Cory:
Unlock Your AI Assistant Now!
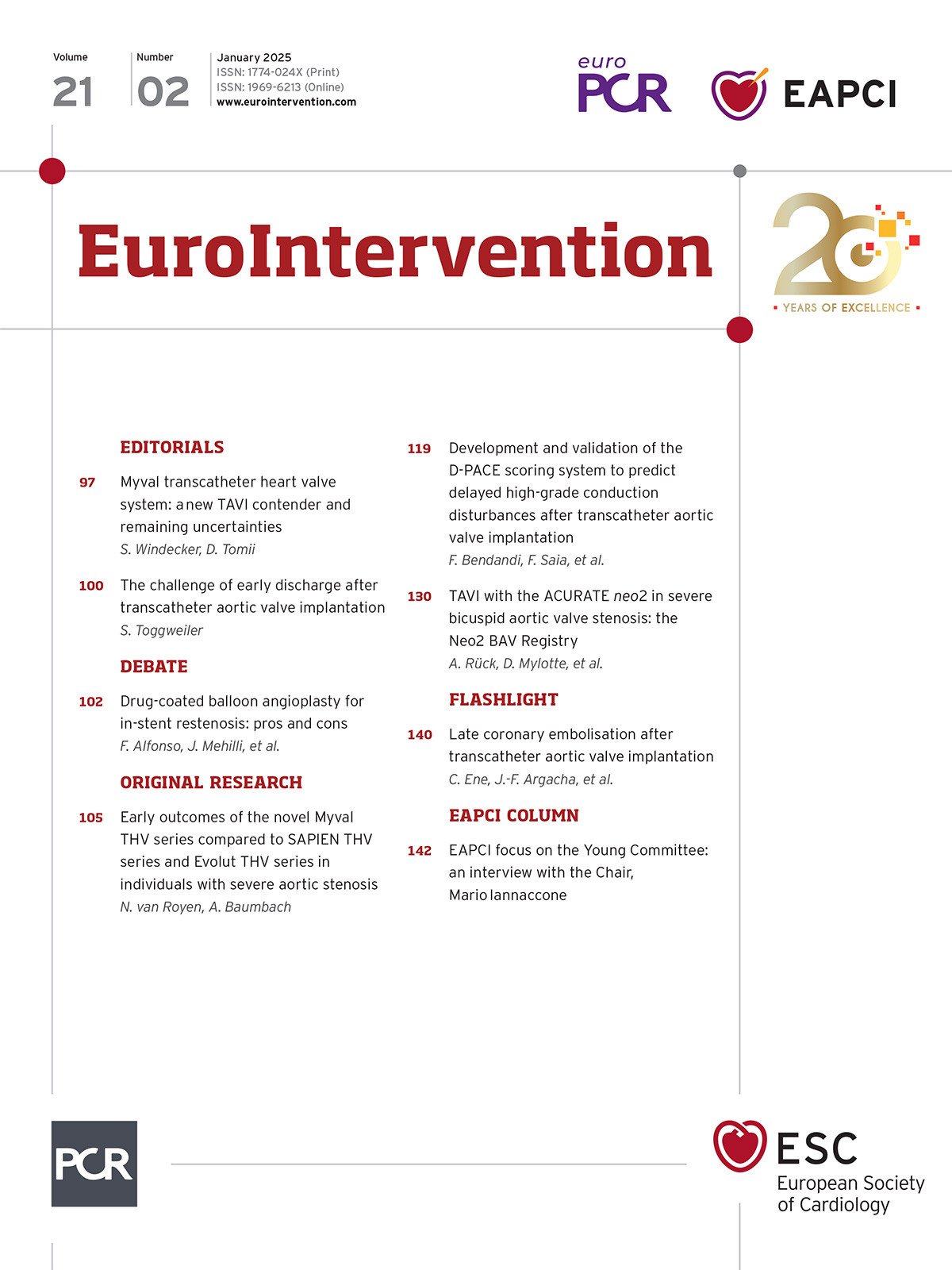
Thanks to next-generation transcatheter valves, physician experience and treatment of lower risk patients, complications after transcatheter aortic valve implantation (TAVI) have continuously declined. In parallel, the increasing number of procedures performed has placed a significant strain on hospital resources and may hamper access for those in need1. In some centres, the waiting list for TAVI extends beyond 1 year. Evidence clearly indicates that such a long waiting time is associated with patient morbidity and mortality2. To mitigate these shortcomings, efforts have been made to shorten the duration of hospitalisation after TAVI.
In this issue of EuroIntervention, Bendandi et al present the D-PACE score which may help to identify candidates for early (same day or next-day) discharge after TAVI3. The score identifies the risk for delayed high-degree atrioventricular (AV) blocks, the major concern when discharging patients early after TAVI. The score incorporates data from pre- and next-day electrocardiograms, the type of valve used, and the implantation depth. Around 40% of patients were identified to be at very low risk for delayed high-degree AV block, and thus were candidates for early discharge. Another 30% were identified as intermediate risk and the remaining 30% as high-risk, and thus not good candidates for early discharge.
The D-PACE score is easy and fast to calculate. However, the score has important limitations. Only a simplified version (D-PACE AF) may be used in patients with atrial fibrillation, and, as it was mainly derived from data from SAPIEN and Evolut platforms, it should not be generalised to other self-expanding valves with different distributions of radial strength. Despite these limitations, the authors should be congratulated for adding to the literature of this hot topic. Indeed, the duration of hospitalisation varies widely between countries and centres and establishing an early discharge programme may be challenging for different reasons.
One such reason is complications other than high-degree AV blocks. Less frequent complications such as ischaemic stroke, major vascular complications, bleeding, or acute kidney failure may prevent early discharge.
Another consideration is balancing the risks and benefits of early discharge. Performing a procedure with an excellent haemodynamic result and without complications is more important than discharging patients early. Depending on patient selection, between 5-10% of patients may require readmission within 30 days after TAVI. This may result in physicians being more cautious, particularly in lower volume centres. Furthermore, a longer hospitalisation may also have some patient benefit. For instance, paroxysmal atrial fibrillation may be detected during a prolonged period of in-hospital observation.
Patient preference is another factor to take into consideration. Despite treatment of younger and lower-risk patients, the mean age of TAVI patients in Switzerland has remained unchanged, around 81 years old. Such elderly patients and their relatives may feel uncomfortable when discharged very early.
One must also consider the decisions that must be made after the procedure rather than before. Patients with a high likelihood for early discharge may be identified with scores such as the D-PACE score, but even in those, next-day discharge is not guaranteed as the final decision can only be made after the procedure. This comes with several challenges for the hospital as well as the patients and their relatives. Ideally, it should be known in advance if a bed on the ward can be used for another patient or not.
There are also historical barriers to early discharge. Hospitals are so-called expert organisations. Because of complex stakeholder engagement, changes are difficult to achieve in the absence of a pressing clinical need. While some physicians may be motivated to optimise their patient pathways, they may face strong “political” resistance forcing them to leave their established TAVI programme unchanged.
Likewise, administrative over-regulation and complicated financial incentives may prevent early discharge after TAVI. For instance, in Switzerland, a hospital is required to hospitalise the patient for at least 2 nights to receive full reimbursement. If a patient is discharged the next day, the hospital receives about €7,000 less in reimbursement. As one night on the ward increases costs by €800, the institution faces a net loss of €6,200. Similar bureaucracy exists in Germany. With such regulations, the governments incentivise longer hospitalisations. The reason for and benefit of such measures remain unclear.
On the other hand, in Scandinavian countries and in the UK, hospitals receive a fixed reimbursement, regardless of the duration of hospitalisation and potential complications, stimulating earlier discharge. In other countries, there are fixed budgets for cardiovascular procedures, resulting in similar motivations.
How can the adoption of early discharge and lean TAVI be encouraged? The fact that many studies now examine options for same-day or next-day discharge after TAVI underscores how far this procedure has come and how widely it has been adopted. However, many centres still perform their procedures under general anaesthesia, with transoesophageal echocardiography, or with a surgical cut-down. Patients are admitted the day before TAVI and not on the same day. The most frequent reasoning used for not changing a TAVI programme is the absence of an obvious clinical need and, as described above, strong historical barriers (we have always done it like this, it works well for us, etc.) and the complex engagement of different stakeholders. Change usually starts with a physician leading the TAVI programme aiming to overcome these challenges. In doing so, it is crucial to (a) elaborate and communicate the potential benefits for the patients and the hospital, and (b) include all stakeholders in the change management process. Such a lean, optimised TAVI programme may dramatically decrease the utilisation of hospital resources, and increase financial benefits, independency, patient and employee satisfaction1. This price is worth the effort.
Conflict of interest statement
S. Toggweiler has received honoraria from Medtronic, Boston Scientific, Biosensors, Hi-D Imaging, Abbott Vascular, Medira, Shockwave, Teleflex, atHeart Medical, Cardiac Dimensions, Polares Medical, Amarin, Sanofi, AstraZeneca, Recor Medical, Daiichi Sankyo, and Bayer; has received institutional research grants from Edwards Lifesciences, Abbott Vascular, Boston Scientific, Fumedica, Novartis, Boehringer Ingelheim, and Polares Medical; and holds equity in Hi-D Imaging.