Abstract
BACKGROUND: Endovascular therapy (EVT) has become the preferred treatment modality for femoropopliteal disease. However, there is limited evidence regarding its procedural and clinical outcomes according to the affected area.
AIMS: The aim of this study is to investigate clinical outcomes and device effectiveness according to treatment extent in the superficial femoral artery (SFA), popliteal artery (PA), or both.
METHODS: In this study, we analysed EVT for SFA (2,404 limbs), PA (155 limbs), SFA/PA (383 limbs) using the population in the K-VIS ELLA (Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases) registry. The primary endpoint was target lesion revascularisation (TLR) at 2 years.
RESULTS: The SFA/PA group exhibited a higher prevalence of anatomical complexity, characterised by long lesions, moderate to severe calcification, and total occlusion. The procedures were successful in 97.2% of SFA, 92.9% of PA, and 95.6% of SFA/PA EVTs. The 2-year TLR rates were 21.1%, 18.6%, and 32.7% in the SFA, PA, and SFA/PA groups, respectively. SFA/PA EVT was associated with a significantly increased risk for TLR compared to the SFA group (adjusted hazard ratio [HR] 1.48 [1.09-2.00]; p=0.008) and a trend towards an increased risk compared to the PA group (adjusted HR 1.80 [1.00-3.27]; p=0.052). After overlap weighting, the use of a drug-coated balloon (DCB) was shown to be beneficial, with the lowest TLR rate after SFA and SFA/PA EVT.
CONCLUSIONS: In this large real-world registry, SFA/PA EVT was associated with an increased risk for TLR at 2 years compared to the SFA or PA EVT groups, with favourable outcomes when using a DCB or drug-eluting stent in the SFA/PA EVT group.
Peripheral artery disease (PAD) affects more than 230 million people worldwide and is increasingly recognised as a major comorbidity resulting in serious health conditions, including claudication, amputation, and mortality1. Endovascular therapy (EVT) has emerged as an important treatment modality for patients with peripheral artery disease due to its less invasive nature and acceptable efficacy2.
EVT for femoropopliteal disease has evolved rapidly over the last decade. A newer class of treatment devices, including drug-coated balloons (DCB) and drug-eluting stents (DES), has improved clinical outcomes after EVT for femoropopliteal disease3456. In clinical trials and real-world registries, femoropopliteal disease has generally been treated as a single entity. However, anatomical and physiological differences between the superficial femoral artery (SFA) and popliteal artery (PA) clearly exist, and these differences can possibly affect the interventional approach, procedural success, and long-term clinical outcomes in patients undergoing EVT for femoropopliteal disease7.
Nonetheless, there is limited evidence regarding the clinical impact of the location of the disease (SFA, PA or both) on procedural and long-term clinical outcomes after EVT. Furthermore, controversy still exists about the effectiveness of various final treatment devices according to the extent of femoropopliteal disease. Therefore, we investigated the clinical significance of treatment extent in patients undergoing EVT for femoropopliteal disease on periprocedural and long-term clinical outcomes and compared the effectiveness of final treatment devices at each treatment extent level.
Methods
STUDY DESIGN AND POPULATION
The K-VIS ELLA (Korean Vascular Intervention Society Endovascular Therapy in Lower Limb Artery Diseases) registry enrolled patients diagnosed with lower extremity PAD undergoing EVT at 19 cardiovascular centres in the Republic of Korea since 2006 (ClinicalTrials.gov: NCT02748226). A comprehensive description of the study’s design and the criteria for inclusion/exclusion have been previously published8. Overall, 4,393 limbs (2,951 patients) were included in this registry. After excluding patients who did not receive EVT for SFA or PA lesions, including those with in-stent restenosis lesions, prior lower extremity amputation, who lacked follow-up data, or those with insufficient data regarding the mode of EVT, a final cohort of 2,942 limbs from 2,275 patients was subjected to analysis for this study (Figure 1).
The study population was subsequently divided into three distinct groups based on the extent of EVT in the target limbs: (1) EVT for the SFA (SFA group: 2,404 limbs [1,868 patients]), (2) EVT for the PA (PA group: 155 limbs [122 patients]), and (3) EVT for both SFA and PA (SFA/PA group: 383 limbs [285 patients]). The study protocol received approval from the institutional review board at each participating centre and was executed in compliance with the principles outlined in the Declaration of Helsinki. Informed consent was obtained from all patients, except those whose data were collected retrospectively.
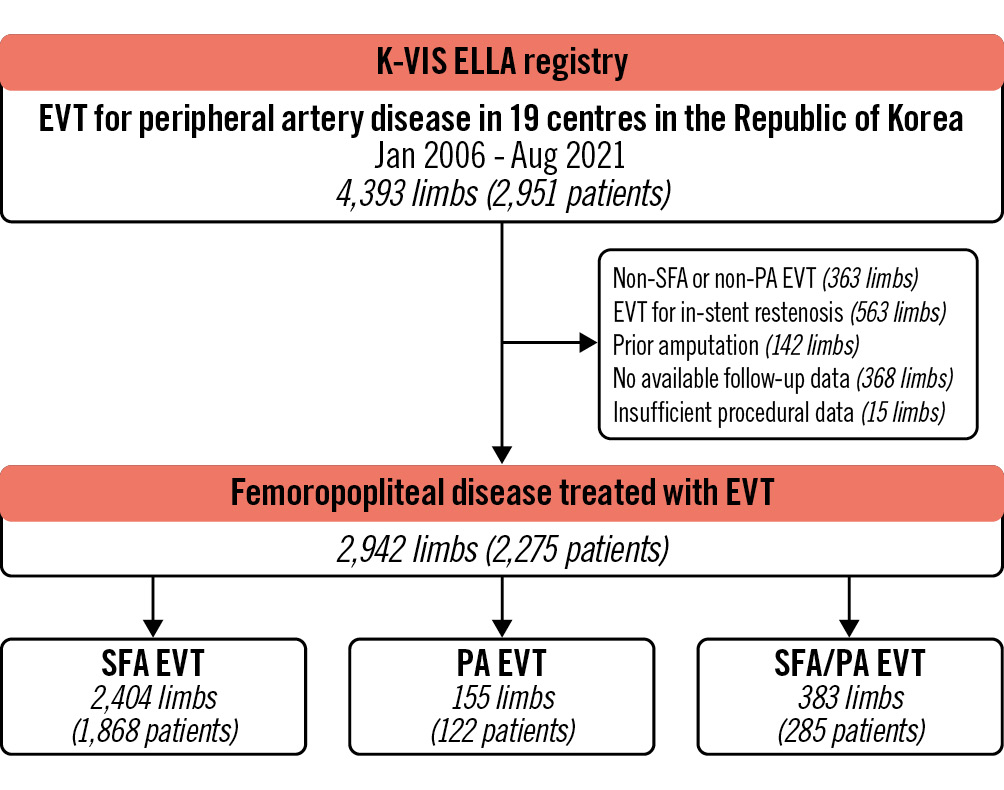
Figure 1. Study flow. EVT: endovascular therapy; PA: popliteal artery; SFA: superficial femoral artery
PROCEDURES AND FOLLOW-UP
Clinical, imaging, and procedural data were obtained from electronic medical records or telephone interviews. The grading of calcification on angiography was determined based on the peripheral arterial calcium scoring system9. Moderate to severe calcification was defined as a calcification grade of 3 or 4. All EVT procedures were conducted by experienced interventional cardiologists. The selection of the treatment strategy, which included factors such as the choice of access route, wire type, wiring technique, the utilisation and type of atherectomy, the use of intravascular imaging, and the final treatment device, was at the discretion of the operator, based on the clinical and anatomical characteristics of each patient. Following balloon angioplasty with either a plain balloon (PB) or DCB, provisional stenting was performed in cases of flow-limiting dissection or residual stenosis greater than 30%. In such cases, patients were categorised into the DCB treatment group. After the initial procedure, patients underwent follow-up evaluations at 6, 12, and 24 months. During the follow-up period, optimal medical treatment, such as antithrombotic agents or lipid-lowering medications, was prescribed by the attending physician.
DEFINITIONS AND CLINICAL OUTCOMES
The success of the EVT procedure was determined by the presence of residual stenosis measuring less than 30% without any flow-limiting dissection. The primary endpoint of the study was target lesion revascularisation (TLR), defined as any subsequent intervention performed within a 5 mm segment proximal or distal to the initially treated target segment during follow-up, with more than 50% angiographic diameter stenosis, accompanied by worsening symptoms and a decline>0.15 in the ankle-brachial index in comparison to the immediate postprocedural ankle-brachial index. Major amputation was defined as amputation of the index limb occurring above the ankle level. Loss of patency was identified when patency, assessed via physiological means (a decrease in ankle-brachial index>0.15) or imaging modalities (such as duplex ultrasound, computed tomography, or angiography), was no longer maintained with symptom aggravation by at least 1 Rutherford category change. A major adverse limb event (MALE) was defined as a composite of TLR or major amputation of the target limb.
STATISTICAL ANALYSIS
Continuous variables are expressed as mean±standard deviation and compared using either one-way analysis of variance or the Kruskal-Wallis test. Categorical variables are presented as counts (%) and analysed using the chi-square or Fisher’s exact test, as appropriate. Clinical events observed during follow-up were also assessed, and cumulative event rates and survival curves were generated using the Kaplan-Meier method. All clinical outcomes were reported based on limb-level data, except for mortality, which was analysed based on patient-level data. The follow-up duration was censored either at the time of a clinical event or at the last follow-up, whichever came first. Cox proportional hazards models were used to adjust for confounding factors, including age, sex, body mass index, smoking status, hypertension, diabetes, dyslipidaemia, chronic kidney disease, coronary artery disease, prior EVT, chronic limb-threatening ischaemia, concomitant interventions involving common femoral, iliac, or infrapopliteal lesions, lesion characteristics including total occlusion, TransAtlantic Inter-Society Consensus (TASC) II classification, lesion length, calcification, the final treatment device, medications at discharge (aspirin, clopidogrel, cilostazol, statin), and the year of procedure. Multiple comparisons of Cox proportional hazards models were conducted using the Tukey method to compare clinical outcomes between the three groups defined by femoropopliteal treatment extent. Moreover, the separated propensity scores were calculated for each treatment location group to compare the effectiveness of the final treatment devices (PB, bare metal stent [BMS], DCB, and DES). The propensity score was utilised to estimate the overlap weighting that highlights the target population with the most overlap in observed characteristics between treatments by continuously reducing the weight of units at the tails of the propensity score distribution1011. The standardised mean differences were calculated to assess the balance between plain device and drug-eluting device treatment groups. The cumulative event rates, survival curves, and hazard ratios (HRs) were estimated using the weighted Kaplan-Meier method, and Cox proportional hazards models were additionally adjusted for medications at discharge and the year of procedure to compare the device effectiveness. All reported p-values are two-sided, and statistical significance was defined as p<0.05. The statistical analyses were performed using R software, version 4.2.3 (R Foundation for Statistical Computing).
Results
BASELINE CHARACTERISTICS
The mean age of the study population was 69.4 years, with 2,397 (81.5%) male patients, based on limb-level data. In the comparison between groups, the SFA group exhibited the highest percentage of male patients, as well as the highest prevalence of current smokers and individuals with coronary artery disease (Table 1, Supplementary Table 1). The SFA/PA group had the highest prevalence of chronic kidney disease. There were no significant differences in the prevalence of hypertension, diabetes, or dyslipidaemia among the groups. The PA group and SFA/PA group had a history of more chronic kidney disease and prior EVT procedures. Additionally, challenging anatomical characteristics, such as TASC classification C or D, long lesions, total occlusions, and moderate or greater calcification, were most prevalent in the SFA/PA group.
Table 1. Baseline demographics.
| Total (N=2,942) |
SFA (N=2,404) | PA (N=155) | SFA/PA (N=383) | p-value | |
|---|---|---|---|---|---|
| Age, years | 69.4±10.4 | 69.5±10.1 | 68.3±10.5 | 69.1±12.2 | 0.305 |
| Male | 2,397 (81.5) | 1,984 (82.5) | 121 (78.1) | 292 (76.2) | 0.007 |
| Body mass index, kg/m2 | 23.3±3.4 | 23.3±3.4 | 23.8±3.2 | 23.0±3.6 | 0.046 |
| Current smoker | 804 (27.3) | 675 (28.1) | 38 (24.5) | 91 (23.8) | 0.153 |
| Hypertension | 2,220 (75.5) | 1,831 (76.2) | 114 (73.5) | 275 (71.8) | 0.156 |
| Diabetes | 1,865 (63.4) | 1,524 (63.4) | 99 (63.9) | 242 (63.2) | 0.989 |
| Diabetes on insulin | 482 (16.4) | 403 (16.8) | 29 (18.7) | 50 (13.1) | 0.138 |
| Dyslipidaemia | 1,715 (58.3) | 1,398 (58.2) | 90 (58.1) | 227 (59.3) | 0.917 |
| Chronic kidney disease | 755 (25.7) | 595 (24.8) | 43 (27.7) | 117 (30.5) | 0.045 |
| End stage renal disease | 404 (13.7) | 306 (12.7) | 29 (18.7) | 69 (18.0) | 0.004 |
| Coronary artery disease | 1,385 (47.1) | 1,189 (49.5) | 53 (34.2) | 143 (37.3) | <0.001 |
| Chronic obstructive lung disease | 104 (3.5) | 92 (3.8) | 1 (0.6) | 11 (2.9) | 0.087 |
| Prior stroke | 515 (17.5) | 429 (17.8) | 28 (18.1) | 58 (15.1) | 0.426 |
| Prior endovascular therapy | 926 (31.5) | 735 (30.6) | 54 (34.8) | 137 (35.8) | 0.082 |
| Chronic limb-threatening ischaemia | 1,161 (39.5) | 888 (36.9) | 73 (47.1) | 200 (52.2) | <0.001 |
| TASC II type C or D | 1,675 (56.9) | 1,363 (56.7) | 64 (41.3) | 248 (64.8) | <0.001 |
| Lesion length ≥150 mm | 1,281 (43.5) | 1,048 (43.6) | 11 (7.1) | 222 (58.0) | <0.001 |
| Total occlusion | 1,480 (50.3) | 1,159 (48.2) | 83 (53.5) | 238 (62.1) | <0.001 |
| Moderate/severe calcification | 920 (31.3) | 743 (30.9) | 33 (21.3) | 144 (37.6) | 0.001 |
| Data are presented as mean±standard deviation or n (%). PA: popliteal artery; SFA: superficial femoral artery; TASC: TransAtlantic Inter-Society Consensus | |||||
PROCEDURAL OUTCOMES
Table 2 and Supplementary Table 2 provide an overview of the procedural characteristics of the study population based on limb-level and patient-level data. Intraluminal wiring was the primary method used in the three groups. Atherectomy was most frequently employed in the SFA/PA group (15.4%), with a higher proportion of rotational atherectomy use observed in both the SFA/PA and PA groups compared to the SFA group. Regarding drug-eluting devices, DCB and DES were utilised in 24.3% and 8.0% of cases, respectively, in the SFA group, and 43.6% and 6.8% in the SFA/PA group (p<0.001). Notably, DCB (35.5%) were the exclusive drug-eluting devices used in the PA group, whereas DES were not used. The technical success rates were 97.2%, 92.9%, and 95.6% in the SFA, PA, and SFA/PA groups, respectively (p=0.006). Vascular rupture and bleeding were most frequently observed in the SFA/PA group. There were no significant differences in the use of antithrombotic and antidyslipidaemia agents at discharge, except for cilostazol, which was administered more often in the SFA group.
Table 2. Procedural characteristics.
| Total (N=2,942) | SFA (N=2,404) | PA (N=155) | SFA/PA (N=383) | p-value | |
|---|---|---|---|---|---|
| Wiring approach | 0.062 | ||||
| Intraluminal | 2,396 (82.3) | 1,960 (82.4) | 135 (87.7) | 301 (79.2) | |
| Subintimal | 516 (17.7) | 418 (17.6) | 19 (12.3) | 79 (20.8) | |
| Atherectomy | <0.001 | ||||
| Not used | 2,716 (92.3) | 2,252 (93.7) | 140 (90.3) | 324 (84.6) | |
| Rotational | 119 (4.0) | 70 (2.9) | 10 (6.5) | 39 (10.2) | |
| Directional | 107 (3.6) | 82 (3.4) | 5 (3.2) | 20 (5.2) | |
| Final treatment | <0.001 | ||||
| Plain balloon | 922 (31.3) | 736 (30.6) | 75 (48.4) | 111 (29.0) | |
| Bare metal stent | 996 (33.9) | 892 (37.1) | 25 (16.1) | 79 (20.6) | |
| Drug-coated balloon | 805 (27.4) | 583 (24.3) | 55 (35.5) | 167 (43.6) | |
| Drug-eluting stent | 219 (7.4) | 193 (8.0) | 0 (0) | 26 (6.8) | |
| Concomitant treatment | |||||
| Common femoral lesion | 96 (3.3) | 50 (2.1) | 2 (1.3) | 44 (11.5) | <0.001 |
| Infrapopliteal lesion | 668 (22.7) | 454 (18.9) | 68 (43.9) | 146 (38.1) | <0.001 |
| Iliac lesion | 422 (14.3) | 353 (14.7) | 18 (11.6) | 51 (13.3) | 0.473 |
| Technical success | 2,846 (96.7) | 2,336 (97.2) | 144 (92.9) | 366 (95.6) | 0.006 |
| Complications | |||||
| Distal embolisation | 14 (0.5) | 11 (0.5) | 0 (0) | 3 (0.8) | 0.467 |
| Vascular rupture | 33 (1.1) | 19 (0.8) | 3 (1.9) | 11 (2.9) | 0.001 |
| Bleeding | 81 (2.8) | 58 (2.4) | 6 (3.9) | 17 (4.4) | 0.054 |
| In-hospital death | 15 (0.5) | 14 (0.6) | 1 (0.6) | 0 (0) | 0.322 |
| Discharge medications | |||||
| Aspirin | 2,291 (77.9) | 1,887 (78.5) | 112 (72.3) | 292 (76.2) | 0.138 |
| Clopidogrel | 2,397 (81.5) | 1,972 (82.0) | 121 (78.1) | 304 (79.4) | 0.246 |
| Cilostazol | 904 (30.7) | 775 (32.2) | 38 (24.5) | 91 (23.8) | 0.001 |
| Statin | 2,153 (73.2) | 1,762 (73.3) | 114 (73.5) | 277 (72.3) | 0.919 |
| Data are presented as n (%). PA: popliteal artery; SFA: superficial femoral artery | |||||
Clinical outcomes
During the 2 years of follow-up, TLR occurred in 361 limbs (21.1%) in the SFA group, 20 limbs (18.6%) in the PA group, and 83 limbs (32.7%) in the SFA/PA group (p<0.001) (Central illustration, Supplementary Table 3). In addition, the incidence of loss of patency and MALE were highest in the SFA/PA group (73.4% and 33.1%), whereas those rates were similar between the SFA group (61.2% and 21.7%) and PA group (60.7% and 19.9%). All-cause death occurred least in patients in the SFA group. The incidence of major amputation was remarkably low in all groups, without a significant difference.
In a multivariable Cox proportional model with multiple comparisons (Table 3), the SFA/PA group was associated with an increased risk of TLR compared to the SFA group (adjusted HR 1.48, 95% CI: 1.09-2.00; p=0.008) and the PA group (adjusted HR 1.80, 95% CI: 1.00-3.27; p=0.052). There was no difference in the risk of TLR between the SFA and PA groups. The SFA/PA group also showed a significantly increased risk of loss of patency compared to the SFA group and the PA group. There were no differences in all-cause mortality nor in the rate of major amputation between these groups.
Supplementary Table 4 shows the baseline and procedural characteristics between final treatment devices stratified by femoropopliteal treatment extent. The prevalence of concomitant infrapopliteal treatment and chronic limb-threatening ischaemia were highest in those treated with PB for all three treatment groups. The total occlusion rate was highest in the DES group for SFA EVT and in the BMS group for SFA/PA EVT. Long lesions were mostly treated with DES in SFA and SFA/PA EVT and with DCB in PA EVT. After overlap weighting, all baseline and procedural characteristics were well balanced (Supplementary Table 5). The crude and weighted comparison of treated devices are presented in Supplementary Figure 1, Figure 2, and Supplementary Table 6. Generally, the use of drug-eluting devices including DCB and DES was associated with lower TLR rates in SFA and SFA/PA EVT in the weighted analysis. The weighted TLR rates were lowest in the DCB group in the SFA EVT (weighted HR 0.45, 95% CI: 0.31-0.64; p<0.001, compared to the PB group). There was no difference in the treatment effect between devices in PA EVT, with the lowest TLR rate in the BMS group. In SFA/PA EVT, the TLR rate was lowest in the DCB group, while the TLR rate was numerically higher in the BMS group compared to the PB group.
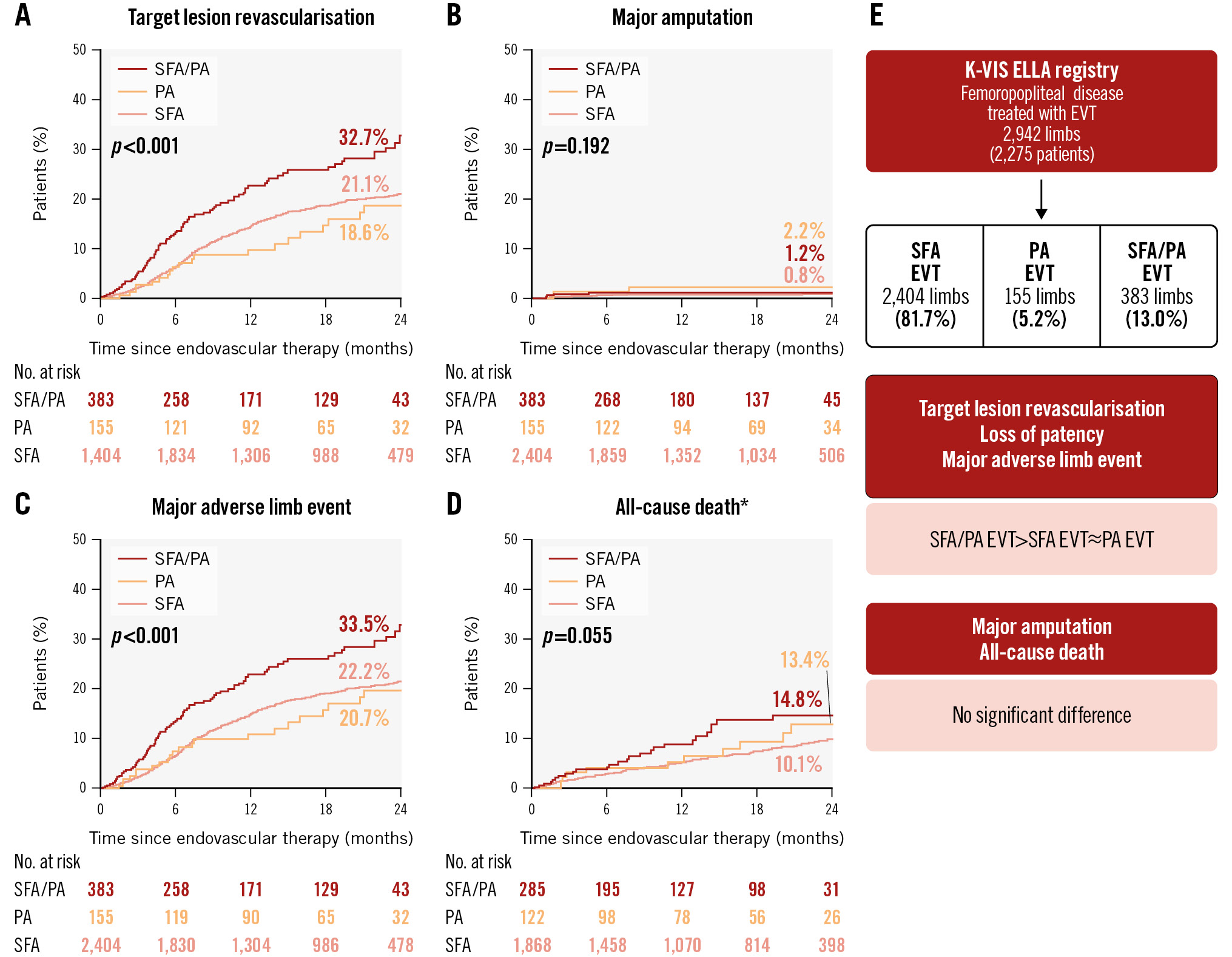
Central illustration. Clinical outcomes of endovascular therapy for femoropopliteal disease over a 2-year period based on treatment extent. *Analysis based on patient-level data. Kaplan-Meier curves for the following clinical outcomes: target lesion revascularisation (A), major amputation (B), major adverse limb event (C), and all-cause death (D). E) summarises the study results. EVT: endovascular therapy; PA: popliteal artery; SFA: superficial femoral artery
Table 3. Multiple comparisons of femoropopliteal treatment location and clinical outcomes.
| Adjusted hazard ratio (95% confidence interval) | p-value | |
|---|---|---|
| Target lesion revascularisation | ||
| PA vs SFA | 0.82 (0.47-1.42) | 0.667 |
| SFA/PA vs SFA | 1.48 (1.09-2.00) | 0.008 |
| SFA/PA vs PA | 1.80 (1.00-3.27) | 0.052 |
| Major amputation | ||
| PA vs SFA | 3.39 (0.61-18.70) | 0.213 |
| SFA/PA vs SFA | 1.36 (0.34-5.42) | 0.859 |
| SFA/PA vs PA | 0.40 (0.06-2.92) | 0.525 |
| Loss of patency | ||
| PA vs SFA | 0.93 (0.70-1.25) | 0.841 |
| SFA/PA vs SFA | 1.30 (1.08-1.56) | 0.002 |
| SFA/PA vs PA | 1.39 (1.01-1.92) | 0.043 |
| Major adverse limb event | ||
| PA vs SFA | 0.87 (0.51-1.48) | 0.809 |
| SFA/PA vs SFA | 1.43 (1.06-1.92) | 0.015 |
| SFA/PA vs PA | 1.64 (0.92-2.90) | 0.106 |
| All-cause death* | ||
| PA vs SFA | 1.31 (0.60-2.84) | 0.695 |
| SFA/PA vs SFA | 1.07 (0.62-1.85) | 0.957 |
| SFA/PA vs PA | 0.82 (0.33-2.02) | 0.858 |
| *Analysis based on patient-level data. PA: popliteal artery; SFA: superficial femoral artery | ||
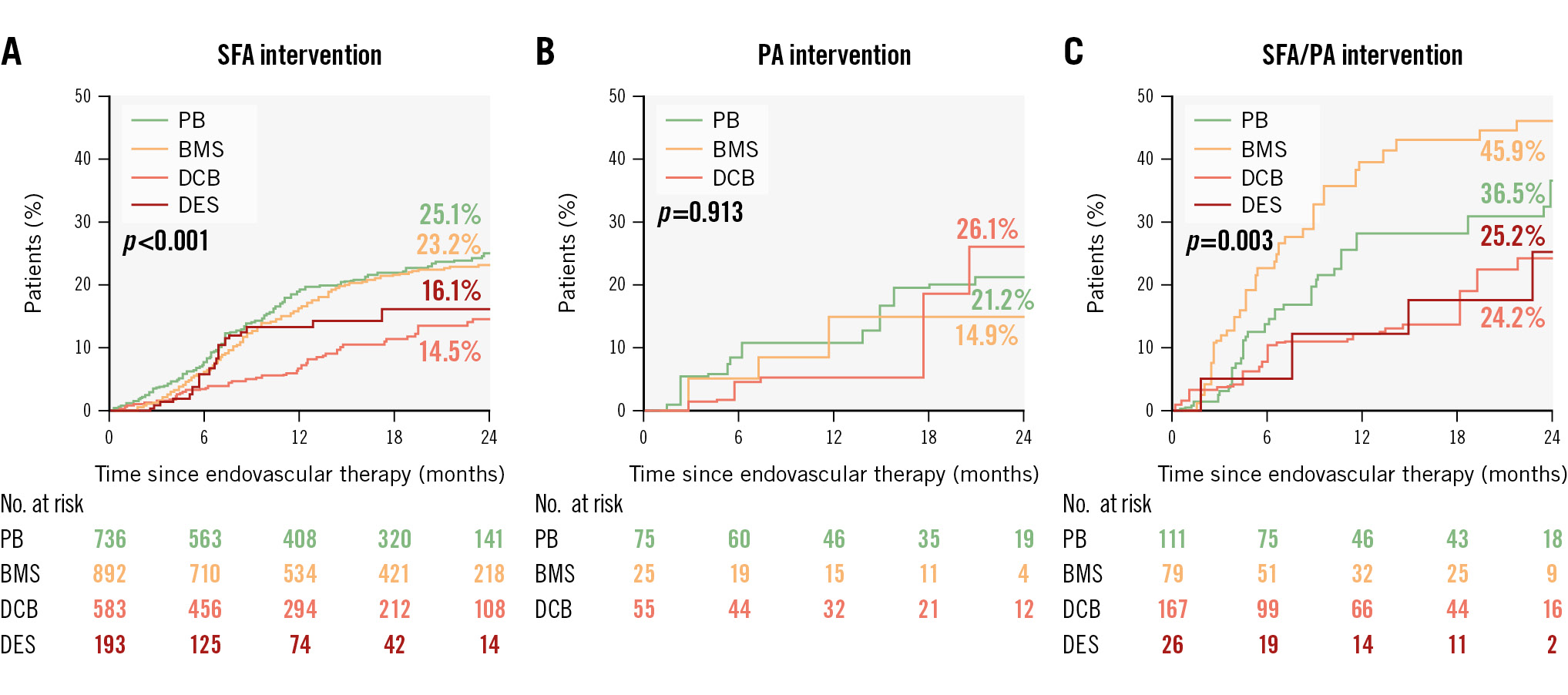
Figure 2. *Analysis based on patient-level data. Kaplan-Meier curves of target lesion revascularisation using overlap weighting between final treatment device groups, stratified by femoropopliteal treatment extent. The curves represent SFA intervention (A), PA intervention (B), and combined SFA/PA intervention (C). BMS: bare metal stent; DCB: drug-coated balloon; DES: drug-eluting stent; PA: popliteal artery; PB: plain balloon; SFA: superficial femoral artery
Discussion
This study investigated the procedural and clinical impact of the treatment extent in patients with femoropopliteal disease undergoing EVT. The study results are summarised as follows: (1) Challenging anatomical characteristics were most prevalent in the SFA/PA group. (2) The technical success rate was lowest in the PA group, and drug-eluting devices including DCB or DES were used most in SFA/PA disease. (3) The prevalence of TLR at 2 years was highest in patients selected for SFA/PA EVT. (4) In multiple comparison analyses, the patients selected for undergoing SFA/PA EVT showed a significantly higher risk for TLR than those undergoing SFA EVT. There was also a trend toward a higher TLR risk in patients undergoing SFA/PA EVT compared to those undergoing PA EVT. (5) In stratified analysis according to femoropopliteal treatment extent, the TLR rate was lowest in the DCB groups in SFA and SFA/PA EVT.
The outcomes of EVT for SFA and PA disease have been evaluated together as femoropopliteal lesions in most published studies. However, in a long segment of femoropopliteal disease, anatomical and physiological differences between the SFA and the popliteal artery exist71213. The SFA is long and straight, with a larger diameter and less external compression, while the PA is relatively short with important branches running below the knee level. Additionally, the popliteal artery is uniquely compressed by an external mechanical force while bending the knee joint. These factors result in differences in procedural approach, techniques, and selection of final devices between SFA and PA EVT. Real-world data indicate that PA EVT is characterised by less use of stents compared to SFA EVT14. In our study, PA EVT showed more concomitant treatment for infrapopliteal lesions, little use of stents, and a lower immediate technical success rate compared to SFA EVT. The strategy of avoiding stents could be one of the reasons for the lower success rate in PA EVT15. To overcome these difficulties, recent studies have investigated the role of atherectomy with antirestenotic therapy using a DCB or an interwoven nitinol stent in PA EVT. The success rate was significantly improved by using an interwoven nitinol stent in PA EVT, with 25% of patients undergoing EVT with PB needing immediate stenting due to a failure to achieve adequate lumen gain1617. However, there is still controversy regarding whether directional atherectomy with antirestenotic therapy could improve technical success in PA EVT1518. All studies about PA EVT have been relatively small; therefore, further studies with large populations are required.
The extent of femoropopliteal disease can vary widely, and thus many factors can affect clinical outcomes after EVT. Lesion length is known to be associated with long-term clinical outcomes after EVT for femoropopliteal disease1920. However, evidence regarding the relevance of disease or treatment extent on long-term outcomes is currently limited. The IN.PACT Global Clinical Study, involving 1,406 patients, reported the lowest freedom from TLR in the SFA/PA EVT group (69.2%) compared to SFA EVT (79.7%) or PA EVT (76.5%) at 3 years using DCB, with a consistent effect after adjusting for lesion length in multivariable analysis21. On the other hand, EVT with the interwoven nitinol stent showed similar 3-year TLR-free rates (69.5%) in patients with SFA disease with or without PA involvement22. A recent large registry involving 19,324 patients undergoing femoropopliteal EVT for patients with claudication showed the highest index limb revascularisation rate in the SFA/PA EVT group and the highest index limb amputation rate in the PA EVT group. Our real-world data include EVTs with all treatment devices and showed the highest TLR rate in the SFA/PA EVT group with similar TLR rates between the SFA and PA EVT groups at 2 years of follow-up. The higher atherosclerotic burden in the SFA/PA group might play a role in developing restenosis after EVT; furthermore, over- or undersizing a DCB in diffuse disease could lead to inadequate acute lumen gain21.
The “leave nothing behind” strategy using DCB has recently emerged as an effective and safe treatment option for femoropopliteal EVT232425. Our data showed that DCB and DES showed relatively lower TLR rates in the SFA and SFA/PA groups. These results are consistent with previous randomised trials and real-world registry data assessing SFA and PA lesions together. EVT with DCB was associated with a significant improvement in primary patency at 1 year compared to EVT with PB34. EVT with DCB was also compared to EVT with DES, and the results showed a similar patency rate in both groups56. In addition, EVT with BMS was associated with a higher TLR rate compared to PB in SFA/PA EVT in this study. This association is believed to be linked to a higher restenosis risk with BMS in extensive atherosclerotic burden due to the metallic scaffold not being coated in an antiproliferative drug. Therefore, the “leave nothing behind” strategy with a drug-eluting device is preferable, especially in the management of extensive femoropopliteal disease. In PA EVT, on the other hand, there were no differences between the three treatment modalities in our study. Not only could the small size of this population mitigate the difference in effect between treatment modalities, but also, the anatomical and procedural differences could affect device effectiveness in isolated PA EVT. Similarly, most previous research is based either on a small number of patients or single-arm studies. If rescue stenting was ignored, 1-year comparisons patency was similar between EVT with PB and BMS17. DCB showed an acceptable 1-year patency21, and there was a trend that the combined treatment of DCB with atherectomy improved 1-year patency compared to EVT with DCB alone15. The lower prevalence of PA involvement in femoropopliteal disease might limit the vigorous investigation of long-term treatment effects between various strategies.
Currently, most evidence with respect to femoropopliteal EVT is limited to midterm follow-up. Therefore, further studies with long-term follow-up comparing the clinical efficacy of different devices in each segment of long femoropopliteal disease are needed. This will enhance understanding of the long-term effect of EVT and clarify the best treatment strategies for each disease segment in femoropopliteal disease.
Limitations
There are several limitations in this study. First, our study primarily serves as a hypothesis-generating investigation because this was an observational study. Therefore, further validation in larger and more diverse cohorts is needed. Second, all analyses were based on treatment extent rather than the area affected by femoropopliteal disease. This fact could limit the proper interpretation of our results because the attending physician determined the treatment extent, which may not have reflected the true atherosclerotic burden and the extent of femoropopliteal disease. Complex SFA/PA disease could have been treated only in the SFA or the PA for simpler procedures, resulting in different procedural and clinical outcomes. Third, in cases where flow-limiting dissection occurred after balloon angioplasty, subsequent treatment strategies may have varied among operators and centres. Our dataset does not provide information regarding the number of bailout stenting procedures following flow-limiting dissection. However, all bailout stenting procedures undergo review by the national health insurance system in the Republic of Korea. The reimbursement criteria are stringent, potentially limiting the number of exceptional cases. Fourth, our data did not include specific treatment information about each segment in the SFA/PA group. There is a possibility of heterogeneous use of devices in limbs with long disease involvement. In addition, there was no uniform indication across the participating centres for the debulking strategy prior to use of the final device, resulting in additional bias in interpreting the effect of the final device. Fifth, small numbers of patients, especially in the PA group, limited the assessment of the effectiveness of various devices. Sixth, TLR events were determined by the attending physician, and the demographic and anatomical characteristics could have affected the decision-making about reintervention for the patients. Seventh, medical treatment following the index EVT was at the discretion of the attending physicians. Lastly, imaging studies and functional assessment to assess patency were not routinely performed for all patients.
Conclusions
In this real-world registry involving a large population undergoing EVT for femoropopliteal disease, SFA/PA EVT was associated with acceptable immediate periprocedural outcomes despite the higher prevalence of anatomical complexity. However, SFA/PA EVT was associated with an increased risk of TLR at 2 years of follow-up compared to the SFA or PA EVT groups. The use of drug-eluting devices including DCB or DES showed favourable outcomes compared to EVT with PB in patients selected for SFA and SFA/PA intervention.
Impact on daily practice
This study provides demographic and procedural characteristics and clinical outcomes following endovascular therapy (EVT) for femoropopliteal disease based on treatment extent. Patients undergoing superficial femoral artery (SFA)/popliteal artery (PA) EVT who suffer from extensive atherosclerotic burden had the highest target lesion revascularisation (TLR) events over 2 years. The stratified analysis based on treatment extent showed that drug-eluting devices, including drug-coated balloons or drug-eluting stents, had the lowest TLR events in these SFA/PA patients. This result suggests that these drug-eluting devices could be the most effective treatment modality for those with long, diffuse femoropopliteal disease involving both the SFA and the PA.
Funding
This study was supported by grants from the Patient-Centered Clinical Research Coordinating Center funded by the Ministry of Health and Welfare, Republic of Korea (grant HC20C0081).
Conflict of interest statement
The authors have no conflicts of interest relevant to this article to declare.
Supplementary data
To read the full content of this article, please download the PDF.