Abstract
Background: Mechanical thrombectomy is the most effective treatment for restoring reperfusion in large vessel occlusion acute ischaemic stroke, even in patients with posterior circulation. However, the strategy for optimal treatment of patients with acute basilar artery occlusion (BAO) in difficult-to-treat cases in which thrombectomy has failed is unknown.
Aims: The purpose of this study was to evaluate the clinical efficacy and safety of rescue intracranial stenting (RIS) in patients with acute BAO treated with thrombectomy.
Methods: Stroke patients with acute BAO who had undergone failed mechanical thrombectomy in the ATTENTION registry were enrolled in this study. Univariable and multivariable regression analyses were performed to assess the clinical efficacy and safety of RIS.
Results: A total of 477 patients were included in the analysis, and 346 patients underwent RIS, of whom 167 (35.0%) patients had a favourable outcome. Symptomatic intracranial haemorrhage (sICH) occurred in 24 (5.0%) patients, and 172 (36.1%) patients died. There were no significant differences between the two groups of patients in the outcomes of modified Rankin Scale (mRS) 0-1 (p=0.541), mRS 0-2 (p=0.374), mRS 0-3 (p=0.600), or death (p=0.706). Patients in the RIS+ group had a significantly higher incidence of sICH (1.5% vs 6.4%; p=0.031). Nevertheless, after adjusting for confounders, RIS was not found to be an independent risk factor for sICH (adjusted odds ratio 4.189, 95% confidence interval: 0.960-18.286; p=0.057).
Conclusions: In this national, multicentre, prospective study, RIS in patients with acute BAO who had undergone failed first-line thrombectomy was feasible, but we could not show significance regarding improved long-term outcomes. Trial registration number: ChiCTR2000041117.
Since 2015, multiple randomised controlled trials (RCTs)123 have demonstrated the efficacy and safety of mechanical thrombectomy (MT) in treating stroke, representing a revolutionary breakthrough for neurointerventional therapy. In particular, among patients with large vessel occlusion (LVO) strokes in the anterior circulation, according to a meta-analysis of five major RCTs conducted in 2016, MT can increase the rate of favourable 90-day outcomes by 46.0%4, more than double that of conventional treatment groups, further confirming the value of MT.
However, the situation is vastly different in LVO strokes in the posterior circulation. The poor neurological prognosis and high rates of disability and mortality in these cases remain unresolved, presenting a significant challenge in the treatment of stroke and the development of MT. Fortunately, in two studies published in 2022, ATTENTION and BAOCHE56, researchers provided high-quality evidence from clinical trials to demonstrate the safety and effectiveness of MT in treating acute basilar artery occlusion (BAO), offering new hope for this patient population.
Despite its notable successes, MT remains insufficient or even ineffective in certain challenging or refractory cases, with no established solution widely recognised in the medical community, especially for LVO strokes in the posterior circulation. For those patients who fail to achieve successful recanalisation following MT, rescue intracranial stenting (RIS) may be a better option compared to failed reperfusion. Unfortunately, current evidence supporting the use of such interventions in acute BAO patients is limited and controversial with high variability7891011.
Therefore, it is imperative to evaluate whether RIS is suitable for those refractory cases of acute BAO with failed first-line MT therapy, allowing us to optimise our revascularisation strategies and improve patient outcomes.
To address this gap, using a nationwide multicentre prospective study, we have evaluated the clinical efficacy and safety of RIS in patients with acute BAO following failed initial thrombectomy, aiming to maximise the benefits of early endovascular treatment for these patients.
Methods
Study population
This study was a retrospective analysis of prospectively collected data. Patient information for this study was sourced from the ATTENTION registry, a large-scale, multicentre, prospective, and validated database encompassing 2,134 subjects recruited from 48 comprehensive stroke centres across 22 Chinese provinces from March 2017 to February 202112. Details of the registry’s study design and inclusion criteria have been described in previous publications12. For the present analysis, we focused on the subset of 1,672 patients diagnosed with acute BAO who received MT as part of the ATTENTION registry study. If repeated thrombectomy attempts resulted in modified treatment in cerebral ischaemia (mTICI) grades13 of 0-2a, it was considered a failed first-line MT. Patients were divided into two groups: (1) RIS+: rescue stenting after failed reperfusion (all patients who underwent stenting regardless of recanalisation); (2) RIS–: no stenting after failed reperfusion (unsuccessful recanalisation and no stenting).
Ethical approval for this research was granted by the Medical Research Ethics Committee of Anhui Provincial Hospital (approval number: 2020KY Audit No. 202). Written informed consent was acquired from each participating individual or their legal representative. The ATTENTION registry is also registered with the Chinese Clinical Trial Registry (registration number: ChiCTR2000041117), accessible online at http://www.chictr.org.cn.
Stenting and data collection
There was no predetermined limit to the number of passes/attempts before deciding on RIS. Selection of the stent type and implantation method was left to the discretion of the operator based on vessel characteristics and lesion morphology. Post-stenting, all patients received antiplatelet therapy consisting of clopidogrel (75 mg/day) and/or aspirin (100 mg/day) unless there were some symptomatic haemorrhagic complications.
Data utilised in this study came from the ATTENTION registry, which prospectively collected clinical information including demographics (age, sex), medical history (atrial fibrillation, hypertension, diabetes mellitus, hyperlipidaemia, coronary heart disease, transient ischaemic attack/stroke), clinical features (systolic/diastolic blood pressure, National Institutes of Health Stroke Scale [NIHSS] score, posterior circulation Alberta stroke program early computed tomography score [pc-ASPECTS], aetiology classification based on Trial of ORG 10172 in Acute Stroke Treatment (TOAST) criteria14, intravenous thrombolysis, onset-to-admission [OTA] time, assessment of collateral circulation according to the American Society of Interventional and Therapeutic Neuroradiology collateral grading system13, occlusion site), first thrombectomy technique, admission-to-puncture time, number of passes, and outcomes (modified Rankin Scale [mRS] score at 90 days, death, symptomatic intracranial haemorrhage [sICH]). The estimated time of BAO was defined as the moment when symptoms consistent with a clinical diagnosis of BAO stroke were first noticed, as judged by the treatment team based on patient or witness descriptions; alternatively, if the exact time was unknown, it was recorded as the last time the patient was seen to be well. sICH was assessed within 3 days of admission and was defined as an increase of ≥4 points in the NIHSS score with any intracranial haemorrhage on neuroimaging15. The mRS is a measure of functional independence that effectively assesses long-term recovery in patients, encompassing self-care ability and daily activity performance. In alignment with recent landmark studies in the realm of basilar artery thrombectomy, we adopted the mRS score as a pivotal long-term prognostic indicator to appraise the therapeutic efficacy56. Follow-up evaluations of mRS scores were completed either over the phone or the patient had an outpatient visit.
Statistical analysis
Depending on their distribution, continuous variables were examined through the Student’s t-test or the Kruskal-Wallis test. Categorical data were analysed using the χ2 test. For the 12 variables with missing values (ranging from 0.2% to 18.9%), multiple imputation by chained equations (MICE) was employed to reduce any selection bias caused by the exclusion of patients with incomplete baseline data. Rubin’s rules were applied in the handling of missing data. Predictive mean matching was used for continuous variables, while ordered or binary logistic regression models were used for categorical variables to generate 10 complete datasets. Separate univariable and multivariable logistic regression analyses were then conducted to explore the relationship between patient-related prognostic outcomes and the studied variables. The outcome variables included in the analysis had complete data and were only used as auxiliary variables during multiple imputations to predict missing values for other variables. All variables with missing values were included in the imputation process. Potential confounders that we adjusted for in the final regression analysis included age, sex, and coronary heart disease. All statistical analyses were carried out using R software, version 4.1.0 (R Foundation for Statistical Computing), with a significance level set at p<0.05.
Results
Ultimately, our analysis included a total of 477 patients who had undergone failed first-line MT, as depicted in Figure 1. Of these, 346 (72.5%) underwent RIS, and 309 (89.3%) achieved successful reperfusion after RIS. Baseline characteristics and comparisons between the RIS+ and RIS– groups are shown in Table 1. The distribution of 90-day mRS scores across both the RIS+ and RIS– groups is presented in Figure 2.
As shown in Table 1, there were only significant differences in sex and coronary artery disease between the RIS+ and RIS– groups, with male patients more likely to receive RIS (76.0% vs 63.4%; p=0.006) and coronary artery disease less prevalent in the RIS+ group (8.7% vs 17.0%; p=0.019). Table 2 shows the differences in clinical efficacy and safety outcomes between the two groups of patients. We can notice that there were no significant differences in 90-day mRS, mRS 0-1, mRS 0-2, mRS 0-3, or death (Central illustration). However, sICH occurred at a significantly higher frequency in the RIS+ group compared to the RIS– group (6.4% vs 1.5%; p=0.031).
As presented in Table 3, the results of univariable regression analyses revealed a significant positive correlation between RIS and sICH (odds ratio [OR] 4.380, 95% confidence interval [CI]: 1.016-18.885; p=0.048). After adjusting for potential confounding factors, however, we did not observe strong associations between RIS and any of the clinical outcomes (primary clinical outcome: mRS 0-2; secondary clinical outcomes: mRS 0-1 and mRS 0-3) or safety endpoints (sICH and death). Nonetheless, RIS was not an independent risk factor for sICH (adjusted OR 4.189, 95% CI: 0.960-18.286; p=0.057).
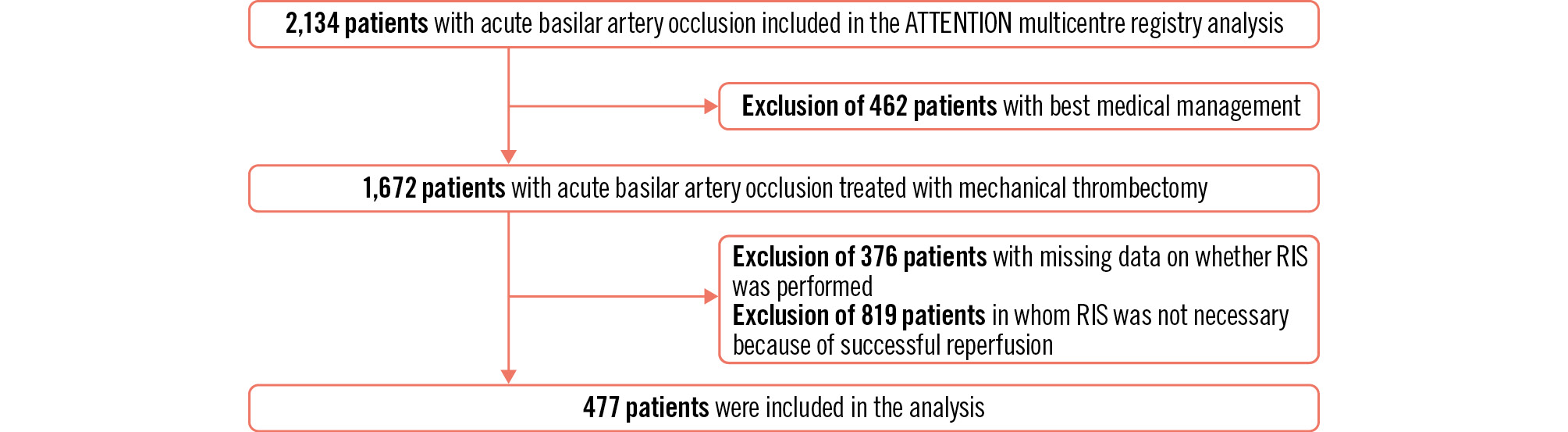
Figure 1. Study flowchart. RIS: rescue intracranial stenting
Table 1. Baseline characteristics and comparisons between the RIS+ and RIS– groups.
| Baseline variables | Overall (n=477) | RIS– (n=131) | RIS+ (n=346) | p-value |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 64.00 [55.00, 71.00] | 66.00 [56.00, 73.00] | 64.00 [55.00, 71.00] | 0.088 |
| Male | 346 (72.5) | 83 (63.4) | 263 (76.0) | 0.006# |
| Medical history | ||||
| Atrial fibrillation* | 131 (32.8) | 29 (27.4) | 102 (34.7) | 0.168 |
| Hypertension* | 298 (72.9) | 81 (69.8) | 217 (74.0) | 0.385 |
| Diabetes mellitus* | 110 (26.9) | 27 (23.7) | 83 (28.1) | 0.363 |
| Hyperlipidaemia* | 128 (32.5) | 41 (36.9) | 87 (30.7) | 0.238 |
| Coronary artery disease* | 44 (10.9) | 18 (17.0) | 26 (8.7) | 0.019# |
| Transient ischaemic attack or stroke* | 89 (22.2) | 26 (23.0) | 63 (21.9) | 0.806 |
| Clinical features | ||||
| Systolic blood pressure* | 150.00 [135.00, 165.00] | 150.00 [132.50, 164.00] | 150.00 [136.00, 165.00] | 0.383 |
| Diastolic blood pressure* | 83.00 [76.50, 94.50] | 85.00 [78.50, 94.00] | 83.00 [76.00, 95.00] | 0.581 |
| NIHSS* | 20.00 [12.75, 30.00] | 21.00 [13.25, 29.00] | 20.00 [12.00, 30.00] | 0.704 |
| pc-ASPECTS | 9.00 [8.00, 10.00] | 9.00 [8.00, 10.00] | 9.00 [8.00, 10.00] | 0.637 |
| Aetiological type* | 0.559 | |||
| Cardioembolism | 138 (33.9) | 42 (37.2) | 96 (32.7) | |
| Large artery atherosclerosis | 179 (44.0) | 45 (39.8) | 134 (45.6) | |
| Other or unknown | 90 (22.1) | 26 (23.0) | 64 (21.8) | |
| Intravenous thrombolysis | 126 (26.4) | 39 (29.8) | 87 (25.1) | 0.306 |
| OTA time | 327.00 [216.00, 572.00] | 288.00 [213.50, 523.00] | 339.50 [223.00, 596.25] | 0.208 |
| Admission-to-puncture time | 91.00 [76.00, 131.00] | 92.00 [77.50, 136.00] | 91.00 [76.00, 128.75] | 0.575 |
| Collateral circulation status* | 0.00 [0.00, 1.00] | 0.00 [0.00, 2.00] | 0.00 [0.00, 1.00] | 0.780 |
| Occlusion site | 0.688 | |||
| Distal | 168 (35.2) | 47 (35.9) | 121 (35.0) | |
| Middle | 146 (30.6) | 43 (32.8) | 103 (29.8) | |
| Proximal | 163 (34.2) | 41 (31.3) | 122 (35.3) | |
| First thrombectomy technique | 0.674 | |||
| Aspiration | 96 (20.1) | 27 (20.6) | 69 (19.9) | |
| Stent-retriever based techniques | 300 (62.9) | 85 (64.9) | 215 (62.1) | |
| Other† | 81 (17.0) | 19 (14.5) | 62 (17.9) | |
| Number of passes* | 2.00 [1.00, 3.00] | 2.00 [1.00, 3.00] | 2.00 [1.00, 3.00] | 0.758 |
| Values are n (%) or median [interquartile range]. *The data were partially missing (0.20-18.87%). †Balloon dilatation with or without intra-arterial thrombolysis was included. #Statistically significant values. NIHSS: National Institutes of Health Stroke Scale; OTA: onset-to-admission; pc-ASPECTS: posterior circulation Alberta stroke program early computed tomography score; RIS: rescue intracranial stenting | ||||
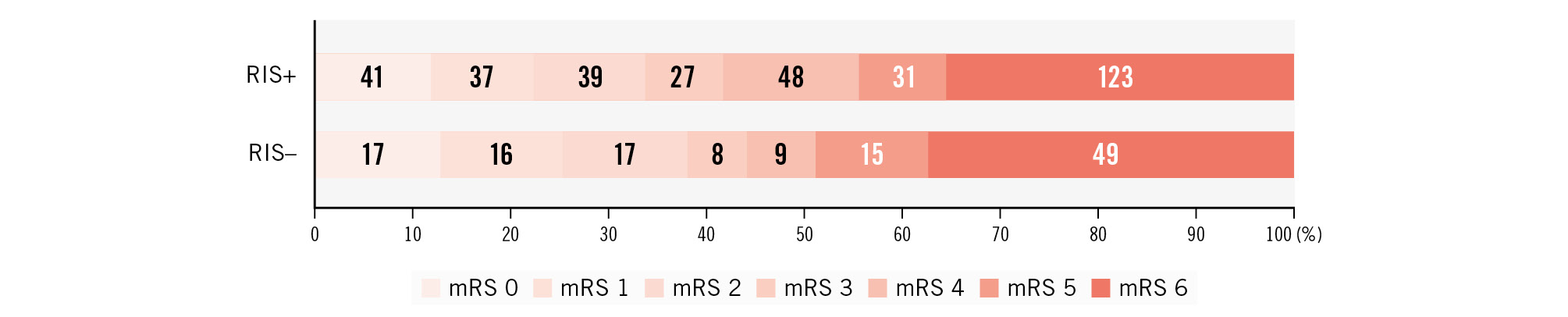
Figure 2. Distribution of 90-day modified Rankin Scale scores in RIS+ and RIS– groups. mRS: modfied Rankin Scale; RIS: rescue intracranial stenting
Table 2. Clinical efficacy and safety outcomes in the RIS+ and RIS– groups.
| Outcomes | Overall (n=477) | RIS– (n=131) | RIS+ (n=346) | p-value |
|---|---|---|---|---|
| 90-day mRS | 4.00 [2.00, 6.00] | 4.00 [1.50, 6.00] | 4.00 [2.00, 6.00] | 0.941 |
| Primary clinical outcome | ||||
| mRS 0-2 | 167 (35.0) | 50 (38.2) | 117 (33.8) | 0.374 |
| Secondary clinical outcomes | ||||
| mRS 0-1 | 111 (23.3) | 33 (25.2) | 78 (22.5) | 0.541 |
| mRS 0-3 | 202 (42.4) | 58 (44.3) | 144 (41.6) | 0.600 |
| Safety endpoints | ||||
| sICH | 24 (5.0) | 2 (1.5) | 22 (6.4) | 0.031 |
| Death | 172 (36.1) | 49 (37.4) | 123 (35.6) | 0.706 |
| Values are n (%) or median [interquartile range]. mRS: modified Rankin Scale; RIS: rescue intracranial stenting; sICH: symptomatic intracranial haemorrhage | ||||

Central illustration. Outcomes of RIS after failed thrombectomy for acute basilar artery occlusion. RIS in patients with acute basilar artery occlusion who had undergone failed first-line thrombectomy was feasible, but significance regarding improved long-term outcomes was not demonstrated. mRS: modified Rankin Scale; RIS: rescue intracranial stenting; sICH: symptomatic intracranial haemorrhage
Table 3. Uni/multivariable regression analyses of rescue intracranial stenting and outcomes.
| Outcomes | Unadjusted OR (95% CI) | p-value | Adjusted* OR (95% CI) | p-value |
|---|---|---|---|---|
| Primary clinical outcome | ||||
| mRS 0-2 | 0.828 (0.545-1.256) | 0.375 | 0.770 (0.502-1.181) | 0.232 |
| Secondary clinical outcomes | ||||
| mRS 0-1 | 0.864 (0.541-1.380) | 0.542 | 0.778 (0.481-1.258) | 0.307 |
| mRS 0-3 | 0.897 (0.598-1.346) | 0.601 | 0.824 (0.543-1.252) | 0.365 |
| Safety endpoints | ||||
| sICH | 4.380 (1.016-18.885) | 0.048 | 4.189 (0.960-18.286) | 0.057 |
| Death | 0.923 (0.608-1.400) | 0.707 | 1.005 (0.654-1.546) | 0.981 |
| *Adjusted for potential confounders such as age, sex, and coronary artery disease. CI: confidence interval; mRS: modified Rankin Scale; OR: odds ratio; sICH: symptomatic intracranial haemorrhage | ||||
Discussion
This study investigated the clinical efficacy and safety of implementing RIS in patients with acute BAO after failed first-line MT. The results showed that the utilisation of RIS failed to significantly improve clinical outcomes (including mRS 0-1, mRS 0-2, mRS 0-3, and death) in patients with acute BAO.
The incidence, prevalence, and mortality rates of stroke have been rising in recent years, with a trend towards younger ages, placing a heavy burden on patients themselves, their families, and society16. Consistent results from previous RCTs indicate that endovascular treatment for LVO in the anterior circulation significantly improves patient functional outcomes4. While MT has become an important treatment method for LVO, its therapeutic effect in patients with posterior circulation LVO remains unsatisfactory17. With the development of neurointerventional technology in recent years, it was only upon release of the ATTENTION and BAOCHE studies56 in 2022 that patients with acute BAO finally gained new hope. Notably, in these two studies, the proportion of rescue intracranial angioplasty/stent implantation reached as high as 40%-55%56. However, even after rescue intracranial angioplasty/stent implantation, recanalisation was still unsuccessful in 7%-12% of acute BAO patients56. Furthermore, the application of rescue intracranial stenting in LVO of the posterior circulation is relatively uncommon, leaving its clinical significance to be further explored.
Our study shows that, while RIS may be effective for some patients and improve reperfusion status (with 89.3% achieving successful reperfusion after RIS), it does not show significant advantages in reducing the mortality rate or improving long-term prognosis. This is a noteworthy and controversial issue, as some previous reports have suggested that RIS significantly improves patient prognosis, and some studies disagree1118192021. There are several possible reasons for this discrepancy. On the one hand, most studies on RIS mainly focus on anterior circulation occlusions, whereas our study specifically targeted patients with acute BAO, whose anatomy, pathophysiology, and response to treatment differ greatly from those with anterior circulation occlusions. Therefore, the efficacy of RIS may vary in these different populations. On the other hand, even within studies targeting posterior circulation, their sample sizes remain low. In the SAINT study analysis, only 84 patients underwent RIS and had better functional independence and safety outcomes compared to RIS– patients, with no significant difference in sICH (5.1% vs 10.9%; p=0.29)18. Due to their small sample size, they cannot provide high-quality evidence-based medical recommendations. Balloon angioplasty and stent implantation are highly technical surgeries with potentially higher complication rates than that of simple MT, especially in patients with posterior circulation occlusions. This means that, in actual applications, the clinical benefits and safety of RIS need to be evaluated more cautiously to ensure that more patients with acute BAO benefit from it.
The utilisation of postoperative dual antiplatelet therapy in conjunction with intravenous thrombolysis may elevate the risk of haemorrhagic transformation. However, our study observed a similar proportion of intravenous thrombolysis between the two groups, with a lower rate in the RIS+ group (25.1% vs 29.8%; p=0.306). Notwithstanding this, patients who received RIS exhibited higher rates of sICH (6.4% vs 1.5%; p=0.031). Considering the grave consequences of sICH, this necessitates our vigilant attention, even though, post-adjustment for confounding variables, no significant correlation was found between RIS and sICH. Subsequent research endeavours should concentrate on delving into the association and potential mechanisms linking rescue intracranial stenting during posterior circulation thrombectomy and sICH.
In our current investigation, 32.7% of patients in the RIS+ group had a cardioembolic aetiology, a percentage akin to that of the RIS– group but lower than cases attributed to large artery atherosclerosis (45.6%). The presence of intracranial atherosclerotic narrowing in the affected blood vessel was not the sole determinant for stent placement. Other reasons were dissection, failed opening, re-thrombosis, etc. During thrombectomy procedures, if the thrombus burden is substantial or lodged in intricate locations like vascular bifurcations or tortuous segments, incomplete or unsuccessful clot removal may occur. Furthermore, mechanical injury to the arterial wall, such as dissection, could transpire during the retrieval process. Even post-thrombectomy, residual clots may persist within the vessel, impeding effective reperfusion. Hence, under such circumstances, opting for a strategy involving the deployment of a stent via RIS to bolster and sustain the patency of the occluded vessel is a justifiable course of action. In this study, the types of intracranial stents utilised included Apollo (MicroPort Scientific Corporation), Neuroform EZ (Stryker), Enterprise (Johnson & Johnson MedTech), and Solitaire X (Medtronic), among others. The use of these stents deviated to varying degrees from their intended use as per instructions for use and were chosen primarily due to their moderate radial strength, improved navigability through tortuous and complex vasculature, enhanced deliverability, and wider size options, all of which made them preferred choices for the treatment of symptomatic intracranial arterial stenosis. Notably, despite being used off-label, there is substantial evidence from multiple studies and clinical practice demonstrating that such stents exhibit favourable safety and efficacy profiles in intracranial endovascular interventions, providing solid grounds for our selection222324.
Among the 346 patients who underwent RIS treatment (accounting for 72.5% of the total), 37 patients (10.7%) underwent unsuccessful recanalisation post-procedure. Further analysis revealed that regardless of whether recanalisation was achieved following RIS, there was no significant difference in favourable prognosis rates across subgroups: 34.3% of patients with successful recanalisation via RIS had a favourable prognosis (106/309), while 29.7% of patients without successful recanalisation despite RIS still had a favourable prognosis (11/37). Statistical testing indicated that the difference in favourable prognosis rates between these two subgroups was not statistically significant (p=0.578).
RIS is not always the best choice for every patient with a failed thrombectomy for acute BAO. The potential complications associated with RIS should be considered when selecting suitable candidates for this treatment, rather than striving for perfect recanalisation in every patient. There are many challenges in effectively utilising RIS to improve patient outcomes. Before deciding on RIS, a thorough evaluation of the risks and benefits for each patient is crucial, along with efforts to optimise their neurological function outcome. Additionally, enhanced monitoring and management measures during and after surgery, such as the use of antithrombotics and blood pressure control, are necessary to ensure the safety of RIS. As technology advances, personalised treatment strategies tailored to individual patient needs will likely be required to maximise the benefits of RIS.
Limitations
Despite these findings, our study also has some limitations. Firstly, it focuses primarily on Asian populations in China and may not be generalisable to other ethnicities worldwide, despite having a large sample size. Secondly, data regarding coronary heart disease, a potential confounder adjusted in this study, were partially missing. However, MICE was used to mitigate the impact of this factor, ensuring the credibility and scientific rigour of our results. The study design was not a randomised controlled trial. In terms of postoperative blood pressure management protocols, we relied on the standard clinical practice of participating centres and the clinical judgment of physicians, and there was no standardised blood pressure management protocol. Furthermore, this study did not record the time passed between hospital arrival or arterial puncture to stent placement, nor did it record peri- and postprocedural antiplatelet or anticoagulation medication; monitoring for early stent occlusion was not performed, nor testing for clopidogrel resistance genotypes. These omissions constrain our ability to conduct a thorough analysis of the impact of antiplatelet/anticoagulant therapy on the prevalence of sICH, stent thrombosis, success rates of interventional procedures and patient outcomes. Thirdly, our assessment of the collateral circulation would not have fully captured all critical anatomical variations, such as the degree of posterior circulation supply via the anterior circulation, the presence of a proximal P1 segment occlusion, and the potential impact of a Percheron artery. These factors could play a pivotal role in determining patients’ clinical outcomes. Fourthly, the inherent limitations of observational studies apply here, such as variations in operator experience and decision-making around RIS procedures and types of implanted stents. However, due to the variability of the vessels and collateral anatomy, fluctuating symptoms and the inherent variability of procedural protocols, any large-scale randomised studies are presently unlikely.
Conclusions
While RIS after failed MT for patients with acute BAO was feasible, RIS failed to demonstrate significant improvement in neurological outcomes. Future studies should consider covariables such as collaterals, variability in anatomy, antiplatelet/anticoagulation regimens, platelet aggregability testing, genotyping and time from initial imaging to the end of procedure.
Impact on daily practice
We evaluated the clinical efficacy and safety of rescue intracranial stenting (RIS) in patients with acute basilar artery occlusion stroke in whom thrombectomy failed to achieve recanalisation. Our results revealed that RIS was feasible and safe. However, within the constraints of our study, we could not demonstrate a significant improvement in long-term functional outcome. Practically, this implies that RIS can be considered for acute basilar artery occlusion when thrombectomy fails, but our findings underscore the complexity of decision-making for acute stroke interventions, advocating refined patient selection and ongoing research to optimise outcomes in challenging scenarios.
Acknowledgements
We thank all relevant clinicians, statisticians, and other technical staff.
Funding
This work has been supported in part by these grants: the Suzhou Science and Technology Bureau Medical-Industrial Collaborative Innovation Research Project (SLJ2021014) and the Suzhou Medical and Health Science and Technology Innovation (SKY2022160).
Conflict of interest statement
The authors have no conflicts of interest to declare.