronary intervention (PCI) was performed according to clinical practice guidelines at the time of the procedure. However, final decisions regarding revascularisation were at the discretion of the operator. Clinical follow-up was obtained at outpatient clinic visits or by telephone contact to ascertain the occurrence of target vessel failure (TVF). TVF was defined as the composite of cardiac death, acute myocardial infarction not clearly attributable to a non-target vessel, and clinically driven revascularisation of the target vessel by means of coronary artery bypass graft surgery or PCI10. All patient-reported events were verified by evaluating hospital records or by contacting the treating cardiologist or general practitioner.
STATISTICAL ANALYSIS
Data were analysed on a per-patient basis for clinical characteristics and on a per-vessel basis for all other calculations. Normality and homogeneity of the variances were tested using the Shapiro-Wilk and Levene’s tests. Continuous variables are presented as mean±standard deviation (SD) or median (first, third quartile [Q1, Q3]) and were compared with the Student’s t-test or Mann-Whitney U test. Categorical variables are presented as counts and percentages and were compared using Fisher’s exact test. For vessel-to-patient analyses, robust regressions with Huber-White robust standard errors were used to adjust for clustering of vessels within patients, where appropriate. Receiver operating characteristic (ROC) curve analysis was performed to determine the diagnostic accuracy of HSR in comparison to the conventional physiological parameters. For this analysis, the presence of reversible perfusion abnormalities during non-invasive stress testing prior to coronary angiography was used as the standard of reference. The optimal cutoff value was determined using the Liu method11. The discriminative value of the dichotomous variables for the presence of inducible ischaemia was tested based on the McNemar statistics. The association of HSR and the conventional parameters as continuous and dichotomous variables with TVF at 5-year follow-up was evaluated using Cox proportional hazards models, adjusted for the effect of relevant clinical and angiographic characteristics (p<0.1 for inclusion). All clinical and angiographic characteristics were considered as covariates. Event rates over time are displayed using the Kaplan-Meier method. The statistical significance of differences in event rates between subgroups was assessed with unadjusted (marginal) Cox proportional hazards models and are presented using hazard ratios (HR) with 95% confidence intervals (CI). All Cox proportional hazards models were preceded by verification of the proportional hazard assumption using Schoenfeld’s residuals. A p-value<0.05 (2-sided) was considered statistically significant. The STATA version 14.0 (StataCorp) software package was used for calculations.
Results
The baseline and angiographic characteristics of all study patients are shown in Table 1. From the ILIAS Registry, 853 patients with 1,107 vessels were assessed using Doppler flow technique and considered eligible for the current analysis. After excluding patients without complete follow-up data or physiological data (N=43), a total of 810 patients with 1,050 vessels formed the final study population, of which 309 vessels (29%) underwent revascularisation during the index procedure. The mean age was 63±10 years, and 74% were male. The most evaluated vessel was the left anterior descending artery (LAD; N=414, 57%). The mean FFR was 0.85±0.08; the mean CFR was 2.5±0.7.
Table 1. Clinical and angiographic characteristics of the study population.
| Clinical characteristics | |
|---|---|
| Demographics | |
| Patients | 810 |
| Age, years | 63±10 |
| Male | 547 (74) |
| Coronary risk factors | |
| Smoking | 196 (27) |
| Hypertension | 419 (56) |
| Hyperlipidaemia | 538 (73) |
| Diabetes | 182 (24) |
| Family history of CAD | 330 (46) |
| Prior myocardial infarction | 191 (26) |
| Prior PCI | 201 (29) |
| Angiographic characteristics | |
| Vessels | 1,050 |
| Evaluated vessel | |
| LAD | 414 (57) |
| RCA | 143 (19) |
| RCx | 176 (24) |
| Quantitative coronary angiography | |
| Diameter stenosis, % | 55±15 |
| Lesion length, mm | 13.4±4.7 |
| Physiological indices | |
| FFR | 0.85±0.08 |
| CFR | 2.50±0.68 |
| Data are presented as N, N (%) or mean±standard deviation. CAD: coronary artery disease; CFR: coronary flow reserve; FFR: fractional flow reserve; LAD: left anterior descending artery; PCI: percutaneous coronary intervention; RCA: right coronary artery; RCx: ramus circumflex artery | |
DIAGNOSTIC PERFORMANCE OF THE HYPERAEMIC STENOSIS RESISTANCE INDEX
Within the final study population, 422 patients had non-invasive stress testing available prior to the index coronary angiography. Figure 1 shows the ROC curves for HSR, FFR and CFR in the same population. The corresponding area under the curve (AUC) and optimal cutoff values are shown in Table 2. The AUC for HSR was 0.71 (95% CI: 0.66-0.75), significantly higher compared with that of CFR and FFR (0.63 [95% CI: 0.58-0.68] and 0.66 [95% CI: 0.63-0.72], respectively; all p<0.005 vs HSR). The optimal cutoff value of HSR for inducible ischaemia was 0.80 mmHg/cm per second with a sensitivity of 57% and a specificity of 89%. In comparison, the optimal cutoff value for FFR in the same population was 0.83 (sensitivity 61%, specificity 68%) and for CFR was 2.23 (sensitivity 56%, specificity 66%). Supplementary Table 1 and Supplementary Table 2 depict the numbers of agreement and disagreement between the binary values of HSR and FFR, and HSR and CFR, with non-invasive tests. The McNemar statistics show that the HSR (cutoff value: 0.80 mmHg/cm per second) has a superior discriminative value for the presence of inducible ischaemia compared to both FFR (cutoff: 0.80; odds ratio [OR] 2.0, 95% CI: 1.4-3.0; p<0.005) and CFR (cutoff: 2.0; OR 1.8, 95% CI: 1.3-2.4; p<0.005).
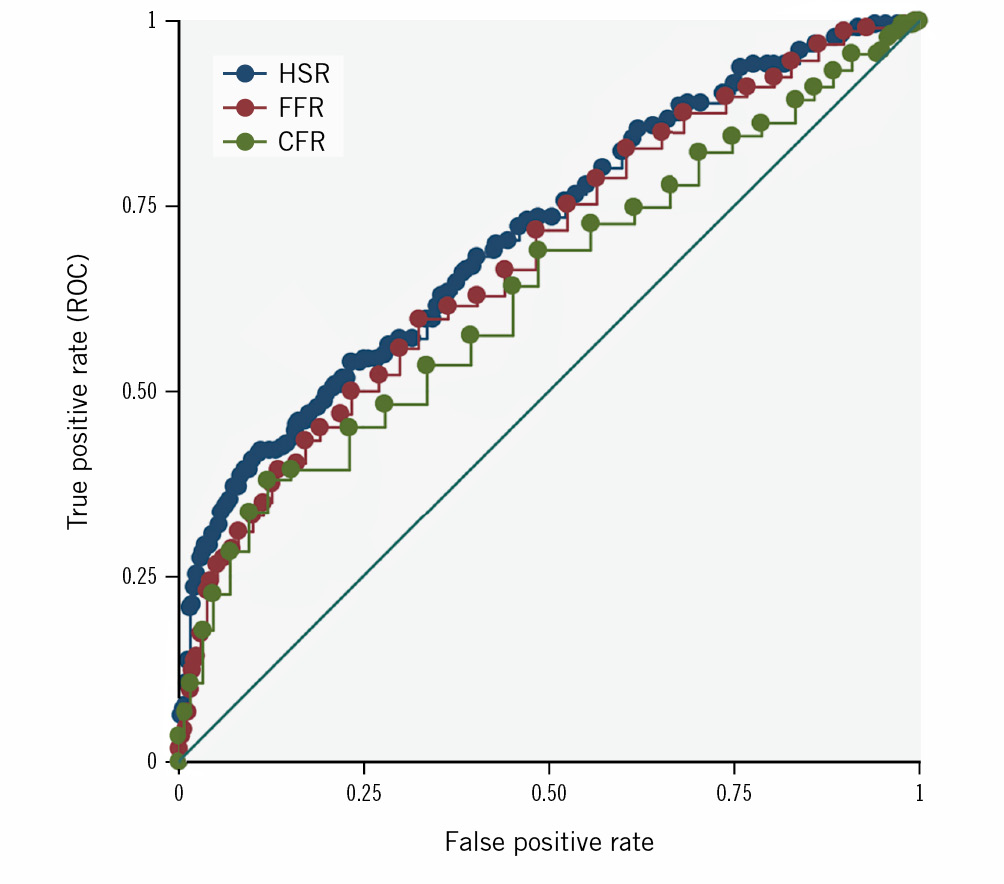
Figure 1. Receiver-operating characteristic (ROC) curves for HSR, FFR and CFR for the presence of inducible ischaemia on non-invasive modalities. CFR: coronary flow reserve; FFR: fractional flow reserve; HSR: hyperaemic stenosis resistance
Table 2. AUROC analysis and optimal cutoff value determination.
| AUC(95% CI) | Optimal cutoff | Sensitivity | Specificity | |
|---|---|---|---|---|
| HSR | 0.71 (0.66-0.75)* | 0.80 | 0.57 | 0.89 |
| FFR | 0.66 (0.62-0.71) | 0.83 | 0.61 | 0.68 |
| CFR | 0.63 (0.58-0.69) | 2.23 | 0.56 | 0.66 |
| *HSR has a significantly higher AUC versus FFR and CFR. AUC: area under the curve; AUROC: area under the receiver-operating characteristic curve; CFR: coronary flow reserve; CI: confidence interval; FFR: fractional flow reserve; HSR: hyperaemic stenosis resistance | ||||
CLINICAL OUTCOMES DETERMINED BY HSR AND COMPARED WITH FFR AND CFR
In those vessels deferred from revascularisation, a total of 73 vessels experienced at least one TVF at 5-year follow-up (10.0%) (Table 3). Among the clinical and angiographic characteristics, age, sex, diabetes, hypercholesterolaemia, family predisposition for cardiovascular disease, previous myocardial infarction, and a reduced left ventricular function were associated with TVF at 5-year follow-up and were considered as confounders for multivariable adjustment. After correction for these confounders, HSR as a continuous variable was independently and significantly associated with TVF at 5-year follow-up (HR 5.43, 95% CI: 3.25-9.08; p<0.005). Using the cutoff value of 0.80 mmHg/cm per second, an abnormal HSR measurement was associated with an increased risk of TVF at 5-year follow-up (HR 3.80, 95% CI: 2.12-6.73; p<0.005). Figure 2A-Figure 2C show the Kaplan-Meier curves for TVF at 5-year follow-up according to normal and abnormal HSR measurements and for FFR and CFR in the same population. Similar to HSR, both an abnormal FFR (<0.80) and an abnormal CFR (<2.0) were independent predictors of TVF at 5-year follow-up (HR 2.24, 95% CI: 1.38-3.64; p<0.005 and HR 3.10, 95% CI: 1.91-5.03; p<0.005, respectively). In addition, both FFR (HR 0.02, 95% CI: 0.01-0.11; p<0.0001) and CFR (HR 0.67, 95% CI: 0.55-0.83; p<0.001) as continuous variables were independently and significantly associated with TVF in this population.
Table 3. TVF and components at 5-year follow-up across the study population
| Vessels (N=1,050) | Total N (%) |
|---|---|
| Target vessel failure | 73 (10) |
| Cardiac death | 27 (3.6) |
| Acute myocardial infarction(target vessel) | 13 (1.8) |
| Urgent revascularisation | 52 (7.0) |
| TVF: target vessel failure | |
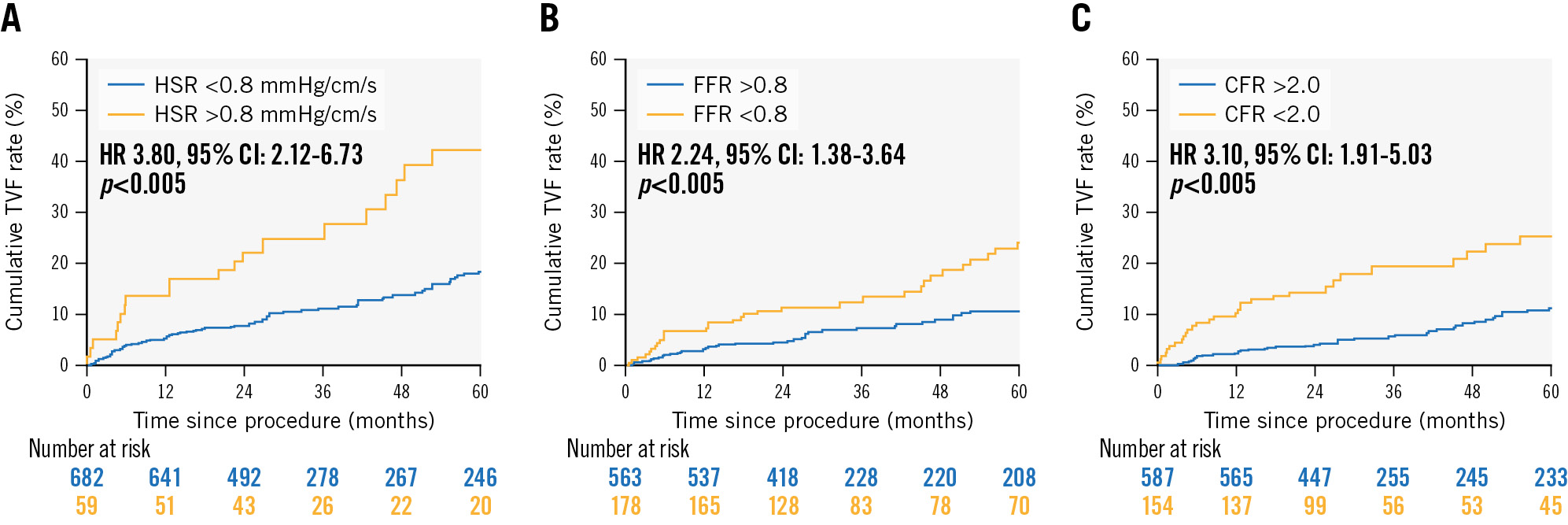
Figure 2. Kaplan-Meier curves for the cumulative incidence of target vessel failure (TVF) at 5-year follow-up. The curves show the TVF rate stratified by HSR (A), FFR (B) and CFR (C). CFR: coronary flow reserve; CI: confidence interval; FFR: fractional flow reserve; HR: hazard ratio; HSR: hyperaemic stenosis resistance
PROGNOSTIC VALUE OF HSR FOR RISK STRATIFICATION COMPARED TO FFR AND CFR IN VESSELS DEFERRED FROM REVASCULARISATION
The clinical value of HSR compared to FFR and CFR was analysed based on the discordance between these indices and the association with clinical outcomes in patients deferred from revascularisation. In vessels deferred from revascularisation during the index procedure, discordance between HSR and FFR was present in 18% of the vessels (N=133 out of 741). Of these, almost all had abnormal FFR in the presence of a normal HSR (N=126). Figure 3A depicts the Kaplan-Meier curves for these vessels and the cumulative incidence of TVF. Vessels with an abnormal HSR had the highest risk of TVF at 5-year follow-up, despite the presence of normal (HR 6.3, 95% CI: 1.8-21.1; p=0.003) or abnormal FFR values (HR 4.0, 95% CI: 2.1-7.7; p<0.001). Those vessels with normal HSR values in the presence of abnormal FFR values showed similar clinical outcomes to those vessels with concordant normal values. Figure 3B shows the Kaplan-Meier curves for vessels with either concordant or discordant CFR and HSR values. Discordance between CFR and HSR in vessels deferred from revascularisation was present in 22% of the vessels (N=169 out of 741). Both vessels with discordant values had an increased risk compared to those vessels with a concordant normal value, either with an abnormal CFR and normal HSR (HR 2.8, 95% CI: 1.6-4.9; p<0.001) or with an abnormal HSR and normal CFR (HR 3.4, 95% CI: 1.5-7.8; p=0.004). There was no statistical difference between these risks (p for difference: 0.680). Vessels with abnormal HSR and CFR had the highest risk for TVF (HR 8.2, 95% CI: 3.8-17.7; p<0.001).
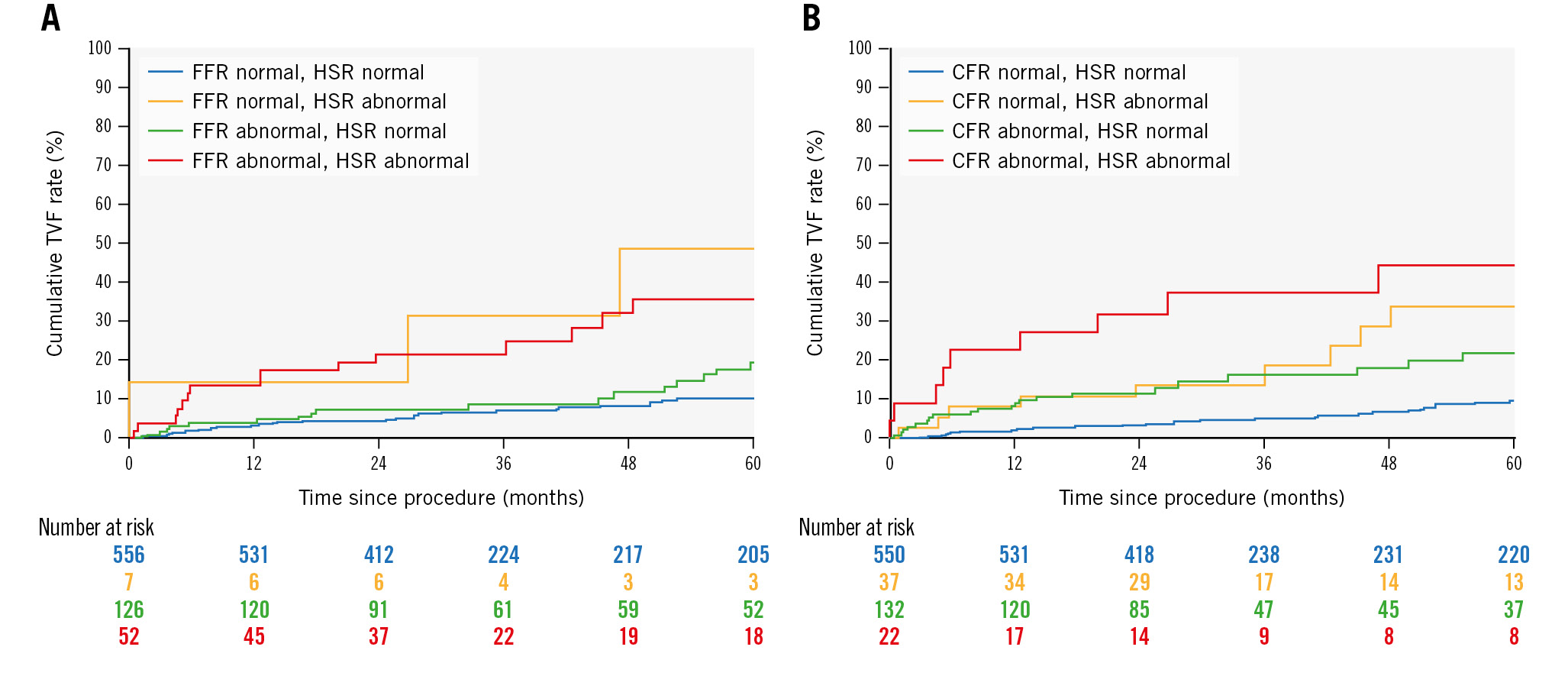
Figure 3. Kaplan-Meier curves for the cumulative incidence of target vessel failure (TVF) at 5-year follow-up. The curves show the TVF rate stratified by the concordance between FFR and HSR (A), and CFR and HSR (B). CFR: coronary flow reserve; FFR: fractional flow reserve; HSR: hyperaemic stenosis resistance
Discussion
The current study evaluates the diagnostic and prognostic characteristics of HSR, a physiological index for the evaluation of the haemodynamic severity of a coronary lesion based on the ratio of the pressure gradient and flow velocity during maximal hyperaemia. The main findings are (1) HSR had a significantly higher predictive power to detect ischaemia based on non-invasive stress testing compared to the conventional physiological parameters FFR and CFR; (2) HSR was a strong and independent predictor of an increased risk for TVF at 5-year follow-up; (3) HSR seems to have additional clinical value compared to the conventional indices for risk stratification in vessels deferred from revascularisation (Central illustration).
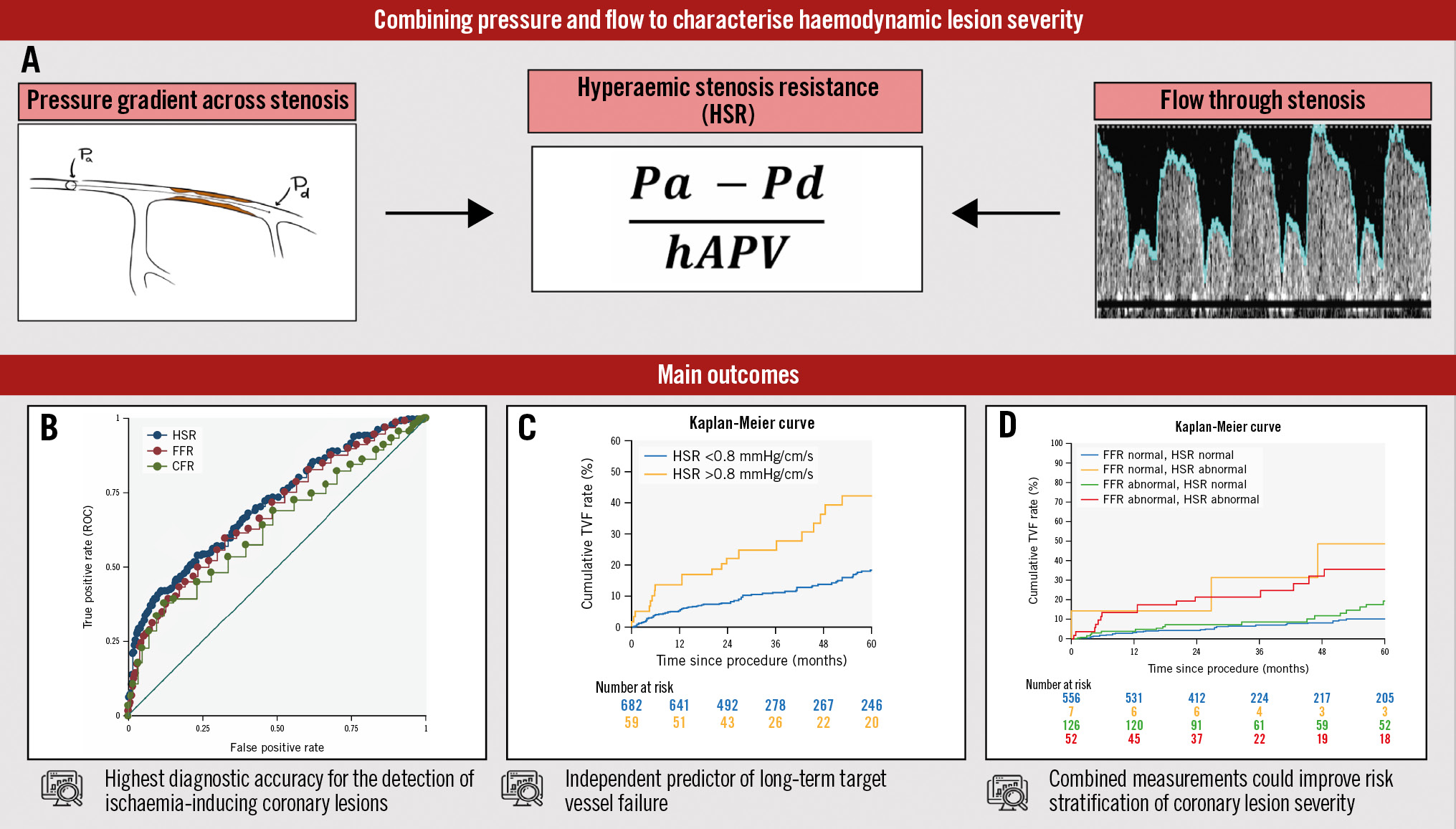
Central illustration. Clinical value of hyperaemic stenosis resistance in stable angina. A general overview of the results of this study. A) Hyperaemic stenosis resistance (HSR) is derived from the ratio between the pressure drop across a stenosis and the flow through it. B) The HSR has a significant higher predictive power to detect ischaemia, is a strong and independent predictor of TVF (C) , and seems to have additional clinical value for risk stratification in vessels deferred from revascularisation (D). CFR: coronary flow reserve; FFR: fractional flow reserve; hAPV: hyperaemic average peak flow velocity; Pa: aortic pressure; Pd: distal pressure; ROC: receiver-operating characteristic; TVF: target vessel failure
PHYSIOLOGICAL ASSESSMENT OF THE HAEMODYNAMIC SEVERITY OF A CORONARY LESION
Physiology-guided assessment of the haemodynamic severity of intermediate coronary lesions is recommended in contemporary clinical guidelines1. Nevertheless, conventional indices like FFR and CFR are subject to intrinsic limitations that may impair their diagnostic efficacy. FFR describes the flow impairment of a coronary lesion by estimating the fraction of maximal flow that can still be achieved in the presence of a stenosis relative to flow through the same artery without a stenosis2. The limitations of the FFR theorem for stenosis assessment have been extensively described elsewhere12. The most important consideration is that coronary flow drives the pressure drop across a stenosis. In the presence of a diseased microcirculation, maximal hyperaemic flow is reduced and the pressure drop across a stenosis is attenuated. Consequently, FFR may be deemed normal in the presence of clinically relevant flow impairment across the coronary circulation. It is shown that simultaneous assessment of CFR adequately identifies those cases and has important prognostic value, but it lacks the ability to distinguish between flow impairment originating from an epicardial stenosis or the microcirculation6. As such, it does not specifically identify those vessels in which alleviation of the stenosis by revascularisation would sufficiently improve coronary blood flow13.
HSR, assessing the pressure drop across a coronary lesion in relation to the flow through it, overcomes these limitations by normalising the pressure drop across the stenosis by the flow that goes through it, and thereby provides a lesion-specific parameter of functional significance7. The diagnostic value of HSR is reinforced by the findings of this study. In line with previous reports, we found that HSR has the highest diagnostic value for the presence of ischaemia on non-invasive stress testing (AUC 0.72 vs 0.66 for FFR [p<0.005] and 0.62 for CFR [p<0.005])7. In addition, we found that the optimal cutoff value for ischaemia (0.80 mmHg/cm/sec) was similar to that of these previous reports and reported the highest discriminative value of inducible ischaemia.
THE PROGNOSTIC VALUE OF HSR ALONE AND COMPARED WITH FFR AND CFR
Despite the theoretical and diagnostic advantages of HSR, there has been limited attention for a more comprehensive assessment of functional severity of a coronary stenosis. Several clinical trials have confirmed the advantages of pressure-derived indices over angiography-guided treatment, and consequently, these indices have governed the clinical and scientific field. Nonetheless, these trials also show that up to one-half of the vessels with abnormal pressure ratios could safely be deferred from revascularisation3. In addition, recent publications reported no prognostic benefit of an FFR-guided approach in several cases, and the debate regarding its value has gained fresh prominence14151617. As mentioned before, discordance between pressure and flow could explain this phenomenon and has significant clinical implications6. However, neither FFR nor CFR specifically address pressure and flow across a haemodynamic lesion, and the additional value of combining these indices to guide revascularisation is debated. In contrast, HSR does specifically address the haemodynamic characteristics across a stenosis, and our study is the first to describe the prognostic value of HSR in a large population of patients with chronic coronary syndromes (CCS). We document that HSR as a continuous variable was independently and significantly associated with TVF at 5-year follow-up (HR 1.40, 95% CI: 1.06-1.84; p=0.016). Based on the optimal clinical cutoff value of 0.80, which is the same as the threshold obtained in previous smaller clinical studies, an abnormal HSR value showed an increased risk for TVF at 5-year follow-up (HR 2.48, 95% CI: 1.49-4.13; p<0.005).
In addition, we evaluated the clinical value of HSR compared to the conventional indices in vessels deferred from revascularisation. In comparison with FFR, HSR was discordant in 17% of these vessels, and almost all of these had normal HSR values in the presence of abnormal FFR values. In these vessels, the risk of TVF during a 5-year follow-up period was not significantly higher compared to those vessels with concordant normal values (HR 1.7, 95% CI: 0.9-3.2; p=0.063). It seems that deferral from revascularisation is safe in these vessels, as hyperaemic flow is adequate. Nevertheless, it should be noted that reports regarding the optimal treatment of these “non-flow-limiting” lesions is still debated, and future research is warranted. Additionally, although clinically less prominent, those vessels with abnormal HSR values in the presence of normal FFR values had the highest risk of TVF (HR 6.3, 95% CI: 1.8-21.1; p=0.003). These vessels are characterised by a diminished hyperaemic flow, by which the pressure drop is attenuated and the HSR is increased. Compared to CFR, HSR was discordant in 22% of the vessels. Patients with normal HSR values and abnormal CFR values had a similar increased risk for TVF (HR 2.8, 95% CI: 1.6-4.9; p<0.001) as those with abnormal HSR and normal CFR (HR 3.4, 95% CI: 1.5-7.8; p=0.004), compared to those with concordant normal values. This is in accordance with the increased risk of patients with angina with no obstructive coronary artery disease and coronary microvascular dysfunction1819.
Limitations
Some limitations of our study merit consideration. First, the decision about revascularisation for the stenosis of interest was driven by clinical practice guidelines at the time of the index procedure but was ultimately at the discretion of the operator. In this respect, it is important to note that, despite the correction for confounders, the occurrence of the TVF endpoint is subject to the bias of the unblinded design of the registry. Second, our study population consisted of patients with stable coronary artery disease. Hence, our findings cannot be directly extrapolated to the setting of non-culprit vessels in acute coronary syndromes. Third, there was no detailed information on the medication profiles of enrolled patients during the follow-up period nor regarding angina burden. Finally, despite the large number of included vessels and the length of follow-up, this study suffers from the basic limitations of a retrospective registry, and these conclusions should therefore be confirmed in a randomised study.
Conclusions
The present study affirms the diagnostic accuracy of HSR for the detection of ischaemia-inducing coronary lesions in a large CCS population. Moreover, this study is the first to show that HSR has an important prognostic value based on the long-term risk for TVF. As such, this study adds to the evolving literature that a comprehensive approach of combined flow and pressure measurements could improve the risk stratification of coronary lesions during an invasive coronary angiography. These findings corroborate the potential of combined pressure and flow measurements in the catheterisation laboratory and warrant future prospective studies.
Impact on daily practice
Physiology-guided treatment of intermediate coronary lesions has significantly improved clinical outcomes. Despite the recognised effectiveness of conventional physiological indices like fractional flow reserve and coronary flow reserve, each method possesses inherent limitations. Our study shows that the combined assessment of pressure and flow, by means of the hyperaemic stenosis resistance index, improves the diagnostic accuracy of the detection of ischaemia-inducing lesions. Moreover, our findings suggest that the incorporation of combined pressure and flow measurements could improve the risk stratification of coronary lesions during an invasive coronary angiography.
Conflict of interest statement
T.P. van de Hoef has received speaker fees and institutional research grants from Abbott and Philips. J.M. Lee has received research grants from Abbott and Philips. M. Echavarría-Pinto has received speaker fees from Abbott and Philips. C-W. Nam has received institutional research grants from Abbott. B-K. Koo has received institutional research grants from Abbott and Philips/Volcano. J.J. Piek has received support as a consultant for Philips/Volcano; and has received institutional research grants from Philips. The other authors have no conflicts of interest to declare related to this work.
Supplementary data
To read the full content of this article, please download the PDF.