Abstract
BACKGROUND: Same-day discharge (SDD) in patients undergoing percutaneous coronary intervention (PCI) of a chronic total occlusion (CTO) is appealing because of the increased patient comfort. However, data on SDD following large-bore vascular access are scarce.
AIMS: We investigated the feasibility and safety of SDD in patients undergoing large-bore CTO PCI.
METHODS: Between 2013 and 2023, 948 patients were prospectively enrolled in a single-centre CTO registry and underwent CTO PCI. SDD was pursued in all patients. Large-bore access was defined as the use of ≥7 French (Fr) sheaths in ≥1 access site. A logistic regression analysis was used to identify predictors for non-SDD. Clinical follow-up was obtained at 30 days.
RESULTS: SDD was observed in 62% of patients. Large-bore access was applied in 99% of the cohort. SDD patients were younger and more often male, with lower rates of renal insufficiency and prior coronary artery bypass grafting. Local access site bleeding (odds ratio [OR] 8.53, 95% confidence interval [CI]: 5.24-13.87) and vascular access complications (OR 7.23, 95% CI: 1.98-26.32) made hospitalisation more likely, with vascular access complications occurring in 3%. At 30 days, the hospital readmission rate was low in both SDD and non-SDD patients (5% vs 7%; p=non-significant). Finally, SDD was not a predictor for major adverse cardiovascular events (MACE) at follow-up.
CONCLUSIONS: Same-day discharge can be achieved in the majority of patients undergoing CTO PCI with large-bore (≥7 Fr) access. Similar low hospital readmission and MACE rates between SDD and non-SDD patients at 30 days demonstrate the feasibility and safety of SDD.
Overnight observation is frequently applied in patients undergoing elective percutaneous coronary intervention (PCI) of a chronic total coronary occlusion (CTO)1. In the Prospective Global Registry for the Study of Chronic Total Occlusion Intervention (PROGRESS-CTO), one of the largest cohorts to date, the overall rate of same-day discharge (SDD) is ~13%2. SDD in CTO PCI is tantalising because of its increased patient comfort and economic advantage13. The feasibility and safety of SDD after PCI in patients with stable angina has been demonstrated in observational studies and randomised trials, yet data on its application in patients undergoing CTO PCI are scarce1. The use of large-bore (≥7 French [Fr]) arterial access in CTO PCI could hamper SDD, due to its association with vascular access complications4. Conversely, reducing the guiding catheter size may drive higher rates of SDD2. Nevertheless, the hybrid algorithm recommends the use of a large-bore guiding catheter, as increasing the Fr size augments therapeutic options by providing backup and space for the delivery of bulky material56. The trade-off between increased therapeutic options and higher complication rates in CTO PCI raises the question of whether SDD can be achieved when large-bore guiding catheters are used. In addition, identifying patients at risk for non-SDD may facilitate improved patient care. The present study sought to determine the feasibility and safety of SDD in CTO PCI after large-bore vascular access. Furthermore, we aimed to identify predictors for non-SDD following large-bore CTO PCI.
Methods
STUDY POPULATION
The present study prospectively recruited patients from a dedicated high-volume CTO PCI centre (Amsterdam UMC, Vrije Universiteit, the Netherlands). All patients who underwent CTO PCI between December 2013 and March 2023 were eligible for inclusion. Referral for revascularisation was performed by the Heart Team and based primarily on the presence of symptoms, ischaemia and/or viability testing. All patients were considered eligible for same-day discharge prior to PCI, which is in accordance with standard hospital care. The decision to postpone SDD was left to the attending physician. Study data were registered and managed using an electronic data capture system (Castor). All patients provided written informed consent.
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Angiographic and procedural characteristics were assessed by 2 expert CTO observers (S.P. Schumacher and Y.B.O. Somsen) using images acquired by a monoplane cardiovascular X-ray system (Allura Xper FD 10/10 [Philips]). Between 2013 and 2019, the definition of a CTO was a luminal occlusion of a coronary artery with an estimated or documented duration of ≥3 months and no or minimal contrast penetration through the lesion (Thrombolysis In Myocardial Infarction [TIMI] flow grade 0-1)7. From 2020 onwards, the updated definition of the CTO Academic Research Consortium was applied, which described a CTO as an absence of antegrade flow through the CTO lesion with a presumed or documented duration of ≥3 months8. The complexity of the CTO vessel was evaluated using the Japanese CTO (J-CTO) score9. Collateral morphology was described using the Rentrop classification and Werner grade1011. CTO PCI was performed by 2 dedicated operators (A. Nap and P. Knaapen) in accordance with the hybrid algorithm5. Technical success was defined as TIMI flow grade 3 and <30% residual diameter stenosis12. Procedural success was defined as technical success and an absence of in-hospital major adverse cardiovascular events (MACE). In-hospital MACE included the following events: all-cause death, non-fatal myocardial infarction (MI), emergency revascularisation of the target vessel with PCI or coronary artery bypass grafting (CABG) surgery, tamponade requiring pericardiocentesis or surgery, and stroke. Periprocedural MI was defined according to the Fourth Universal Definition of Myocardial Infarction13. Cardiac biomarkers were collected if periprocedural MI was suspected.
VASCULAR ACCESS CHARACTERISTICS
The standard CTO PCI vascular setup involved a transradial (7 Fr) and transfemoral (8 Fr) vascular access approach. Any deviation from the standard vascular setup was at the operator’s discretion and included the following access sites and/or setups: single, biradial, bifemoral, and triple access. All access sites underwent sterile preparation and subcutaneous injection of lidocaine, followed by arterial puncture using the (modified) Seldinger technique and introduction of a 5, 6, 7 or 8 Fr sheath into the primary and secondary access sites. The terms primary and secondary refer to the sequence of arterial puncture by the operator. Fluoroscopic or ultrasound guidance was utilised at the discretion of the operator. All patients received a concoction of verapamil and nitroglycerine after insertion of the radial sheath(s), followed by unfractionated heparin (70-100 IU/kg) prior to insertion of the guiding catheters. The radial and femoral sheaths were immediately removed upon completion of the procedure, unless the operator decided otherwise. Haemostasis was achieved by the application of manual compression or 1 or more of the following vascular closure devices (VCD): TR Band (Terumo), Angio-Seal (Terumo), Perclose ProGlide Suture-Mediated Closure System (Abbott), and FemoStop (Abbott). In patients with a femoral puncture, horizontal bed rest was mandatory for a minimum of 2 hours following PCI. All patients were hospitalised for a minimum of 4.5 hours following CTO PCI to ensure adequate access site monitoring (such as gradual TR Band deflation and mobilisation after femoral access), as per standard practice in this centre.
ENDPOINTS AND CLINICAL FOLLOW-UP
The primary endpoint of this study was successful SDD, defined as no overnight hospital stay following CTO PCI. Secondary endpoints included clinically relevant access site-related bleeding, vascular access site complications, and the occurrence of MACE during hospitalisation and at 30-day follow-up. Events recorded at 30-day follow-up in the non-SDD group did not include the primary event causing hospitalisation. Access site-related bleeding was defined according to the Bleeding Academic Research Consortium (BARC) criteria and perceived to be clinically relevant when it required medical intervention by a healthcare professional, such as hospitalisation, evaluation or increased level of care (BARC ≥2)14. Vascular access site complications included the occurrence of vascular damage as defined by 1 or more of the following parameters: acute arterial thrombosis, arteriovenous fistula, arterial dissection, pseudoaneurysm, arterial perforation, and retroperitoneal haematoma. Clinical follow-up was obtained through electronic patient files and telephone contact following CTO PCI.
STATISTICAL ANALYSIS
Continuous variables are presented as mean±standard deviation for normally distributed data, and as median (interquartile range) for non-normally distributed data. Categorical variables are noted as frequencies with percentages. Baseline characteristics are stratified to SDD and non-SDD patients; normally distributed data were analysed using the independent t-test, and non-normally distributed data were compared using the Mann-Whitney U test. Fisher’s exact test or the Chi-square test were used to compare categorical data, accordingly. First, to identify predictors for the occurrence of non-SDD, several univariable logistic regression analyses were performed. The following variables were selected on clinical relevance and separately entered into the model: age, female sex, body mass index, hypertension, hypercholesterolaemia, history of smoking, diabetes mellitus type II, renal insufficiency, peripheral artery disease, dual antiplatelet therapy use, prior MI, prior PCI, prior CABG, CTO target vessel, calcification, bending >45 degrees, occlusion length ≥20 mm, re-try lesion, J-CTO score, single access, technical success, local access site bleeding, and vascular access complications. Dummy variables were created for categorical data, wherein the first category of each variable type was used as a reference. Second, a multivariable logistic regression analysis was performed including all variables with a univariable p-value of <0.10. Finally, we performed 3 univariable logistic regression analyses to analyse whether SDD predicted hospital readmission, MACE and vascular access complications at 30-day follow-up. A p-value of <0.05 was considered statistically significant. Statistical analysis was carried out using SPSS software (IBM).
Results
STUDY POPULATION
Between December 2013 and March 2023, a total of 1,052 patients were considered for CTO PCI after initial detection of a CTO on invasive coronary angiography (Figure 1). Of the included 948 patients, SDD was observed in 62%. Baseline characteristics are listed in Table 1. SDD patients were younger and more often male. In addition, renal insufficiency, prior MI and prior CABG were associated with non-SDD. Finally, medication use was comparable between the groups.
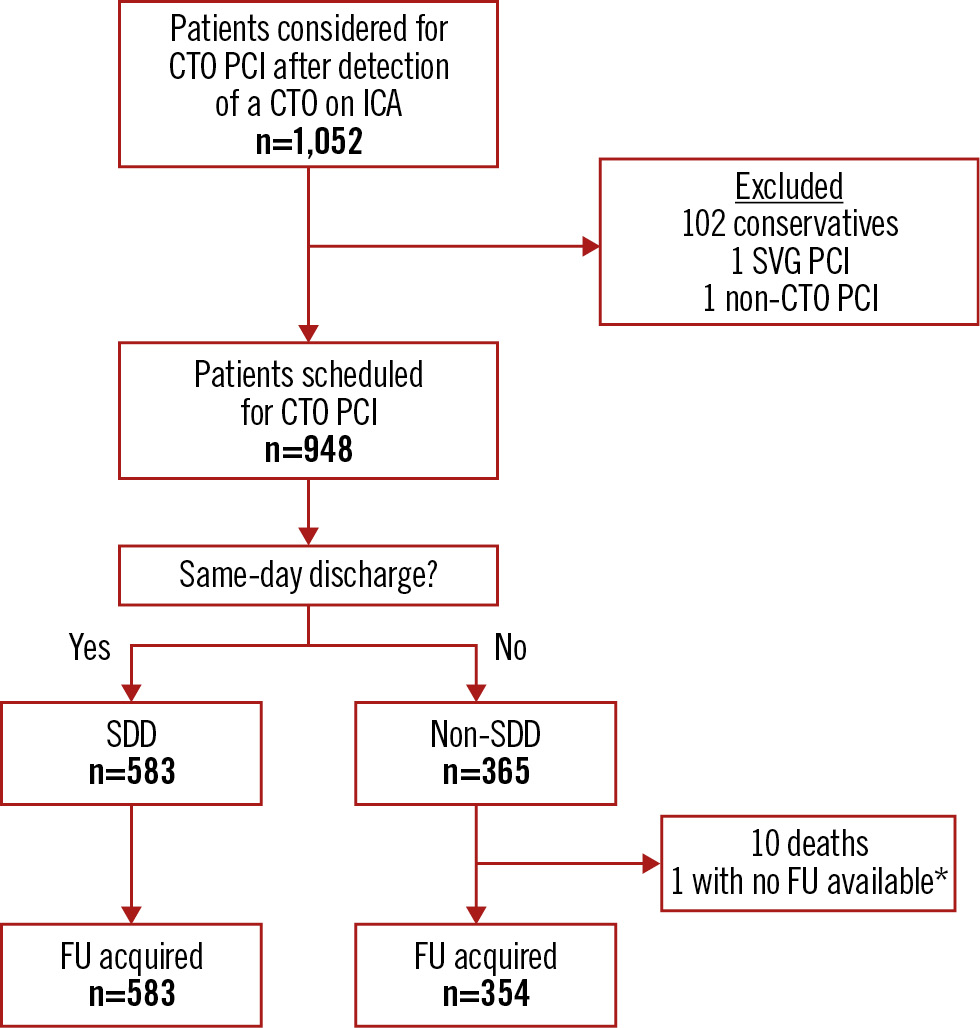
Figure 1. Flowchart of the study population. *Patient was transferred to a different hospital and lost to FU. CTO: chronic coronary total occlusion; FU: follow-up; ICA: invasive coronary angiography; PCI: percutaneous coronary intervention; SDD: same-day discharge; SVG: saphenous vein graft
Table 1. Baseline characteristics.
| Total cohort (n=948) | SDD (n=583) |
Non-SDD (n=365) | p-value* | |
|---|---|---|---|---|
| Demographics | ||||
| Age, years | 66±11 | 65±10 | 68±11 | <0.01 |
| BMI, kg/m2 | 28±7 | 28±4 | 28±10 | 0.76 |
| Male | 775 (82) | 495 (85) | 280 (77) | <0.01 |
| LVEF, % | 0.01 | |||
| Normal, >55 | 395 (43) | 267 (47) | 128 (36) | - |
| Mild, 45-55 | 278 (30) | 163 (29) | 115 (33) | - |
| Moderate, 30-45 | 164 (18) | 93 (16) | 71 (20) | - |
| Severe, <30 | 82 (9) | 42 (7) | 40 (11) | - |
| Cardiovascular risk factors | ||||
| Hypertension | 548 (59) | 321 (56) | 227 (63) | 0.05 |
| Hypercholesterolaemia | 477 (51) | 283 (50) | 194 (53) | 0.24 |
| Diabetes mellitus type II | 260 (28) | 153 (26) | 107 (29) | 0.31 |
| History of smoking | 519 (58) | 343 (62) | 175 (51) | <0.01 |
| Renal insufficiency | 158 (17) | 70 (12) | 88 (24) | <0.01 |
| eGFR, mL/min/1.73 m2 | 73±20 | 76±19 | 67±20 | <0.01 |
| Peripheral artery disease | 157 (17) | 88 (15) | 69 (19) | 0.15 |
| Cardiac history | ||||
| Prior MI | 495 (52) | 275 (47) | 220 (60) | <0.01 |
| Prior PCI | 344 (58) | 341 (59) | 227 (62) | 0.25 |
| Prior CABG | 216 (23) | 100 (17) | 116 (32) | <0.01 |
| Cardiac medication | ||||
| Salicylates | 795 (84) | 498 (85) | 297 (81) | 0.10 |
| Dual antiplatelet therapy | 525 (55) | 311 (53) | 214 (59) | 0.11 |
| Oral anticoagulation | 132 (14) | 79 (14) | 53 (15) | 0.68 |
| DOAC† | 34 (13) | 20 (13) | 14 (13) | 0.84 |
| Proton pump inhibitor† | 179 (68) | 103 (64) | 76 (72) | 0.17 |
| ACE inhibitor† | 98 (37) | 54 (34) | 44 (42) | 0.18 |
| ß-blocker | 731 (77) | 448 (77) | 283 (78) | 0.81 |
| Calcium channel blocker | 264 (28) | 156 (27) | 108 (30) | 0.34 |
| Long-acting nitrate | 314 (33) | 177 (30) | 137 (38) | 0.02 |
| Statin | 788 (83) | 478 (82) | 310 (85) | 0.24 |
| Clinical presentation‡ | ||||
| Anginal pain | 483 (62) | 314 (62) | 169 (62) | 0.99 |
| Dyspnoea on exertion | 336 (43) | 222 (44) | 114 (42) | 0.67 |
| Values are presented as mean±SD or n (%). *Statistical testing was performed between the SDD and non-SDD cohort. †The use of DOAC, proton pump inhibitors, and/or ACE inhibitor was documented in 28% of cases. ‡Clinical presentation was documented in 82% of cases. ACE: angiotensin-converting enzyme; BMI: body mass index; CABG: coronary artery bypass grafting; DOAC: direct oral anticoagulants; eGFR: estimated glomerular filtration rate; LVEF: left ventricular ejection fraction; MI: myocardial infarction; PCI: percutaneous coronary intervention; SD: standard deviation; SDD: same-day discharge | ||||
ANGIOGRAPHIC AND PROCEDURAL CHARACTERISTICS
Angiographic characteristics are detailed in Table 2. SDD was less often pursued with increased CTO lesion complexity, as reflected by higher rates of blunt cap, calcification, bending >45 degrees, occlusion length ≥20 mm, and a complex J-CTO score (≥3) in non-SDD patients. The procedural characteristics are presented in Table 3. Dual arterial access was used in the majority of patients in both groups (90% in SDD vs 94% in non-SDD; p=0.05). The most common vascular access setup in the total cohort was a radial-femoral approach. Large-bore access was used in 936 (99%) patients. Failure to achieve technical CTO PCI success was associated with non-SDD (5% in SDD vs 13% in non-SDD; p<0.01). Similarly, failure to achieve procedural success preceded non-SDD (5% in SDD vs 23% in non-SDD; p<0.01). Lastly, a shorter total procedure time, shorter fluoroscopy time, and lower total contrast volume were all associated with SDD.
Table 2. Angiographic characteristics.
| Total cohort (n=948) | SDD (n=583) |
Non-SDD (n=365) | p-value* | |
|---|---|---|---|---|
| CTO target vessel | 0.78 | |||
| RCA | 573 (60) | 348 (60) | 225 (62) | - |
| LAD | 237 (25) | 145 (25) | 92 (25) | - |
| LCx | 133 (14) | 87 (15) | 46 (13) | - |
| LM | 5 (<1) | 3 (<1) | 2 (<1) | - |
| Number of diseased vessels | 1.00 | |||
| 1 | 594 (63) | 365 (63) | 229 (63) | - |
| 2 | 253 (27) | 156 (27) | 97 (27) | - |
| 3 | 101 (11) | 62 (11) | 39 (11) | - |
| CTO lesion characteristics | ||||
| Blunt cap | 297 (34) | 169 (32) | 128 (39) | 0.03 |
| Calcification | 558 (59) | 322 (55) | 236 (65) | <0.01 |
| Bending >45 degrees | 370 (39) | 201 (35) | 169 (47) | <0.01 |
| Occlusion length ≥20 mm | 455 (48) | 251 (43) | 204 (56) | <0.01 |
| Re-try lesion | 121 (13) | 76 (13) | 45 (12) | 0.77 |
| Rentrop classification† | 0.61 | |||
| 0-1 | 14 (3) | 8 (2) | 6 (3) | - |
| 2 | 83 (16) | 57 (17) | 26 (15) | - |
| 3 | 410 (81) | 263 (80) | 147 (82) | - |
| Werner grade | 0.69 | |||
| 0 | 15 (2) | 10 (2) | 5 (2) | - |
| 1 | 298 (34) | 190 (35) | 108 (34) | - |
| 2 | 538 (62) | 338 (62) | 200 (62) | - |
| J-CTO score | <0.01 | |||
| 0-1 | 347 (37) | 241 (42) | 106 (29) | - |
| 2 | 278 (30) | 185 (32) | 93 (26) | - |
| ≥3 | 318 (34) | 155 (27) | 163 (45) | - |
| Values are presented as n (%). *Statistical testing was performed between the SDD and non-SDD cohort. †Rentrop classification was documented in 54% of cases. CTO: chronic total coronary occlusion; J-CTO: Japanese chronic total occlusion; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; RCA: right coronary artery; SDD: same-day discharge | ||||
Table 3. Procedural characteristics.
| Total cohort (n=948) | SDD (n=583) |
Non-SDD (n=365) | p-value* | |
|---|---|---|---|---|
| Total no. of vessels treated by PCI† | <0.01 | |||
| 1 | 605 (69) | 387 (73) | 218 (64) | - |
| 2 | 184 (21) | 114 (21) | 70 (21) | - |
| 3 | 49 (6) | 18 (3) | 31 (9) | - |
| Setup | <0.01 | |||
| Radial-Femoral | 663 (77) | 419 (80) | 244 (71) | - |
| Femoral-Femoral | 192 (22) | 98 (19) | 94 (28) | - |
| Radial-Radial | 8 (<1) | 4 (<1) | 4 (1) | - |
| Access | ||||
| Dual access | 876 (92) | 525 (90) | 342 (94) | 0.05 |
| Triple access | 9 (<1) | 2 (<2) | 7 (2) | 0.03 |
| Primary access site | <0.01 | |||
| RFA | 5 (<1) | 1 (<1) | 4 (1) | - |
| LFA | 187 (21) | 97 (18) | 90 (26) | - |
| RRA | 674 (74) | 434 (78) | 240 (68) | - |
| LRA | 30 (3) | 15 (3) | 15 (4) | - |
| Transradial or transfemoral use | <0.01 | |||
| Transradial use | 704 (79) | 449 (82) | 255 (73) | - |
| Transfemoral use | 192 (21) | 98 (18) | 94 (27) | - |
| Secondary access site | 0.12 | |||
| RFA | 860 (93) | 531 (93) | 329 (91) | - |
| LFA | 47 (5) | 22 (4) | 25 (7) | - |
| RRA | 8 (<1) | 4 (<1) | 4 (1) | - |
| LRA | 0 | 0 | 0 | - |
| Transradial or transfemoral use | 0.53 | |||
| Transradial use | 8 (<1) | 4 (<1) | 4 (1) | - |
| Transfemoral use | 907 (99) | 553 (93) | 354 (99) | - |
| Guiding catheter size | ||||
| No large-bore access used | 12 (1) | 11 (2) | 1 (<1) | 0.04 |
| Primary access site | 0.47 | |||
| 5 Fr | 1 (<1) | 1 (<1) | 0 | - |
| 6 Fr | 98 (11) | 58 (11) | 40 (11) | - |
| ≥7 Fr | 801 (88) | 492 (88) | 309 (88) | - |
| Secondary access site | 0.27 | |||
| 6 Fr | 13 (1) | 10 (2) | 3 (<1) | - |
| ≥7 Fr | 902 (97) | 547 (96) | 355 (98) | - |
| Vascular closure used‡ | ||||
| Manual pressure | 11 (1) | 4 (<1) | 7 (2) | 0.12 |
| TR Band | 538 (57) | 341 (59) | 197 (54) | 0.17 |
| Angio-Seal | 665 (70) | 414 (71) | 251 (69) | 0.46 |
| Perclose ProGlide | 38 (4) | 20 (3) | 18 (5) | 0.31 |
| FemoStop | 1 | 1 (<1) | 0 | 1.00 |
| Final successful CTO crossing strategy | <0.01 | |||
| AWE | 432 (48) | 317 (56) | 115 (34) | - |
| ADR | 174 (19) | 92 (16) | 82 (24) | - |
| RWE | 95 (11) | 57 (10) | 38 (11) | - |
| RDR | 207 (23) | 103 (18) | 104 (31) | - |
| Technical outcomes§ | ||||
| Technical success | 872 (92) | 554 (95) | 318 (87) | <0.01 |
| Procedural success | 831 (88) | 552 (95) | 279 (77) | <0.01 |
| Wire crossing time, min | 30 [8-66] | 20 [5-49] | 50 [13-90] | <0.01 |
| Total procedure time, min | 113±55 | 99±49 | 137±55 | <0.01 |
| Total fluoroscopy time, min | 46±34 | 38±27 | 59±39 | <0.01 |
| Total contrast volume, ml | 279±146 | 258±132 | 316±161 | <0.01 |
| Values are presented as mean±SD, median [IQR] or n (%). *Statistical testing was performed between the SDD and non-SDD cohort. †The number of treated vessels was documented in 89% of cases. ‡The percentages represent the percentage of patients receiving ≥1 VCD. VCD use was documented in 79% (for primary access site) and 69% (for secondary access site) of cases. §Total procedure time, fluoroscopy time and contrast volume were available in 83%, 75%, and 68% of cases. ADR: antegrade dissection and re-entry; AWE: antegrade wire escalation; CTO: chronic total coronary occlusion; Fr: French; IQR: interquartile range; LFA: left femoral artery; LRA: left radial artery; PCI: percutaneous coronary intervention; RDR: retrograde dissection and re-entry; RFA: right femoral artery; RRA: right radial artery; RWE: retrograde wire escalation; SD: standard deviation; SDD: same-day discharge; VCD: vascular closure device | ||||
IN-HOSPITAL EVENTS AND CLINICAL FOLLOW-UP
In-hospital events are listed in Table 4. Perforation and periprocedural MI often preceded hospitalisation. Equally, emergency revascularisation, tamponade, and contrast-induced nephropathy (CIN) were associated with a failure to achieve SDD. In the non-SDD group, local access site bleeding and retroperitoneal haematoma represented the largest proportion of bleeding and vascular access complications. Figure 2 shows the primary causes for non-SDD. Hypotension, side-branch occlusion and persisting chest pain combined (classified as other causes) were most often reported as the primary cause for hospital admission (30%), followed by bleeding (22%) and MACE (16%). Vascular access complications represented 5% of the primary causes for non-SDD. A comparison between short (≤48 hours) and long (>48 hours) hospital admission can be found in Supplementary Table 1.
Figure 3 depicts the hospital readmission rates and causes for readmission at 30-day follow-up in SDD and non-SDD patients. Follow-up was available for 100% of SDD patients and for 97% of non-SDD patients. The hospital readmission rate at 30 days was overall low and not statistically different between the 2 cohorts. In both groups, a minority of patients were admitted within 24 hours following CTO PCI. MACE and vascular access complication rates at 30-day follow-up were low for the total cohort (2% and 1%, respectively) (Supplementary Table 2). Finally, temporal trends in the rates of SDD, MACE, and the most common in-hospital events (perforation and local access site bleeding) are depicted in Figure 4. A high SDD rate and low MACE rate were observed over the entire study period, whereas there was a trend towards lower perforation rates and a significant increase in local access site bleeding.
Table 4. In-hospital events.
| Total cohort (n=948) | SDD (n=583) |
Non-SDD (n=365) | p-value* | |
|---|---|---|---|---|
| In-hospital events | ||||
| Perforation | 114 (12) | 22 (4) | 92 (25) | <0.01 |
| MACE | 83 (9) | 5 (<1) | 83 (23) | <0.01 |
| Mortality | 10 (1) | 0 | 10 (3) | <0.01 |
| Periprocedural MI | 58 (6) | 3 (<1) | 55 (15) | <0.01 |
| Emergency revascularisation | ||||
| PCI | 6 (<1) | 0 | 6 (2) | <0.01 |
| CABG | 0 | - | - | - |
| Tamponade requiring treatment | 29 (3) | 0 | 28 (8) | <0.01 |
| Stroke | 5 (<1) | 0 | 4 (1) | 0.01 |
| CIN | 11 (1) | 2 (<1) | 9 (3) | <0.01 |
| Bleeding | ||||
| Local access site | 131 (14) | 25 (4) | 106 (29) | <0.01 |
| Retroperitoneal | 9 (<1) | 0 | 9 (3) | <0.01 |
| Gastrointestinal | 2 (<1) | 0 | 2 (<1) | 0.15 |
| Intracerebral | 0 | - | - | - |
| Vascular access complication | ||||
| Complication occurred | 25 (3) | 3 (<1) | 22 (6) | <0.01 |
| Dissection | 4 (<1) | 1 (<1) | 3 (<1) | 0.16 |
| AV fistula | 1 (<1) | 0 | 1 (<1) | 0.39 |
| Thrombosis | 1 (<1) | 1 (<1) | 0 | 1.00 |
| Pseudoaneurysm | 9 (<1) | 1 (<1) | 8 (2) | <0.01 |
| Retroperitoneal haematoma | 9 (<1) | 0 | 9 (3) | <0.01 |
| Perforation | 2 (<1) | 0 | 2 (<1) | 0.15 |
| Other† | 1 (<1) | 0 | 1 (<1) | 0.39 |
| Values are presented as n (%). *Statistical testing was performed between the SDD and non-SDD cohort. †Pertains to one case wherein the guiding catheter had to be surgically extracted due to extreme tortuosity in the brachial artery. AV: arteriovenous; CABG: coronary artery bypass grafting; CIN: contrast-induced nephropathy; MACE: major adverse cardiovascular events; MI: myocardial infarction; PCI: percutaneous coronary intervention; SDD: same-day discharge | ||||
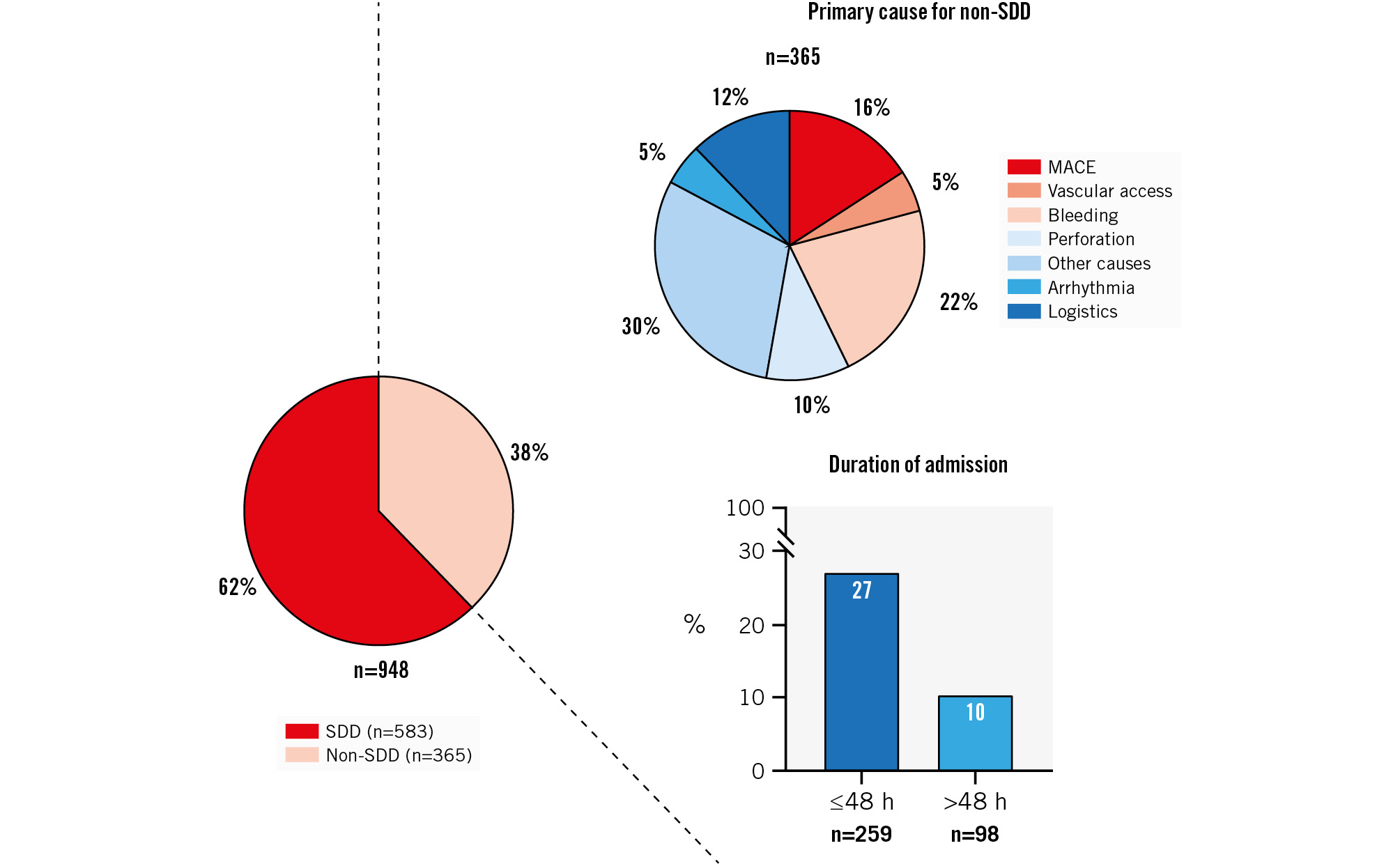
Figure 2. Primary causes for non-SDD. The pie charts depict the primary causes for non-SDD and the incidence of SDD and non-SDD, and the bar graph shows the duration of hospital admission. Non-SDD occurred in 38%. Other causes (a composite of clinically relevant hypotension, side-branch occlusion and persisting chest pain) was the most common primary cause for non-SDD. Notably, vascular access complications represented a minority of all causes. The majority of non-SDD patients were admitted for ≤48 hours following CTO PCI. N.B. The primary cause for non-SDD could not be determined in 2 patients. In 4% of patients admitted for major adverse cardiovascular events (MACE), the event had occurred prior to CTO PCI. The duration of hospital admission was not available in 8 patients (6 periprocedural deaths, 2 transferred to a different hospital). CTO: chronic total coronary occlusion; PCI: percutaneous coronary intervention; SDD: same-day discharge
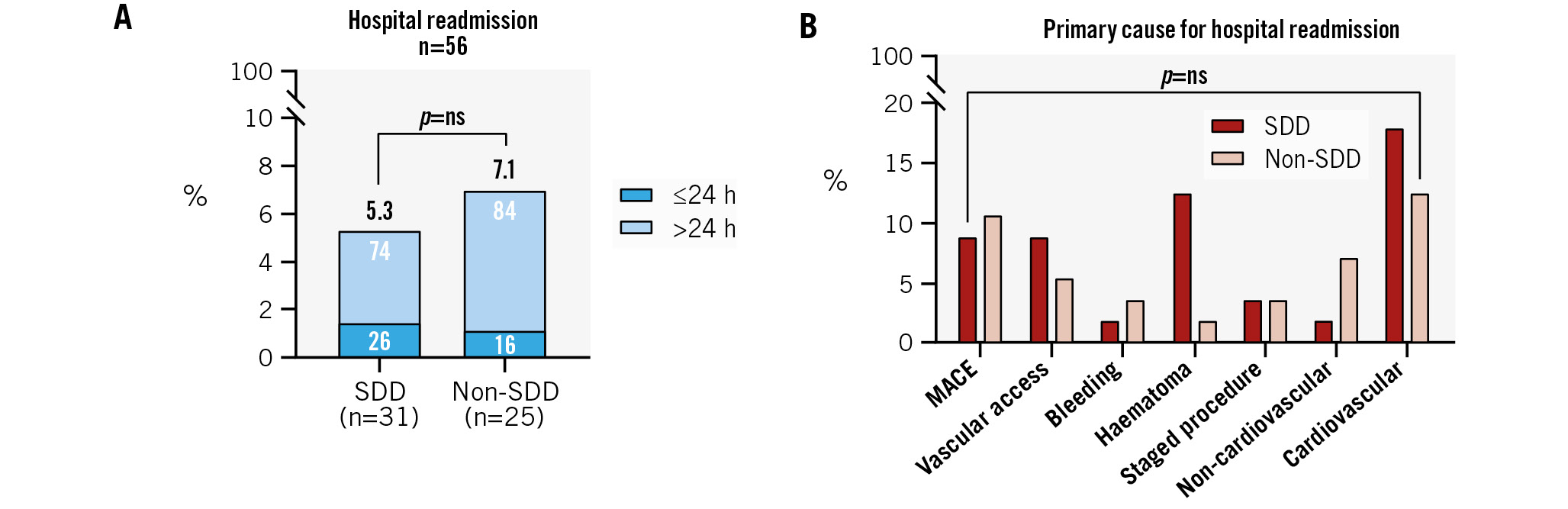
Figure 3. Hospital readmission at 30-day follow-up. A) Hospital readmission rates were low and comparable between SDD and non-SDD patients (5.3% vs 7.1%; p=ns). In both groups, the majority of patients were admitted after 24 hours. B) Cardiovascular causes were the most frequently listed primary cause for hospital readmission in both groups, followed by MACE. Cardiovascular causes for readmission included arrhythmias, recurrent cardiac symptoms, and (acute) heart failure. A staged procedure could either be an invasive coronary angiography or PCI. MACE: major adverse cardiovascular events; ns: non-significant; PCI: percutaneous coronary intervention; SDD: same-day discharge
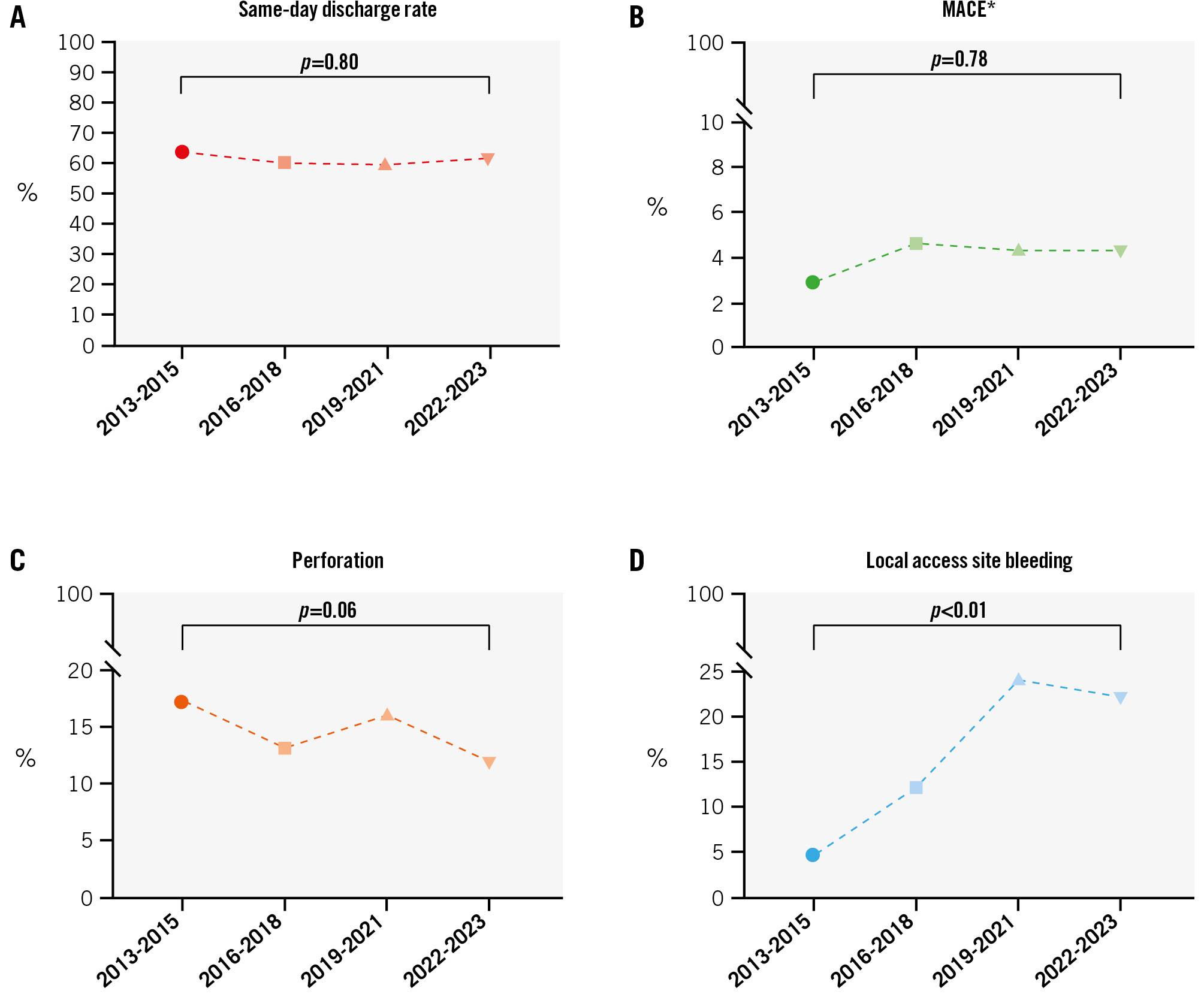
Figure 4. Temporal trends in SDD and in-hospital complications. A) SDD rate, in-hospital MACE (B), perforation (C), and local access site bleeding (D). Notably, SDD was achieved in the majority of patients and remained constant over the total study period, regardless of the increasing rates of local access site bleeding. Equally, the MACE rate was low and constant. Finally, there appears to be a trend towards lower perforation rates over the inclusion period, yet, this was not statistically significant. *MACE is represented without periprocedural MI. MACE: major adverse cardiovascular events; MI: myocardial infarction; SDD: same-day discharge
IDENTIFICATION OF PREDICTORS FOR NON-SDD
Multivariable regression analysis led to the identification of predictors for non-SDD (Table 5). Predictors for hospitalisation included the presence of renal insufficiency (odds ratio [OR] 1.84, 95% confidence interval [CI]: 1.23-2.75), prior MI (OR 1.68, 95% CI: 1.24-2.29), and prior CABG (OR 1.66, 95% CI: 1.15-2.41). Female sex (OR 0.64, 95% CI: 0.44-0.95) and technical CTO PCI success (OR 0.44, 95% CI: 0.25-0.78) were both associated with same-day discharge. Furthermore, hospitalisation was more likely when local access site bleeding (OR 8.53, 95% CI: 5.24-13.87) or vascular access complications (OR 7.23, 95% CI: 1.98-26.32) occurred. Finally, SDD was not found to be a significant predictor for hospital readmission, MACE, or vascular access complications at 30-day clinical follow-up (Table 6).
Table 5. Predictors for non-SDD following CTO PCI.
| Univariable analysis | Multivariable analysis | |||
|---|---|---|---|---|
| OR (95% CI) | p-value* | OR (95% CI) | p-value* | |
| Demographics | ||||
| Age | 1.03 (1.02-1.05) | <0.01 | 1.01 (0.97-1.03) | 0.14 |
| Female sex | 0.59 (0.42-0.82) | <0.01 | 0.64 (0.44-0.95) | 0.03 |
| BMI | 1.00 (0.98-1.02) | 0.76 | - | - |
| Cardiovascular risk factors | ||||
| Hypertension | 1.32 (1.01-1.72) | 0.05 | 1.14 (0.83-1.55) | 0.41 |
| Hypercholesterolaemia | 1.17 (0.90-1.53) | 0.24 | - | - |
| History of smoking | 1.00 (0.99-1.01) | 0.57 | - | - |
| Diabetes mellitus type II | 1.16 (0.87-1.56) | 0.31 | - | - |
| Renal insufficiency | 2.32 (1.64-3.27) | <0.01 | 1.84 (1.23-2.75) | <0.01 |
| Peripheral artery disease | 1.29 (0.91-1.83) | 0.15 | - | - |
| Dual antiplatelet therapy | 1.24 (0.95-1.62) | 0.11 | - | - |
| Cardiac history | ||||
| Prior MI | 1.69 (1.30-2.21) | <0.01 | 1.68 (1.24-2.29) | <0.01 |
| Prior PCI | 1.17 (0.90-1.53) | 0.25 | - | - |
| Prior CABG | 2.26 (1.66-3.07) | <0.01 | 1.66 (1.15-2.41) | <0.01 |
| Angiographic outcomes | ||||
| CTO target vessel | ||||
| LAD | 1.02 (0.75-1.34) | 0.91 | - | - |
| LCx | 0.82 (0.56-1.21) | 0.32 | - | - |
| LM | 1.07 (1.18-6.41) | 0.95 | - | - |
| Calcification | 1.50 (1.14-1.96) | <0.01 | 0.84 (0.56-1.27) | 0.42 |
| Bending >45 degrees | 1.66 (1.27-2.16) | <0.01 | 1.20 (0.79-1.81) | 0.40 |
| Occlusion length ≥20 mm | 1.68 (1.29-2.19) | <0.01 | 0.99 (0.65-1.52) | 0.97 |
| Re-try lesion | 0.94 (0.64-1.40) | 0.77 | - | - |
| J-CTO score | 1.33 (1.19-1.49) | <0.01 | 1.19 (0.93-1.53) | 0.18 |
| Procedural outcomes | ||||
| Single access | 0.61 (0.37-1.01) | 0.05 | 0.84 (0.48-1.50) | 0.56 |
| Technical success | 0.35 (0.22-0.57) | <0.01 | 0.44 (0.25-0.78) | <0.01 |
| In-hospital events | ||||
| Local access site bleeding | 9.14 (5.77-14.47) | <0.01 | 8.53 (5.24-13.87) | <0.01 |
| Vascular access complication | 12.40 (3.68-41.74) | <0.01 | 7.23 (1.98-26.32) | <0.01 |
| *The p-value threshold was set at 0.10 in the univariable analyses and at 0.05 in the multivariable analyses. BMI: body mass index; CABG: coronary artery bypass grafting; CI: confidence interval; CTO: chronic total coronary occlusion; J-CTO: Japanese CTO; LAD: left anterior descending artery; LCx: left circumflex artery; LM: left main; MI: myocardial infarction; OR: odds ratio; PCI: percutaneous coronary intervention; SDD: same-day discharge | ||||
Table 6. Predictive value of SDD for hospital readmission and clinical events at 30-day follow-up.
| Univariable analysis* | ||
|---|---|---|
| OR (95% CI) | p-value | |
| Hospital readmission | ||
| SDD | 0.74 (0.43-1.27) | 0.28 |
| MACE | ||
| SDD | 0.60 (0.21-1.73) | 0.35 |
| Vascular access complications | ||
| SDD | 1.22 (0.30-4.90) | 0.78 |
| *In 11 patients, 30-day follow-up could not be acquired because of death during hospitalisation (n=10) and transfer to a different hospital (n=1). CI: confidence interval; MACE: major adverse cardiovascular events; OR: odds ratio; SDD: same-day discharge | ||
Discussion
The present study sought to investigate the feasibility and safety of same-day discharge in CTO PCI following large-bore vascular access (Central illustration). First, all patients enrolled in this study were considered eligible for SDD prior to revascularisation. SDD was achieved in the majority of patients (62%) along with a low vascular access complication rate, irrespective of the high rate of large-bore (≥7 Fr) guiding catheter use (99%). Patients with local access site bleeding and vascular access complications were more often held for overnight observation. Second, clinical follow-up at 30 days showed low overall vascular access complication and MACE rates which were not statistically different between patients with and without SDD. Finally, the presence of renal insufficiency, prior MI, prior CABG, and in-hospital complications made hospitalisation more likely.
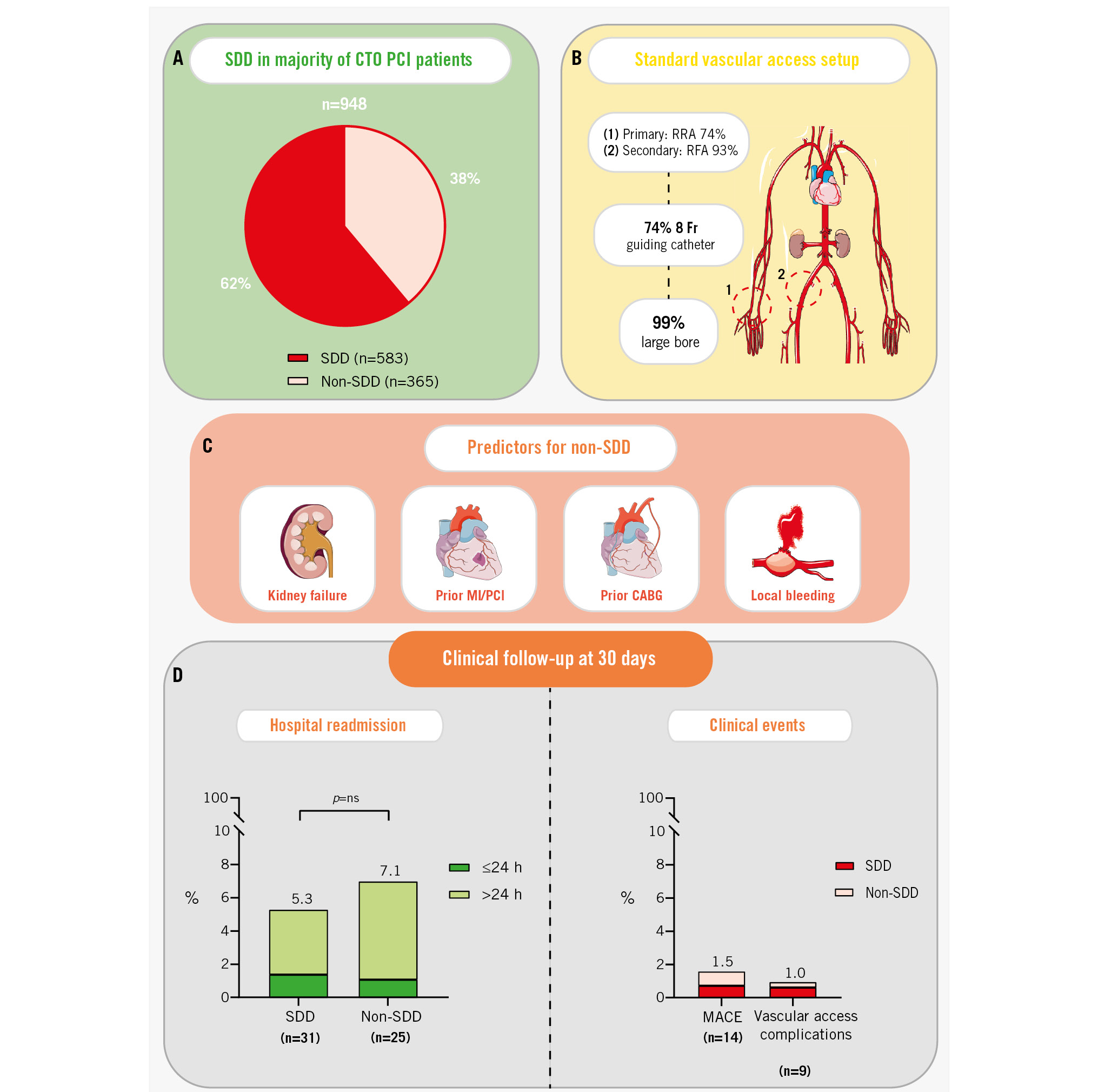
Central illustration. Same-day discharge after large-bore access in percutaneous coronary intervention of chronic total coronary occlusions. A) This study comprised 948 patients who were prospectively enrolled in a single CTO centre and underwent CTO PCI. The majority of patients (62%) underwent same-day discharge (SDD). B) In the total cohort, the most common vascular access sites were the RRA (74%) and RFA (93%). The application of large-bore (≥7 Fr) guiding catheters was highly prevalent. C) Predictors for non-SDD included the presence of renal insufficiency, prior MI or PCI, prior CABG, and local access site bleeding. D) At 30-day follow-up, the overall readmission rate was low and statistically comparable between patients with and without SDD. Finally, the MACE rate and vascular access complication rates were low and statistically equal. The (n=) represents the number of readmissions/clinical events within each group. CABG: coronary artery bypass grafting; CTO: chronic total coronary occlusion; MACE: major adverse cardiovascular events; MI: myocardial infarction; ns: non-significant; PCI: percutaneous coronary intervention; RFA: right femoral artery; RRA: right radial artery; SDD: same-day discharge
SAME-DAY DISCHARGE IN CTO PCI
Same-day discharge following complex PCI has received limited attention, and most available data stem from observational studies. Koutouzis et al suggested that SDD could be achieved in selected patients undergoing elective complex PCI when a forearm approach was used. In the 28 (17%) patients who were discharged the same day, there were no reported complications at 30-day follow-up15. A more recent study by the same research group in 173 patients showed an increase in the rate of SDD (to 30%), with low MACE and mortality rates at 30-day follow-up3. Sawant and colleagues demonstrated an SDD rate of 42% in 144 consecutive CTO PCI patients, wherein the MACE rate at 30-day follow-up was low and comparable between patients with and without SDD (1.7% vs 2.4%; p=non-significant). In the same study, several predictors for non-SDD were identified, including older age and the presence of complications16. Interestingly, a third observational study by Taxiarchi et al reported that the rate of SDD in elective CTO PCI increased over time. The data, acquired from the British Cardiovascular Intervention Society registry, showed SDD practice in CTO PCI increased from 22% (2007) to 45% (2014). In addition, the transradial approach was strongly and independently associated with SDD1. While these observational studies all appear favourable towards SDD following CTO PCI, few provide insight into the application of large-bore guiding catheters. A meta-analysis by Meijers et al listed an overview of all CTO PCI studies on vascular access over the last 15 years. In the majority of these trials, guiding catheter sizes were either below 7 Fr or not specified17. This meta-analysis did not included the study by Simsek et al, who reported an SDD rate of 13% in the PROGRESS-CTO. The authors found that utilisation of an 8 Fr sheath size was significantly less prevalent in patients with versus without SDD (8.3% vs 23.0%; p<0.01); however, data on guiding catheter size were only available for 33% of the total cohort2. To the best of our knowledge, our study is the first to demonstrate high rates of SDD (62%) combined with a high percentage of large-bore arterial access in at least 1 access site (99% of the total cohort). As previous studies report relatively lower rates of SDD combined with a low percentage of 8 Fr sheath size use, our data add to the current body of evidence that SDD can be pursued in a more complex patient population. Predictors for non-SDD found in our study, which include renal insufficiency, prior CABG, and the occurrence of in-hospital complications, have been reported in prior literature. Of all the primary causes listed for non-SDD, bleeding and vascular access complications represented 22% and 5%, respectively. Clinical follow-up at 30 days showed low and similar hospital readmission and MACE rates in patients with and without SDD. Our results suggest that SDD is feasible and safe following large-bore guiding catheters in CTO PCI and that SDD could be pursued in all patients scheduled for CTO PCI. Additionally, the identified predictors for non-SDD may better prepare the patient and physician for an increased likelihood of a prolonged hospital stay.
SELECTION OF ARTERIAL ACCESS SITE IN CTO PCI
The utilisation of a radial access has gained increasing interest in CTO PCI. A recent meta-analysis of 10,590 patients by Megaly et al reported an association between radial access and a lower risk of major bleeding and vascular access site complications – albeit in observational studies only18. Nevertheless, large-bore transradial access might not be suitable for all patients, due to the presence of anatomical variants of the artery, radial artery occlusion, or a small-calibre artery17. Besides these possible limitations of a biradial access, the use of a femoral access is often justified as it facilitates the insertion of large-bore guiding catheters (8 Fr) that provide ample support in complex lesions. In the present study, a radial-femoral vascular access setup was most commonly used. Furthermore, 8 Fr guiding catheters were used in 74% of all study subjects. While a high technical success rate was achieved in our population (92%), it should be noted that the procedural success rate was significantly lower in the non-SDD group (95% vs 77%; p<0.01). We hypothesise that this was driven by a higher patient complexity in the non-SDD group, as reflected by their increased comorbidities and a higher prevalence of a complex J-CTO score (≥3). Furthermore, local access site bleeding was notably higher in the non-SDD group. While data on the location of the bleeding are lacking, it is likely that the majority of bleeds occur at the femoral access site. The Femoral or Radial Approach in the Treatment of Coronary Chronic Total Occlusion (FORT CTO) Trial also reported a lower overall bleeding rate in patients randomised to a radial-only approach, which could be attributed to the use of smaller guiding catheters19. A limitation of this trial is the lower lesion and patient complexity compared to contemporary registries, along with the lack of data on techniques that may improve the safety of a femoral approach (such as ultrasound). Emphasis on the reduction of complications in CTO PCI has fuelled the introduction of a minimalistic version of the hybrid algorithm (advocating the use of smaller guiding catheters), as well as the initiation of the Ultrasound Guided Transfemoral Puncture in Complex Large-bore PCI Trial (ULTRACOLOR; ClinicalTrials.gov: NCT04837404)2021. The utilisation of the biradial approach could be considered to reduce the occurrence of concomitant complications in patients already at risk for prolonged hospitalisation. Systematically adopting the biradial approach could potentially enable an even greater percentage of SDD, given its inherently lower risk of bleeding and vascular complications, compared with a femoral approach19. However, sufficient operator expertise would be required. To conclude, each arterial access site and concomitant guiding catheter carries advantages and limitations. The modern hybrid operator should be proficient in all approaches and should tailor the final setup to the individual patient in order to maximise both technical and procedural success22.
Limitations
Several limitations should be addressed. First, the observational nature of this study in a single CTO centre leaves the results subject to possible selection bias. Second, the criteria for non-SDD are not uniformly defined, and thus the decision for hospitalisation was left to the attending physician. This could potentially have led to a higher admission rate amongst patients with an increased risk profile and subsequent higher event rate at follow-up – although this was not reflected by our results. Third, if the clinical likelihood of periprocedural MI was low, cardiac enzymes were not routinely obtained. This could have led to an underestimation of periprocedural MI in the SDD group. As such, periprocedural MI has not been included in the analysis of temporal trends in the MACE rate. Fourth, the reason for a temporal increase in local access site bleeding could not be determined from our data. Possibly, the improved adjudication of events through the electronic data capture system, as well as the implementation of fellowship programmes (and subsequent increase in access site complications), could have driven these results. Fifth, the percentage of missing data for some variables was >10%. These missing variables are assumed to be missing completely at random, hence imputation was not performed. Finally, data on the application of echo-guided access site puncture and vascular closure device failure were not available. As such, no conclusions could be drawn from the present study on the impact of echo-guided puncture or VCD failure on SDD and access site-related complications.
Conclusions
Same-day discharge was successfully achieved in the majority of patients undergoing CTO PCI with large-bore (≥7 Fr) vascular access, paired with a low vascular access complication rate. Similar hospital readmission and MACE rates between SDD and non-SDD patients at 30-day follow-up illustrate the feasibility and safety of SDD. High patient complexity is predictive for hospitalisation, as well as the occurrence of local access site bleeding and vascular access complications. The latter emphasises a need for delicate postprocedural patient care and careful access puncture.
Impact on daily practice
Same-day discharge (SDD) in percutaneous coronary intervention (PCI) of a chronic total occlusion (CTO) is appealing because of the increased patient comfort and economic advantage. However, data on SDD following large-bore vascular access are scarce. We found that SDD is feasible and safe in patients undergoing large-bore CTO PCI, as reflected by a low vascular access complication rate and similar low hospital readmission and major adverse cardiovascular event rates between SDD and non-SDD patients at 30-day follow-up. These results may drive the implementation of SDD following large-bore CTO PCI, improving both patient comfort and hospital capacity in daily practice.
Acknowledgements
Dr Adriaan Wilgenhof has been supported by a research grant provided by the DigiCardioPaTh PhD programme.
Conflict of interest statement
The authors have no conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.