Cory:
Unlock Your AI Assistant Now!
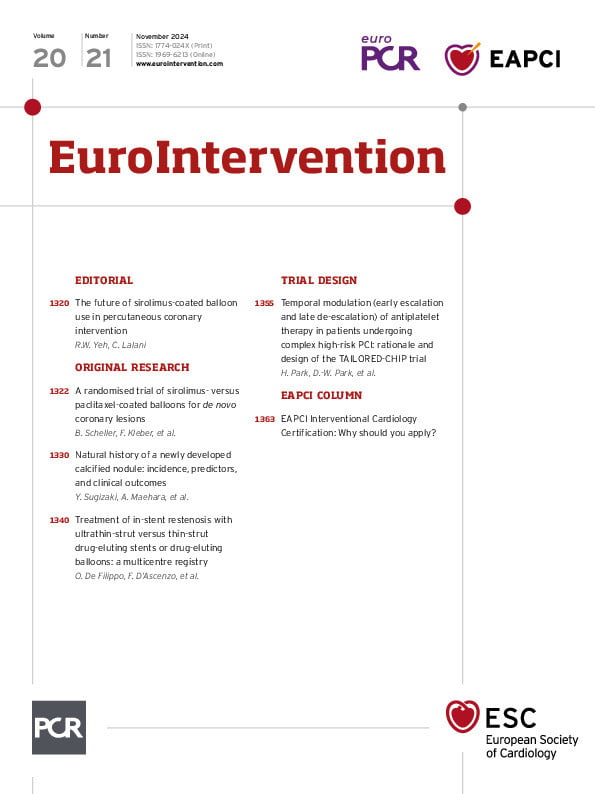
Paclitaxel drug-coated balloons (DCBs) have become a mainstay for treatment of coronary in-stent restenosis (ISR) for more than a decade in Europe, more recently in Asia, and are now available for this indication in the United States12. More recently, there has been a surge in interest in exploring the utility of DCBs in de novo coronary disease, as a means of potentially averting the year-on-year growth in adverse events attributable to stented vessels3. In addition, a number of manufacturers have invested in the development of new DCBs employing non-paclitaxel active ingredients, most commonly sirolimus. With these developments come important questions about the use of DCBs in coronary disease: in which lesions should DCBs be used, and which DCBs are most effective for use?
In this issue of EuroIntervention, Scheller et al aim to address the latter question by comparing rates of late lumen loss (LLL) between patients with de novo lesions who received paclitaxel-coated balloon (PCB) versus sirolimus-coated balloon (SCB) therapy (the SeQuent SCB [B. Braun])4. The authors found no significant difference in LLL between patients who received PCBs versus SCBs, although there was a trend toward more LLL for the SCB, which aligns with the findings of a similarly designed study of the same DCB conducted in Malaysia5. In contrast to the TRANSFORM I trial, which did not establish non-inferiority of a different SCB (the MagicTouch [Concept Medical]) in de novo small vessel disease, these findings demonstrate promise that the SeQuent SCB may be non-inferior to PCBs in simple de novo lesions6.
Paclitaxel has been the most commonly used agent for DCBs because of several distinct biochemical advantages it may possess for a balloon application. The lipophilic and hydrophobic properties of paclitaxel help facilitate rapid tissue uptake of the drug and the irreversible, cytotoxic mechanism of action helps inhibit long-term smooth muscle proliferation7. In contrast, sirolimus is cytostatic and more slowly absorbed, leading to greater dependence on the excipient to ensure adequate tissue uptake of the drug during transient balloon inflation. Given these known advantages, why should paclitaxel alternatives be explored in the first place?
Some of the interest in alternatives to PCBs stems from the results of a meta-analysis that suggested increased mortality with PCB use in peripheral artery disease, a finding that was never redemonstrated in other studies, but did lead the U.S. Food and Drug Administration to issue a warning letter regarding PCB use that was later retracted89. Another driver may be evidence of the improved safety and effectiveness of sirolimus versus paclitaxel drug-eluting stents (DES), although the relative advantages of sirolimus compared with paclitaxel are likely distinct in the setting of a stent versus balloon application. An important question thus remains as to what advantages SCBs will have over PCBs, and whether these differences will be demonstrable in a randomised clinical trial.
Looking forward, as additional studies continue to evaluate different drugs and excipients for DCBs, it will become increasingly important that such studies are powered to evaluate not only the mechanical impacts of DCBs, but also long-term clinical endpoints, to better understand which DCBs provide benefit and whether the benefit of DCBs is truly a class effect.
Conflict of interest statement
C. Lalani receives funding from NIH grant T32HL160522, unrelated to this work. R.W. Yeh consults for Boston Scientific, Abbott, Medtronic, and Edwards Lifesciences; and receives research funds from Boston Scientific, Abbott, and Medtronic, unrelated to this work.