Despite an increasing awareness of the cardiovascular disease burden in women, they are notably underÂrepresented in cardiovascular clinical trials and under- or mistreated in real-world practice1. Coronary artery disease (CAD) exemplifies the sex disparities in cardiovascular medicine. The proportion of women in trials evaluating coronary interventions usually falls below 30%, despite women experiencing higher rates of adverse cardiac events following both percutaneous coronary intervention (PCI) and bypass surgery23.
In this issue of EuroIntervention, Gaudino and colleagues present a post hoc sex-stratified analysis of the International Study of Comparative Health Effectiveness With Medical and Invasive Approaches (ISCHEMIA) trial, with the aim of assessing the probability of undergoing revascularisation for women and men assigned to the invasive treatment arm, along with exploring sex-related variations in the primary outcome and its individual components4. No sex interaction for the effect of an invasive versus conservative treatment approach on the primary composite endpoint, including cardiovascular death, myocardial infarction (MI) and hospitalisation for cardiac causes, was found. However, women in the invasive arm were significantly less likely to undergo revascularisation compared to men (adjusted odds ratio 0.75, 95% confidence interval: 0.57-0.99). Indeed, out of 2,588 patients randomised to the invasive group, 22% (28% of women and 20% of men) did not undergo revascularisation. A lower rate of procedural MI in women (5.9 vs 12.9%; p=0.01) was also observed, aligning with their lower likelihood of undergoing a revascularisation procedure.
The key strength of this analysis lies in the inclusion of the randomised patients from the ISCHEMIA trial (N=5,179) who had evidence of obstructive CAD at coronary computed tomography angiography (CCTA) and/or moderate to severe ischaemia on non-invasive stress testing. This minimised the confounding effect of non-obstructive CAD, which is more prevalent in women and negatively impacts revascularisation rates in all-comers studies1. Despite adjusting for multiple clinical and angiographic variables, the tendency towards a lower likelihood of being referred for revascularisation in women persisted, raising both interest and concern.
Several factors may contribute to such undertreatment, even within the framework of a clinical trial that specifically included patients with obstructive CAD (Figure 1). First, 151 patients from the invasive arm of the ISCHEMIA trial had no ≥50% stenosis at angiographic core lab evaluation, which potentially accounts for up to 26% of the patients who were randomised to intervention and not treated (N=576)4. Discordance between CCTA and invasive angiographic findings has been reported in women5, and the study by Gaudino et al does not specify whether this proportion differed between sexes. Secondly, while the anatomical extent of CAD was considered for adjustment in the final model, the treatment choice might also have been influenced by the invasive physiological assessment, which was performed in roughly 20% of patients and is poorly correlated with the visual degree of stenosis in women6. On the background of sex-related differences in angiographic findings, however, physician bias does undoubtedly play a role. Treating women is perceived as more challenging because of atypical clinical presentation, higher risk of periprocedural bleeding and access-site complications, and lower expected adherence to discharge therapy17. On the other hand, women are notably less aware of their cardiovascular risk and less prone to receive invasive treatments as compared to men (Figure 1). This perception from both physicians and patients has been correlated with a delayed time to reperfusion in the MI setting and could also contribute to greater angina burden and impaired quality of life in women with stable CAD8.
Despite numerous claims, a trend towards the undertreatment of women with CAD is still tremendously evident, and a substantial effort is needed to reverse this. As trialists, we should implement innovative strategies to include sufficient proportions of women in clinical trials. As physicians, we need to be aware of the differences in CAD pathophysiology between men and women and tailor diagnostic and therapeutic approaches accordingly.
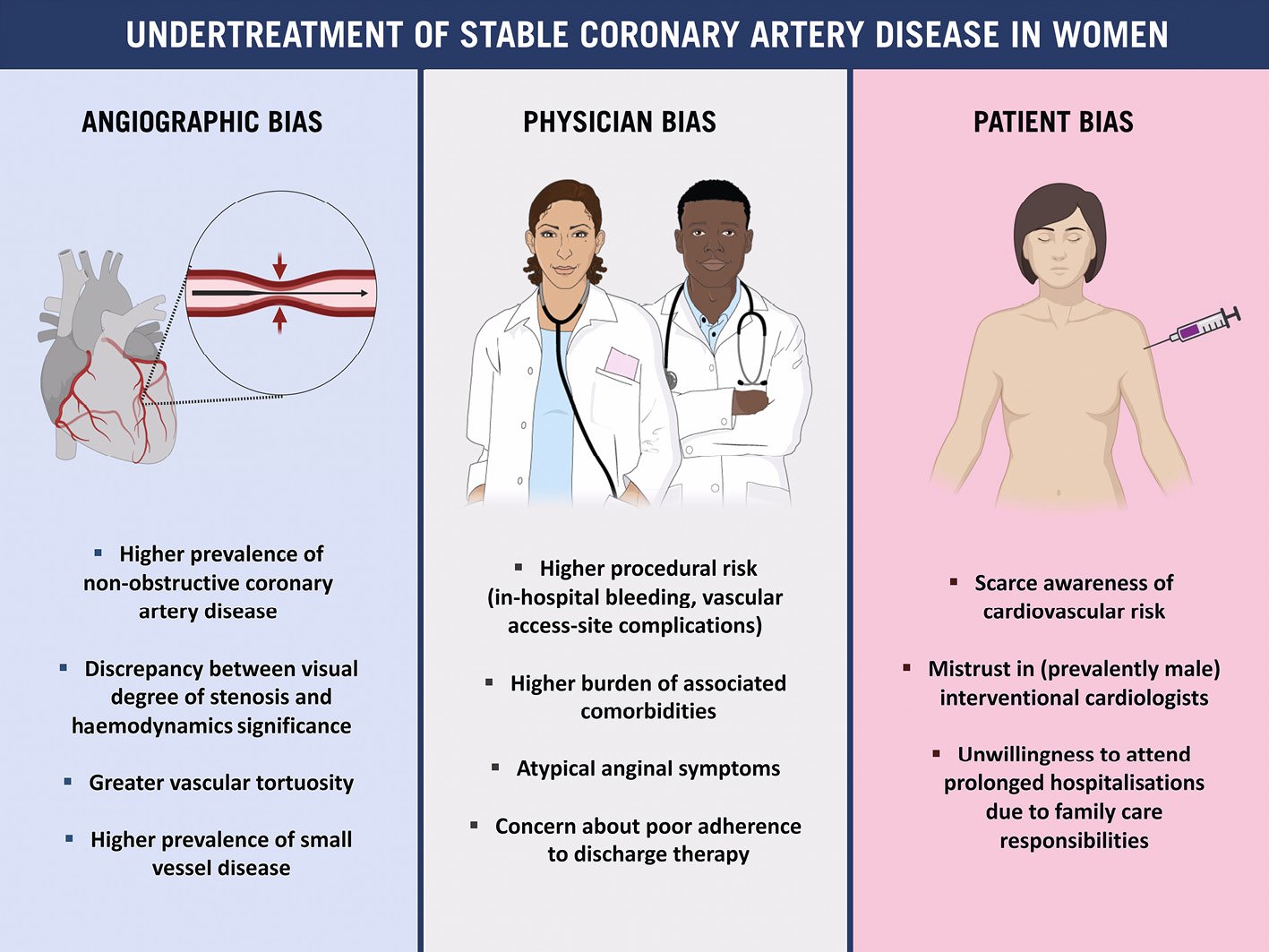
Figure 1. Causes underlying the undertreatment of women with stable coronary artery disease. This figure was created in part from an image provided by Servier Medical Art (https://smart.servier.com), licensed under a Creative Commons Attribution 4.0 License.
Conflict of interest statement
R. Mehran reports institutional research grants from Abbott, Abiomed, Applied Therapeutics, Arena, AstraZeneca, Bayer, Biosensors, Boston Scientific, Bristol-Myers Squibb, Cardiawave, CellAegis, CERC, Chiesi, Concept Medical, CSL Behring, DSI, Insel Gruppe AG, Medtronic, Novartis Pharmaceuticals, OrbusNeich, Philips, Transverse Medical, and Zoll; personal fees from ACC, Boston Scientific, California Institute for Regenerative Medicine (CIRM), Cine-Med Research, Janssen, WebMD, and SCAI; consulting fees paid to the institution from Abbott, Abiomed, AM-Pharma, Alleviant Medical, Bayer, Beth Israel Deaconess, Cardiawave, CeloNova, Chiesi, Concept Medical, DSI, Duke University, Idorsia Pharmaceuticals, Medtronic, Novartis, and Philips; equity <1% in Applied Therapeutics, Elixir Medical, Stel, and ControlRad (spouse); and scientific advisory board for AMA and Biosensors (spouse). M. Gitto has no conflicts of interest to declare.