Introduction
The coexistence of coronary artery disease (CAD) and severe aortic stenosis is a frequent and complex clinical scenario, affecting up to 80% of patients undergoing transcatheter aortic valve implantation (TAVI). As the profile of TAVI candidates evolves − with younger patients and longer life expectancies − the prognostic implications of CAD become increasingly relevant. In addition, while aortic stenosis is a life-threatening condition requiring treatment to reduce overall mortality, the management of concomitant CAD is also crucial to improve symptoms. Treating significant CAD may undermine the benefits of TAVI, leading to persistent angina, adverse cardiac events over time, and reduced quality of life. However, stable CAD rarely necessitates urgent intervention, and percutaneous coronary intervention (PCI) carries potential risks (including bleeding, stroke, and acute kidney injury) without clear benefits in this setting. Although two randomised trials investigated this delicate issue, whether treating bystander CAD in patients undergoing TAVI is associated with favourable prognostic implications or merely adds procedural risks remains a matter of debate.
PROS
Josep Rodés-Cabau, MD, PhD; Marisa Avvedimento, MD
Due to the shared pathophysiology of aortic stenosis (AS) and atherosclerotic disease, more than half of patients with severe AS exhibit some degree of obstructive CAD, establishing coronary angiography as a routine examination to depict its presence before aortic valve replacement, whether surgical or transcatheter1. While obstructive CAD is routinely addressed at the time of surgical aortic valve replacement, the need for coronary revascularisation in TAVI candidates remains an unresolved issue. Three key points support the clinical benefit of PCI in TAVI recipients, with careful patient (and coronary anatomy) selection playing a pivotal role.
Why? Impact of severe CAD on angina symptoms and functional status
The primary goal of the TAVI procedure is not only to enhance survival but also functional status by relieving symptoms and ameliorating functional capacity. However, in TAVI candidates with severe, functionally significant coronary lesions, treating AS may extend life expectancy but may not sufficiently improve quality of life. Indeed, the coexistence of CAD is a strong contributing factor to persistent anginal symptoms, potentially hindering the overall benefit of the TAVI procedure23. In this context, addressing CAD can provide greater health benefits than performing TAVI alone, including improvements in angina relief, physical performance and quality of life.
When? Favourable outcomes of PCI pre-TAVI
PCI performed as part of the pre-TAVI work-up has consistently proven feasible and successful in most cases, even when addressing complex coronary lesions. Satisfactory midterm results have been reported, with low rates of target lesion failure (stent thrombosis and clinical restenosis at 2 years: 0.4% and 2.3%, respectively)4. These outcomes are comparable to those observed in all-comer PCI populations outside the TAVI setting, providing reassuring evidence regarding the safety of combined PCI and TAVI procedures. Moreover, incomplete revascularisation and persistent angina after TAVI have been linked to poorer outcomes, including increased coronary events and cardiac death13. Performing PCI before TAVI may help to prevent coronary events stemming from untreated lesions and reduce the likelihood of unplanned revascularisation. Indeed, PCI failure rates increase in patients with prior TAVI, partly due to the interference between the transcatheter valve and the coronary ostia that can challenge or even preclude coronary revascularisation, which would likely have a negative impact on patient prognosis1.
Who? Appropriate coronary anatomy selection
To date, two randomised clinical trials have assessed the role of PCI in patients undergoing TAVI. In the PercutAneous Coronary inTervention prIor to transcatheter aortic VAlve implantaTION (ACTIVATION) trial, angiography-guided PCI pre-TAVI did not significantly reduce death or rehospitalisation rates at 1 year compared to medical treatment5. However, several limitations – such as premature enrolment termination, the exclusion of patients with more severe angina (Canadian Cardiovascular Society class III), lack of invasive physiology assessment, and an unrestricted CAD definition (stenosis ≥70%) – prevent firm conclusions. The third Nordic Aortic Valve Intervention (NOTION-3) trial constitutes the last and most valuable evidence in this scenario. In TAVI candidates with stable CAD, defined by a fractional flow reserve (FFR) ≤0.80 or a coronary stenosis of at least 90% as assessed by angiography, coronary revascularisation (PCI) was associated with a significant 29% reduction in all-cause mortality, myocardial infarction, or urgent revascularisation at a median follow-up of 2 years compared to conservative management6. Indeed, PCI decreased the risk of myocardial infarction by about 50%. This discrepancy with the ACTIVATION trial likely stems from coronary anatomy selection bias, as prior studies involving moderate or non-functionally significant lesions also failed to show clear benefits from routine revascularisation.
Revascularisation of bystander CAD in TAVI recipients can improve both prognosis and quality of life, provided that careful selection is performed. The decision to perform PCI should primarily be based on the angiographic degree of disease severity, with truly severe or physiologically significant stenoses located in the proximal-mid segments of major coronary arteries being the target of a default strategy. However, decisions should be also individualised according to the patient’s age and comorbidities, functional status, and life expectancy, as well as bleeding risk.
Conflict of interest statement
J. Rodés-Cabau has received research grants and consultant/speaker fees from Edwards Lifesciences and Medtronic. M. Avvedimento reports no conflict of interest.
Cons
Tiffany Patterson, PhD; Benedict McDonaugh, MSc
Coronary artery disease coexists in a large proportion of patients with severe aortic stenosis (up to 80% in some series), the management of which continues to generate debate within Heart Teams across Europe and internationally1. Fundamentally, severe aortic stenosis is a life-threatening condition, whereas concomitant stable coronary artery disease is not. Therefore, the focus in these patients should always be relief of the aortic stenosis by TAVI. However, in the presence of bystander coronary disease, questions remain as to how best to minimise periprocedural risk and optimise longer-term outcomes.
There have been two recent randomised controlled trials comparing pre-TAVI PCI to a conservative approach, neither of which demonstrated an increase in periprocedural (TAVI) events in the control arm56. This could, in part, be due to the cohort of patients, who were younger and less comorbid than their counterparts 17 years ago, but also next-generation devices, delivery systems and operator experience with procedural risks, now quoted to be in the region of 2%.
Prior to the publication of the ACTIVATION trial results, practice was already changing: TAVI operators had moved away from performing routine pre-TAVI coronary angiography, to reduce hospital visits, and there had been a reduction in routine pre-TAVI PCI, in order to minimise stroke and acute kidney injury prior to TAVI (Figure 1). With no demonstrable difference in the combined primary endpoint of death or rehospitalisation at 1 year and increased bleeding rates in the PCI arm post-randomisation, cardiologists were further deterred from performing pre-TAVI PCI.
The NOTION-3 Trial investigators present a different demographic of patients; in this refined cohort, patients with a low glomerular filtration rate were excluded, and patients exhibited a lower incidence of peripheral arterial disease, hence, the lower overall rates of bleeding in the PCI arm (although this was numerically higher compared to the conservative arm). Furthermore, fewer patients had prior myocardial infarction (MI), coronary artery bypass grafting or PCI in the trial cohort. The combined primary endpoint of death, MI and urgent revascularisation (predominantly non-ST-elevation MI [NSTEMI]) just reached statistical significance at 2 years, with a numerical difference of 21 events between the two groups for the primary endpoint despite the presence of significant coronary lesions (stenosis >90% on angiography and/or FFR <0.8) in all patients.
Post-TAVI coronary access is also a concern in these patients, and it is still prudent to select a valve with favourable coronary access in patients with concomitant coronary disease. However, the combination of refined device positioning, reduced stent-frame height, larger stent-frame cell size and commissural alignment increase the feasibility of successful coronary re-access7.
Over the past two decades, numerous randomised trials have questioned the utility of PCI compared to medical therapy in patients with stable coronary disease. These have demonstrated that PCI does not reduce deaths or total MIs but does reduce unplanned revascularisation and spontaneous MI; in patients with significant angina, quality of life is improved with PCI. In patients over 75 years old, the SENIOR-RITA Trial8 supports a conservative approach even in the presence of NSTEMI with no difference in outcomes when followed up to 4 years.
Extrapolation of these findings to our cohort of TAVI patients then raises the more important question of which endpoints matter to us and our patients, as large registries demonstrate a 1% incidence, at most, of unplanned PCI post-TAVI. Therefore, in the absence of severe left main stem disease or ST-elevation MI, it is sensible to conclude that the most significant lesion is in the aortic valve.
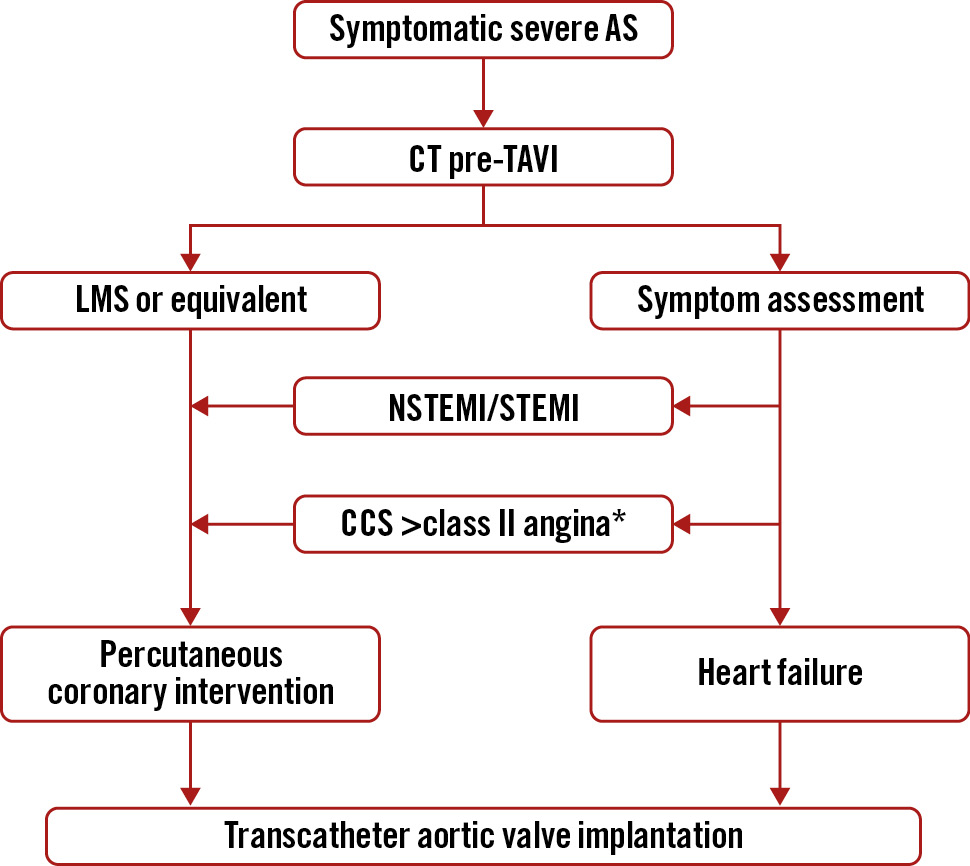
Figure 1. Treatment of significant bystander coronary disease in patients awaiting transcatheter aortic valve implantation. All patients should be discussed in a Heart Team meeting, and the presence of significant frailty or advanced age would favour conservative management. *Considering FFR guidance whilst acknowledging the limitations in the presence of severe AS, it is reasonable to perform PCI before or after TAVI; if it is the latter, consideration should be given to valve choice. CCS: Canadian Cardiovascular Society; CT: computed tomography; FFR: fractional flow reserve; LMS: left main stem; NSTEMI: non-ST-elevation myocardial infarction; STEMI: ST-elevation myocardial infarction
Conflict of interest statement
T. Patterson has no conflicts of interest to declare in relation to this article. B. McDonough has no conflicts of interest to declare in relation to this article.