Cory:
Unlock Your AI Assistant Now!
Abstract
BACKGROUND: ST-segment elevation myocardial infarction (STEMI) complicated by cardiogenic shock (STEMI-CS) is associated with high mortality rates. Patients admitted during off-hours, specifically on weekends and at night, show higher mortality rates, which is called the “off-hours effect”. The off-hours effect in patients with STEMI-CS treated with mechanical circulatory support, especially Impella, has not been fully evaluated.
AIMS: We aimed to investigate whether off-hours admissions were associated with higher mortality rates in this population.
METHODS: We used large-scale Japanese registry data for consecutive patients treated with Impella between February 2020 and December 2021 and compared on- and off-hours admissions. On- and off-hours were defined as the time between 8:00 and 19:59 on weekdays and the remaining time, respectively. The Cox proportional hazards model was used to calculate the adjusted hazard ratios (aHRs) for 30-day mortality.
RESULTS: Of the 1,207 STEMI patients, 566 (46.9%) patients (mean age: 69 years; 107 females) with STEMI-CS treated with Impella were included. Of these, 300 (53.0%) were admitted during on-hours. During the follow-up period (median 22 days [interquartile range 13-38 days]), 112 (42.1%) and 91 (30.3%) deaths were observed among patients admitted during off- and on-hours, respectively. Off-hours admissions were independently associated with a higher risk of 30-day mortality than on-hours admissions (aHR 1.60, 95% confidence interval: 1.07-2.39; p=0.02).
CONCLUSIONS: Our findings indicated the persistence of the “off-hours effect” in STEMI-CS patients treated with Impella. Healthcare professionals should continue to address the disparities in cardiovascular care by improving the timely provision of evidence-based treatments and enhancing off-hours medical services.
Cardiogenic shock (CS) is associated with high mortality and rehospitalisation rates1, and identifying the modifiable factors that influence these outcomes is of paramount importance. One such factor is the “off-hours effect", which refers to the phenomenon wherein patients admitted during off-hours show greater deterioration than those admitted during on-hours. The “off-hours effect” has been recognised in various clinical settings related to cardiovascular diseases. Temporal constraints can affect the prognosis in clinical scenarios such as acute myocardial infarction (AMI), acute pulmonary thromboembolism, and acute heart failure234. Patients admitted during off-hours, such as nights, weekends, or holidays, tend to have higher mortality rates than those admitted during regular weekday hours56. Factors contributing to the worsening outcomes of patients admitted during off-hours may include limited medical resources, reduced accessibility to healthcare facilities, and restricted availability of specialists to perform revascularisation procedures78.
Impella (Abiomed), a percutaneous ventricular assist device for circulatory support, was introduced as a treatment for patients with drug-resistant CS9. Utilisation of Impella requires a swift collaborative approach from a multidisciplinary team that includes specialists in cardiac intervention, cardiac surgery, and cardiovascular intensive care10. Consequently, the “off-hours effect” may still be observed in patients treated with Impella. However, to the best of our knowledge, no previous studies have explored this issue. Understanding the impact of the “off-hours effect” in patients receiving Impella during weekends or at night is vital for making evidence-informed treatment decisions. Thus, the aim of this study was to ascertain the existence of the “off-hours effect” in patients with ST-segment elevation myocardial infarction (STEMI) complicated by CS (STEMI-CS) who received mechanical circulatory support with an Impella device.
Methods
STUDY DESIGN
The Japan Registry for Percutaneous Ventricular Assist Device (J-PVAD) is an ongoing multicentre observational registry that enrols consecutive patients treated with Impella in Japan. All patients who underwent attempted or successful placement of the Impella device (Impella 2.5 or Impella CP) at qualified centres certified by the academic-based Japan Impella Committee were enrolled in the J-PVAD11. All patient data were collected by the participating investigators, registered directly in a centralised electronic database, and followed up during hospitalisation. The current study complied with the Declaration of Helsinki and was approved by the central institutional review board at Osaka University (“Catheter-type ventricular assist device registry study”; Graduate School of Medicine/Faculty of Medicine, Osaka University Ethics Committee, Approval no. 17232).
STUDY POPULATION AND DEVICE CHARACTERISTICS
We included consecutive patients who received Impella and underwent primary percutaneous coronary intervention (PCI) among patients with STEMI-CS requiring Impella (Impella CP or Impella 2.5) between February 2020 and December 2021. The inclusion criterion for this study was the presence of STEMI-CS, while the exclusion criteria were the provision of intra-aortic balloon pump support before Impella, treatment with Impella 5.0, no primary PCI within 6 hours of admission, and missing data on the door-to-unload (DTU) and door-to-balloon (DTB) times. CS was defined as a shock caused by AMI that met at least 1 of the following major criteria and 1 or more of the minor criteria: the major criteria were (1) systolic blood pressure <100 mmHg with a heart rate <60 beats per minute or >100 beats per minute, and (2) a drop of ≥30 mmHg in the usual systolic blood pressure, while the minor criteria included cold sweat, pale skin, cyanosis, a nailbed capillary refill time delay of >2 seconds, altered consciousness (Japan Coma Scale: 2 or higher), and conditions where the initial treating physician identified circulatory failure1112. The diagnostic criteria for STEMI were based on the universal definition13.
Impella 2.5 and Impella CP use 12 Fr- and 14 Fr-sized microaxial pumps, respectively. A 9 Fr catheter shaft was percutaneously inserted and placed in the left ventricle. This allowed for a continuous blood flow of up to 2.5 L/min for Impella 2.5 and 3.7 L/min for Impella CP, providing temporary circulatory support. Impella 2.5 was approved by the Pharmaceuticals and Medical Devices Agency of Japan’s Ministry of Health, Labour and Welfare in September 2016, while Impella CP received approval in March 2019 and has been in use since July 2019. In Japan, the use of Impella is reimbursed only for CS, primarily indicating its use for haemodynamic support in cases of acute heart failure that are resistant to pharmacotherapy11.
DEFINITION OF ADMISSION TIME AND BASELINE VARIABLES
“On-hours admission” was defined as admission from 8:00 a.m. to 7:59 p.m. from Monday to Friday, while “off-hours admission” was defined as admission during night shifts (from 8:00 p.m. to 7:59 a.m.), weekends, and holidays. The definition of off-hours was based on previous studies214. The holidays in Japan are determined by the law concerning public holidays and include the de facto end-of-year and New Year periods (29 December-31 December and 1 January-3 January). We defined the time from admission to the start of Impella support as the DTU time and the time from admission to reperfusion of the coronary artery as the DTB time.
ENDPOINT AND VARIABLE DEFINITIONS
The primary endpoint was 30-day all-cause mortality. Secondary endpoints were the incidence of complications including bleeding, haemolysis, peripheral ischaemia, access-related vascular injury, and cerebrovascular accidents. In the registry protocol, haemolysis was defined by an increase of >40 mg/dL in the plasma-free haemoglobin level within 48 hours after Impella insertion or a clinically significant increase in lactic acid dehydrogenase and indirect bilirubin levels along with a decrease in the haemoglobin level within 48 hours of Impella insertion. Haemorrhage was defined as an event requiring surgical intervention or transfusion. A clinically relevant haematoma was defined as a haematoma with a diameter ≥5 cm or a haematoma that required surgical intervention. Peripheral ischaemia was defined as a reduction in the perfusion of peripheral tissues requiring medical or surgical treatment. An access-related vascular injury was defined as one requiring diagnostic testing followed, if necessary, by therapeutic intervention, such as a pseudoaneurysm; arteriovenous fistula; vascular thrombosis; vascular dissection, penetration, or rupture; and vascular stenosis. Stroke was defined as a clinically significant neurological deficit, an evident infarction, and/or an intracranial haemorrhage. Other relevant datasets included baseline patient characteristics, limited laboratory values, device usage status, and procedural characteristics11.
STATISTICAL ANALYSIS
Baseline characteristics were compared between patients with on- and off-hours admissions. Continuous variables are presented as mean±standard deviation (SD), and these variables were compared using the Student’s t-test. Categorical variables are presented as rates or proportions and were analysed using either the chi-square or Fisher’s exact test. The cumulative survival probability was calculated over time from the day of admission between on- and off-hours admissions using Kaplan-Meier curves and compared using log-rank tests. The frequency of complications and crude in-hospital outcomes was investigated by stratifying patients into those who received extracorporeal membrane oxygenation (ECMO) combined with Impella and those who only received Impella. Cox proportional hazard models were used to estimate multivariable-adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs) for all-cause mortality. Covariates in the first adjusted model (model 1) included age, sex, and admission time, while the covariates in the additionally adjusted model (model 2) included age, sex, body mass index (BMI), smoking, hypertension, hyperlipidaemia, diabetes, chronic kidney disease, previous myocardial infarction, angina pectoris, congestive heart failure, out-of-hospital cardiac arrest, in-hospital cardiac arrest, and admission time. Additionally, we further included the DTU and DTB times and ECMO implantation in the fully adjusted model (model 3), and we employed a multiplicative interaction term for admission time and ECMO implantation to evaluate the modification of effect measurement due to ECMO implantation in model 3. To account for the difference in experience among facilities and its impact on prognosis, we classified the hospital intervention volume based on the number of cases into tertiles, dividing them into top and middle, and model 4 was further adjusted for the hospital intervention volume. We performed a complete case analysis using Cox hazard analysis for each model, examined the proportionality assumption using Schoenfeld residuals, and found no models in which the assumption was violated. We performed a similar analysis of the cases limited to weekday admissions. We also conducted logistic regression analysis to evaluate the relationship between the primary outcomes and specific admission periods. Admissions were categorised into 6 time periods, each spanning 4 hours, starting at 8:00 a.m. (8:00 a.m. to 11:59 a.m., 12:00 p.m. to 3:59 p.m., 4:00 p.m. to 7:59 p.m., 8:00 p.m. to 11:59 p.m., 12:00 a.m. to 3:59 a.m., and 4:00 a.m. to 7:59 a.m.). All our hypotheses were 2-sided. Statistical significance was set at p<0.05. All statistical analyses were conducted using R, version 4.2.3 (R Foundation for Statistical Computing).
Results
Of the 1,207 patients with STEMI, 566 (46.9%) were analysed after application of the additional exclusion criteria, and of these patients, 300 (53.0%) were admitted during on-hours. Figure 1 illustrates the patient selection process for this cohort. Table 1 summarises the baseline characteristics of the patients admitted during off- and on-hours; the baseline variables were comparable between on- and off-hours admissions. The mean age was 69.0±11.9 years, with 18.9% (n=107) females, and the mean BMI was 23.5±4.5 kg/m2. Of the entire cohort, 20.7% (n=117) of the patients presented with out-of-hospital cardiac arrest, and 29% (n=164) experienced in-hospital cardiac arrest after admission. The majority (51.6%, n=292) had Interagency Registry for Mechanically Assisted Circulatory Support (INTERMACS) profile 1. Regarding the introduced Impella device, 95.1% (n=538) received Impella CP, while the remaining patients received Impella 2.5. ECMO was used in 32.9% (n=186) of the patients. Among the entire cohort, 232 (41.0%) received cardiopulmonary resuscitation (CPR), while 334 (59.0%) did not. Regarding the haemodynamic status of trial participants, stratified by the implementation of CPR, patients who received CPR had lower systolic blood pressure before Impella insertion (79.6 mmHg vs 94.0 mmHg; p<0.001) and higher lactate levels (10.3 mmol/L vs 5.2 mmol/L; p<0.001).
The DTB time was longer for patients admitted during off-hours compared to those admitted during on-hours (median 103 minutes vs 88 minutes; p=0.006). Similarly, the DTU time was also longer for patients admitted during off-hours than for those during on-hours (median 90 minutes vs 77 minutes; p=0.02) (Figure 2).
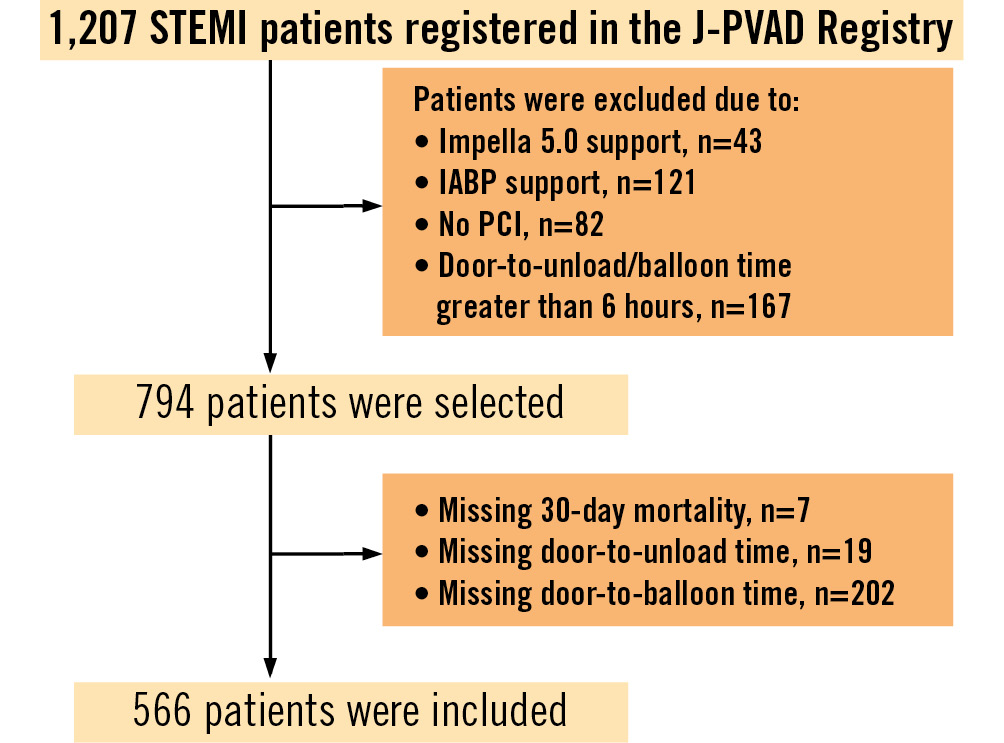
Figure 1. Flowchart of the patient selection process for this study. Of the 1,207 patients with STEMI, 566 (46.9%) were analysed after the application of the additional exclusion criteria. IABP: intra-aortic balloon pump; J-PVAD: Japan Registry for Percutaneous Ventricular Assist Device; PCI: percutaneous coronary intervention; STEMI: ST-segment elevation myocardial infarction
Table 1. Baseline characteristics of study participants.
| On-hours admissionn=300 (53.0%) | Off-hours admissionn=266 (47.0%) | p-value | |
|---|---|---|---|
| Characteristics | |||
| Age, years | 68.4±12.1 | 69.7±11.7 | 0.18 |
| Female sex | 53 (17.7) | 54 (20.3) | 0.49 |
| Previous medical history | |||
| Hypertension | 185 (61.7) | 181 (68.0) | 0.27 |
| Hyperlipidaemia | 160 (53.3) | 126 (47.4) | 0.33 |
| Diabetes | 114 (38.0) | 117 (44.0) | 0.35 |
| Chronic kidney disease | 75 (25.0) | 70 (26.3) | 0.70 |
| Myocardial infarction | 45 (15.0) | 34 (12.8) | 0.73 |
| Heart failure | 30 (10.0) | 25 (9.4) | 0.97 |
| Cerebrovascular event | 20 (6.7) | 19 (7.1) | 0.77 |
| Body mass index, kg/m2 | 23.4±4.30 | 23.7±4.63 | 0.43 |
| Smoking history | 0.90 | ||
| Current smoker | 94 (31.3) | 89 (33.5) | |
| Former smoker | 77 (25.7) | 62 (23.3) | |
| Out-of-hospital cardiac arrest | 66 (22.0) | 51 (19.2) | 0.71 |
| In-hospital cardiac arrest | 85 (28.3) | 79 (29.7) | 0.79 |
| Cardiopulmonary resuscitation | 123 (41.0) | 109 (41.0) | 1.00 |
| Functional Class | 0.27 | ||
| NYHA 1 | 8 (2.7) | 6 (2.3) | |
| NYHA 2 | 4 (1.3) | 4 (1.5) | |
| NYHA 3 | 22 (7.3) | 10 (3.8) | |
| NYHA 4 | 234 (78.0) | 225 (84.6) | |
| INTERMACS profile | 0.59 | ||
| 1 | 160 (53.3) | 132 (49.6) | |
| 2 | 35 (11.7) | 39 (14.7) | |
| ≥3 | 10 (3.3) | 10 (3.8) | |
| Systolic blood pressure before Impella, mmHg | 90.6±34.8 | 85.3±36.3 | 0.08 |
| Diastolic blood pressure before Impella, mmHg | 60.6±24.3 | 56.91±26.0 | 0.08 |
| Lactate level before Impella, mmol/L | 7.81±10.8 | 7.11±4.8 | 0.40 |
| Left ventricular ejection fraction, % | 28.7±9.9 | 31.5±12.7 | 0.06 |
| Impella device CP | 285 (95.0) | 253 (95.1) | 1.00 |
| Access site of Impella | |||
| Femoral | 300 (100) | 266 (100) | 1.00 |
| Impella implantation before PCI | 240 (80.0) | 221 (83.1) | 0.41 |
| ECMO implantation | 0.61 | ||
| ECMO before Impella | 55 (18.3) | 55 (20.7) | |
| ECMO after Impella | 38 (12.7) | 38 (14.3) | |
| Data are given as mean±SD or n (%). ECMO: extracorporeal membrane oxygenation; INTERMACS: Interagency Registry for Mechanically Assisted Circulatory Support; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; SD: standard deviation | |||
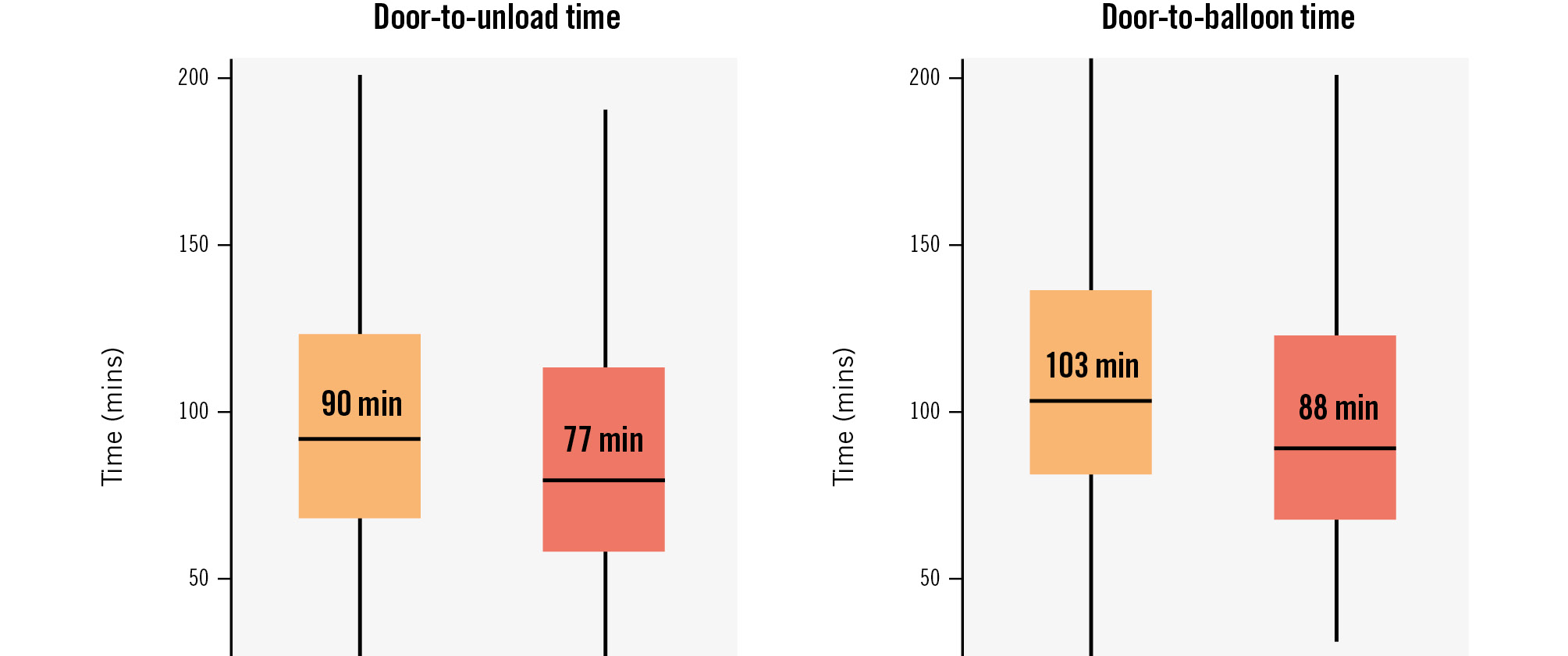
Figure 2. Comparison of off-hours admissions and on-hours admissions for door-to-balloon and door-to-unload times. Both DTB and DTU times were longer for patients admitted during off-hours compared to those admitted during on-hours. DTB: door-to-balloon; DTU: door-to-balloon
ASSOCIATION BETWEEN ADMISSION TIME AND CLINICAL ADVERSE EVENTS DURING HOSPITALISATION
The median follow-up time was 22.0 days (interquartile range [IQR] 13-38 days): 21.0 days (IQR 11-36 days) among patients admitted during off-hours and 23.0 days (IQR 14-38 days) among those admitted during on-hours. The clinical adverse events observed in the follow-up period during hospitalisation are presented in Table 2, and the rates of 30-day mortality and in-hospital mortality were significantly higher in the patients admitted during off-hours than in those admitted during on-hours (35.7% vs 24.3%; p=0.004; 42.1% vs 30.3%; p=0.005, respectively). However, the incidences of complications, including bleeding, haemolysis, peripheral ischaemia, access-related vascular injury, and cerebrovascular accidents (ischaemia and bleeding), were similar between the 2 groups (26.3% vs 23.7%; p=0.69; 5.3% vs 5.7%; p=0.96; 4.1% vs 4.0%; p=0.97; 2.0% vs 1.9%; p=0.97; 6.6% vs 5.9%; p=0.62, respectively). The comparison of in-hospital outcomes and the frequency of complications between the ECMO combined with Impella group and the Impella alone group is presented in Supplementary Table 1. The rate of 30-day mortality was higher in the ECMO combined with Impella group compared to the Impella alone group (48.9% vs 20.3%; p<0.001). Among complications, the rate of bleeding was higher in the ECMO combined with Impella group compared to the Impella alone group (32.3% vs 21.6%; p=0.04). No significant interaction was identified between ECMO implantation and off-hours admission for the primary outcome (p for interaction=0.34), indicating a consistent effect of off-hours admission on mortality regardless of ECMO implantation.
The Kaplan-Meier curve showed that the all-cause survival probability was significantly lower in patients admitted to hospitals during off-hours than in those admitted during on-hours (log-rank test: p=0.006) (Central illustration). Additionally, we performed multivariable analysis after adjusting for age and sex (model 1). Table 3 shows the Cox regression analysis results with 95% CIs for the association between off-hours admission and all-cause mortality. In model 1, off-hours admission was associated with an increased risk of all-cause mortality (aHR 1.50, 95% CI: 1.10-2.03; p=0.01). We further adjusted for BMI, smoking history, hypertension, hyperlipidaemia, diabetes, chronic kidney disease, previous myocardial infarction, previous angina pectoris, previous heart failure, out-of-hospital cardiac arrest, and in-hospital cardiac arrest in model 2. Off-hours admission was still significantly associated with an elevated risk of all-cause mortality in model 2, model 3 and model 4 (aHR 1.52, 95% CI: 1.03-2.25; p=0.04; aHR 1.55, 95% CI: 1.03-2.31; p=0.03; aHR 1.60, 95% CI: 1.07-2.39; p=0.02, respectively).
Table 2. Clinical adverse events during hospitalisation.
| On-hours admissionn=300 | Off-hours admissionn=266 | p-value | |
|---|---|---|---|
| 30-day mortality | 73 (24.3) | 95 (35.7) | 0.004 |
| Complications | |||
| Bleeding | 79 (26.3) | 63 (23.7) | 0.69 |
| Haemolysis | 14 (5.3) | 17 (5.7) | 0.96 |
| Peripheral ischaemia | 11 (4.1) | 12 (4.0) | 0.97 |
| Access-related vascular injury | 6 (2.0) | 5 (1.9) | 0.97 |
| Cerebrovascular accident | |||
| Ischaemia | 13 (4.3) | 11 (4.1) | 1.00 |
| Bleeding | 7 (2.3) | 4 (1.5) | 0.68 |
| Data are given as n (%). | |||
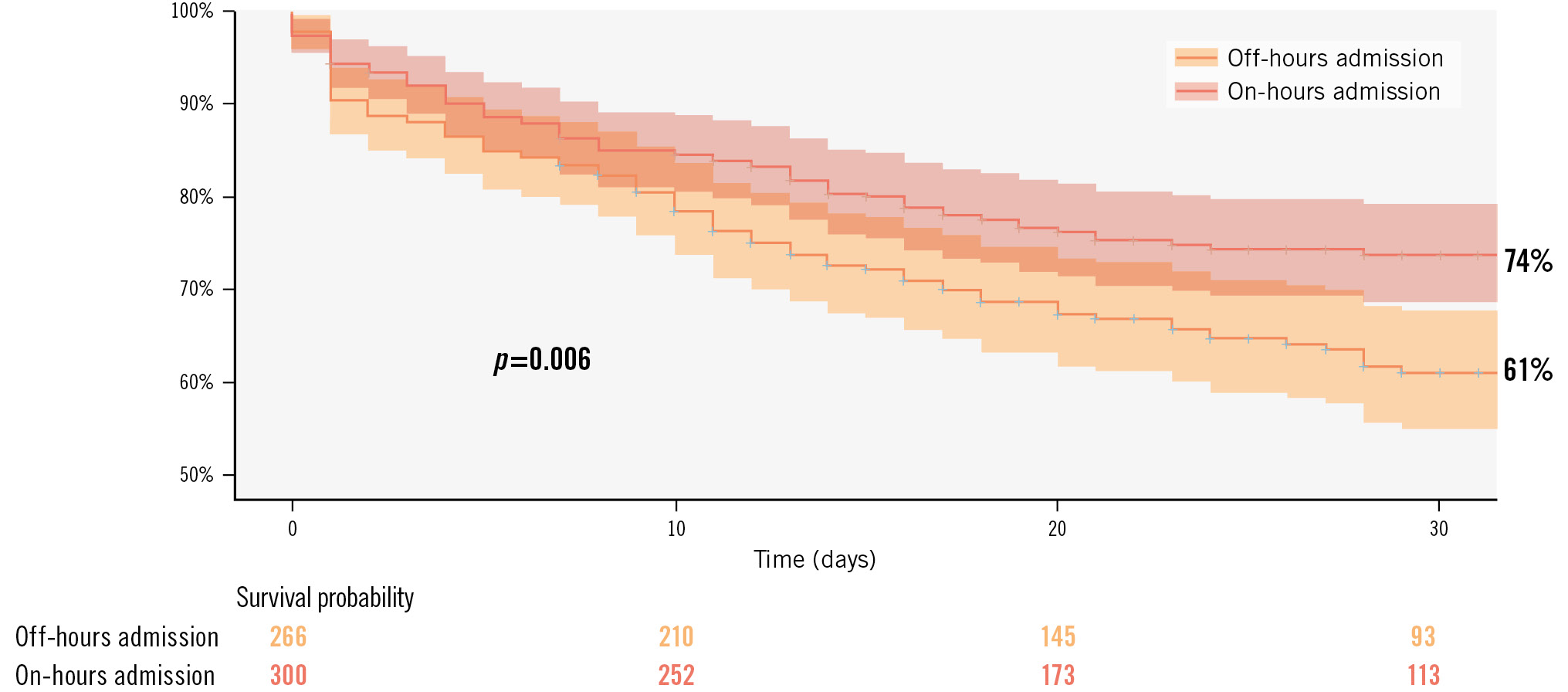
Central illustration. Kaplan-Meier survival estimates of 30-day mortality by the admission time. The Kaplan-Meier curve revealed that the 30-day mortality was significantly higher in patients admitted to hospital during off-hours than in those admitted during on-hours.
Table 3. Multivariable Cox regression analysis for the primary endpoint.
| Multivariable model 1 | Multivariable model 2 | Multivariable model 3 | Multivariable model 4 | |||||
|---|---|---|---|---|---|---|---|---|
| Missing, n (%) | 20 (3.5) | 120 (21.2) | 120 (21.2) | 120 (21.2) | ||||
| HR (95% CI) | p-value | HR (95% CI) | p-value | HR (95% CI) | p-value | HR (95% CI) | p-value | |
| On-hours admission | Reference | - | Reference | - | Reference | - | Reference | - |
| Off-hours admission | 1.50 (1.10, 2.03) | 0.01 | 1.52 (1.03, 2.25) | 0.04 | 1.55 (1.03, 2.31) | 0.03 | 1.60 (1.07, 2.39) | 0.02 |
| Age per SD | 1.19 (1.10, 1.40) | 0.04 | 1.45 (1.13, 1.86) | 0.004 | 1.47 (1.15, 1.88) | 0.003 | 1.49 (1.16, 1.90) | 0.002 |
| Sex | ||||||||
| Female | Reference | - | Reference | - | Reference | - | Reference | - |
| Male | 0.94 (0.64, 1.38) | 0.74 | 1.25 (0.68, 2.30) | 0.47 | 1.20 (0.64, 2.23) | 0.57 | 1.13 (0.61, 2.12) | 0.69 |
| Body mass index | 1.45 (1.14, 1.83) | 0.002 | 1.40 (1.11, 1.76) | 0.004 | 1.40 (1.12, 1.76) | 0.004 | ||
| Smoking | ||||||||
| Non-smoker | Reference | - | Reference | - | Reference | - | ||
| Former smoker | 0.88 (0.52, 1.47) | 0.62 | 0.92 (0.55, 1.55) | 0.76 | 0.98 (0.58, 1.67) | 0.94 | ||
| Current smoker | 0.60 (0.35, 1.02) | 0.06 | 0.61 (0.35, 1.05) | 0.08 | 0.63 (0.37, 1.09) | 0.10 | ||
| Hypertension | 0.63 (0.41, 0.97) | 0.04 | 0.66 (0.42, 1.00) | 0.05 | 0.66 (0.42, 1.02) | 0.06 | ||
| Hyperlipidaemia | 0.92 (0.61, 1.38) | 0.68 | 0.89 (0.59, 1.34) | 0.57 | 0.85 (0.56, 1.29) | 0.46 | ||
| Diabetes | 1.18 (0.79, 1.75) | 0.42 | 1.18 (0.79, 1.76) | 0.41 | 1.22 (0.82, 1.83) | 0.33 | ||
| Chronic kidney disease | 1.15 (0.74, 1.78) | 0.53 | 1.18 (0.76, 1.84) | 0.46 | 1.30 (0.82, 2.04) | 0.26 | ||
| Previous myocardial infarction | 0.95 (0.50, 1.81) | 0.87 | 1.02 (0.52, 2.00) | 0.95 | 0.99 (0.51, 1.91) | 0.97 | ||
| Previous angina pectoris | 1.66 (0.89, 3.09) | 0.11 | 1.42 (0.75, 2.69) | 0.28 | 1.37 (0.72, 2.62) | 0.34 | ||
| Previous heart failure | 1.54 (0.78, 3.07) | 0.22 | 1.91 (0.94, 3.91) | 0.08 | 1.83 (0.89, 3.74) | 0.10 | ||
| Out-of-hospital cardiac arrest | 1.82 (1.12, 2.98) | 0.02 | 1.59 (0.96, 2.64) | 0.07 | 1.64 (0.99, 2.71) | 0.06 | ||
| In-hospital cardiac arrest | 1.90 (1.25, 2.89) | 0.003 | 1.41 (0.89, 2.23) | 0.14 | 1.43 (0.90, 2.26) | 0.13 | ||
| ECMO implantation | 2.38 (1.51, 3.76) | <0.001 | 2.40 (1.53, 3.77) | <0.001 | ||||
| DTB time | 1.04 (0.76, 1.41) | 0.81 | 1.05 (0.77, 1.42) | 0.77 | ||||
| DTU time | 0.84 (0.62, 1.14) | 0.27 | 0.82 (0.61, 1.12) | 0.22 | ||||
| Hospital intervention volume | ||||||||
| Bottom tertile | Reference | - | ||||||
| Middle tertile | 0.63 (0.39, 1.02) | 0.06 | ||||||
| Top tertile | 0.82 (0.33, 0.91) | 0.02 | ||||||
| CI: confidence interval; DTB: door-to-balloon; DTU: door-to-unload; ECMO: extracorporeal membrane oxygenation; HR: hazard ratio; SD: standard deviation | ||||||||
ASSOCIATION BETWEEN ADMISSION TIME AND PROGNOSIS ON WEEKDAYS
A total of 425 (75.1%) patients were hospitalised on weekdays. In model 1, off-hours admissions were an independent predictor of 30-day mortality (aHR 1.52, 95% CI: 1.05-2.19; p=0.03). However, in model 2, this relationship was attenuated, and no statistically significant association was observed between off-hours admissions and 30-day mortality (aHR 1.54, 95% CI: 0.96-2.46; p=0.07). In model 1, we further examined more specific times, segmenting admission times into 4-hour intervals, and evaluated the relationship between admission time and mortality. When patients were classified into 6 groups based on the time of admission, 122 (28.7%) were admitted from 8:00 a.m. to 11:59 a.m., 105 (24.7%) from 12:00 p.m. to 3:59 p.m., 72 (16.9%) from 4:00 p.m. to 7:59 p.m., 44 (10.4%) from 8:00 p.m. to 11:59 p.m., 37 (8.7%) from 12:00 a.m. to 3:59 a.m., and 45 (10.6%) from 4:00 a.m. to 7:59 a.m. The 30-day mortality rates for these groups were 21.3%, 24.8%, 29.2%, 34.1%, 37.8%, and 40.0%, respectively. Among these groups, admission between 4:00 a.m. and 7:59 a.m. was significantly associated with 30-day mortality (odds ratio 2.30, 95% CI: 1.09-4.85; p=0.03) (Supplementary Figure 1).
Discussion
OFF-HOURS EFFECT IN PATIENTS WITH STEMI-CS TREATED WITH IMPELLA
This study investigated the short-term prognosis of consecutive patients who underwent primary PCI for STEMI using Impella for cardiogenic shock. Given recent data showing a significant reduction in mortality in patients with CS due to STEMI treated with Impella15, the findings of this study are crucial, as they may be associated with a potential improvement in the prognosis of this population16. To the best of our knowledge, this is the first cohort study using national-level Impella registry data to evaluate the impact of the “off-hours effect” on the strategy of Impella support for patients with STEMI-CS. The main findings are as follows. 1) The 30-day mortality rate was higher during off-hours than during on-hours, with off-hours admissions being associated with an approximately 60% increase in the risk of 30-day mortality. 2) Among patients with STEMI who received Impella in current Japanese acute care settings, patient characteristics and the frequency of complications were comparable between those who were admitted during off-hours and on-hours. 3) Admission from 4:00 a.m. to 7:59 a.m. was an independent predictor of 30-day mortality when limited to weekday admissions. 4) The DTB and DTU times were significantly longer in the patients who were admitted during off-hours than those who were admitted during on-hours.
The potential reasons for the higher mortality rate in patients with STEMI during off-hours admission include a lower frequency of coronary angiography during off-hours17, prolonged time to reperfusion18, lower rates of PCI performed within the recommended time19, increased decision-making errors due to staff fatigue or sleep deprivation20, a delay in acute-phase treatment due to diagnostic assessment in the emergency department821, and the availability of fewer medical staff at night622. These factors are reportedly interlinked, suggesting a combined effect on worsening patient outcomes. In our study, even after adjusting for various patient characteristics, off-hours admissions remained an independent predictor of mortality. The likelihood that differences in patient characteristics could explain the increased mortality rate in patients admitted at weekends was low. The disparity based on admission time is crucial, as it is not solely due to patient-related factors, implying an urgent need for revisions in the medical system.
CHALLENGES IN IMPROVING OUTCOMES FOR OFF-HOURS ADMISSIONS
Previous reports have indicated that the mortality rates for patients with AMI presenting during off-hours are worse than those of patients presenting during on-hours214. Conversely, some studies have suggested that the short-term prognosis remains unchanged regardless of admission during on- or off-hours23, leading to inconsistent findings. Such discrepancies can be attributed to many factors, including differences in study populations, variations in disease severity, and different definitions of off-hours24. Our study specifically focused on patients with STEMI-CS, which may show different implications from conventional STEMI cases during off-hours. Notably, in our cohort, while the frequency of Impella-related complications remained unchanged between the groups, the short-term prognosis was heavily influenced by off-hours admissions, suggesting that postprocedural patient management in the intensive care unit (ICU), rather than procedural complications, significantly affects patient outcomes. Several reports have highlighted the profound effect of ICU admissions during off-hours242526. Patients with STEMI-CS may be more susceptible to the effects of off-hours admission than the general STEMI population. Continuous efforts have been made to improve outcomes for patients admitted during off-hours by ensuring equitable, evidence-based treatment, regardless of admission timing27. However, despite the stringent criteria set for treatment with Impella in Japan − encompassing rigorous facility capabilities, staff requirements, and expertise − our findings imply that the current night-time healthcare infrastructure remains inadequate, especially considering the implications for STEMI-CS patient outcomes. However, the use of Impella to treat cardiogenic shock is rapidly increasing. A recently published randomised trial, the DanGer Shock Trial, demonstrated the effectiveness of Impella in reducing mortality in patients with STEMI-CS15. The high rate of adverse events in the Impella-alone group emphasises the importance of management and monitoring protocols, especially during off-hours. Furthermore, a cohort study involving 1,010 hospitals in the USA from 2009 to 2016 revealed significant variations in Impella-related clinical practices. Facilities with higher Impella implantation volumes reported superior survival rates when Impella was used as the initial support strategy28. This interfacility discrepancy may further exacerbate the off-hours effect. Standardised shock protocols emphasising best practices with Impella have been highlighted to improve outcomes. Factors such as patient selection for Impella, timing of implantation, and post-implant management in cardiac ICUs are pivotal for its success. Therefore, implementing such standardised protocols could potentially bridge the gap in clinical outcomes between the daytime and the night-time2930.
Limitations
First, this registry only included individuals who were treated with Impella; therefore, this study did not account for those who could not receive Impella treatment because of off-hours admission. Consequently, due to the nature of this cohort, information related to the “weekend effect” associated with the introduction of Impella or comparisons between patients who received Impella treatment and those who did not could not be obtained, making it impossible to establish a control group. Second, the generalisability of the findings is a concern. As is common in all off-hours studies, the healthcare system during off-hours might vary by region, and patient characteristics and healthcare systems may also differ regionally. Therefore, caution should be exercised when extrapolating these findings to other regions and nations. Third, our analysis did not consider factors related to medical services in the prehospital stage. Reports have indicated that off-hours admission may be associated with adverse outcomes in prehospital medical services31. This could potentially exacerbate the outcomes of patients with STEMI-CS admitted during off-hours, and this aspect warrants further investigation in future studies. Finally, since our registry is set up focusing on Impella, it does not contain detailed information on the PCI procedural details or postoperative cardiovascular intensive care unit (CICU) information, and we were unable to obtain information on the culprit lesion, Thrombolysis in Myocardial Infarction flow, any complications of the PCI itself, CICU systems, or details of on-call physicians.
Conclusions
Our findings indicate the persistence of the “off-hours effect” in cases of STEMI-CS patients treated with Impella. Healthcare professionals should continue to address the disparities caused by existing temporal factors in cardiovascular care by striving to improve the timely provision of evidence-based treatments and enhancing off-hours medical services.
Impact on daily practice
In patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock (STEMI-CS) treated with Impella, we observed the “off-hours effect”. In the Japanese Impella registry dataset, off-hours admissions are associated with an increased risk of all-cause mortality for patients with STEMI-CS compared to on-hours admissions. The issue of the “off-hours effect” still persists, highlighting the need for further evaluation of improvement measures. Healthcare providers must be aware of this admission time disparity and continue efforts to provide optimised care and services, especially during off-hours.
Acknowledgements
We thank all members of the Japan Registry for Percutaneous Ventricular Assist Device (J-PVAD).
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.