Cory:
Unlock Your AI Assistant Now!
The tricuspid valve stepped into the spotlight when interventional therapies were first developed and applied specifically to treat tricuspid regurgitation (TR). While surgical strategies were previously known to have a high mortality, more recent analysis showed improved surgical results due to better understanding of risk profiles, novel risk scores, improved perioperative management and minimally invasive techniques123. Further, intermediate- and high-risk patients have been recently treated by interventional valve repair applying tricuspid transcatheter edge-to-edge repair (T-TEER) or transcatheter tricuspid valve replacement (TTVR). Heart Teams rapidly implemented these novel techniques into clinical practice and provided independent risk scores and improved screening protocols4. Furthermore, advances in imaging technologies (three-dimensional echocardiography and four-dimensional computed tomography) allow specific assessment of the tricuspid valve and the underlying pathological mechanisms.
The LEADing problem
The rapid progress in imaging of and therapy for the tricuspid valve propelled the identification of a novel disease entity, lead-related TR5. The PCR Tricuspid Focus Group initiated an expert review including numerous experts in interventional cardiology, cardiac surgery, imaging and electrophysiology to discuss and develop algorithms for the diagnosis and treatment of cardiac implantable electric device (CIED)-related TR6. One of the most important diagnostic questions is the role of the lead itself in the disease progress. Tricuspid regurgitation may be associated with a CIED or related to a CIED (Figure 1). The mechanisms of TR induction in CIED patients are leaflet impingement, leaflet perforation, entanglement in the subvalvular apparatus, fibrosis and scarring, endocarditis, prior lead extraction and/or a high percentage of right ventricular pacing. Importantly, an intensive review of the literature revealed an increase in the incidence of severe tricuspid regurgitation by 4% in CIED patients. This number is worrisome and requires attention by the medical community.
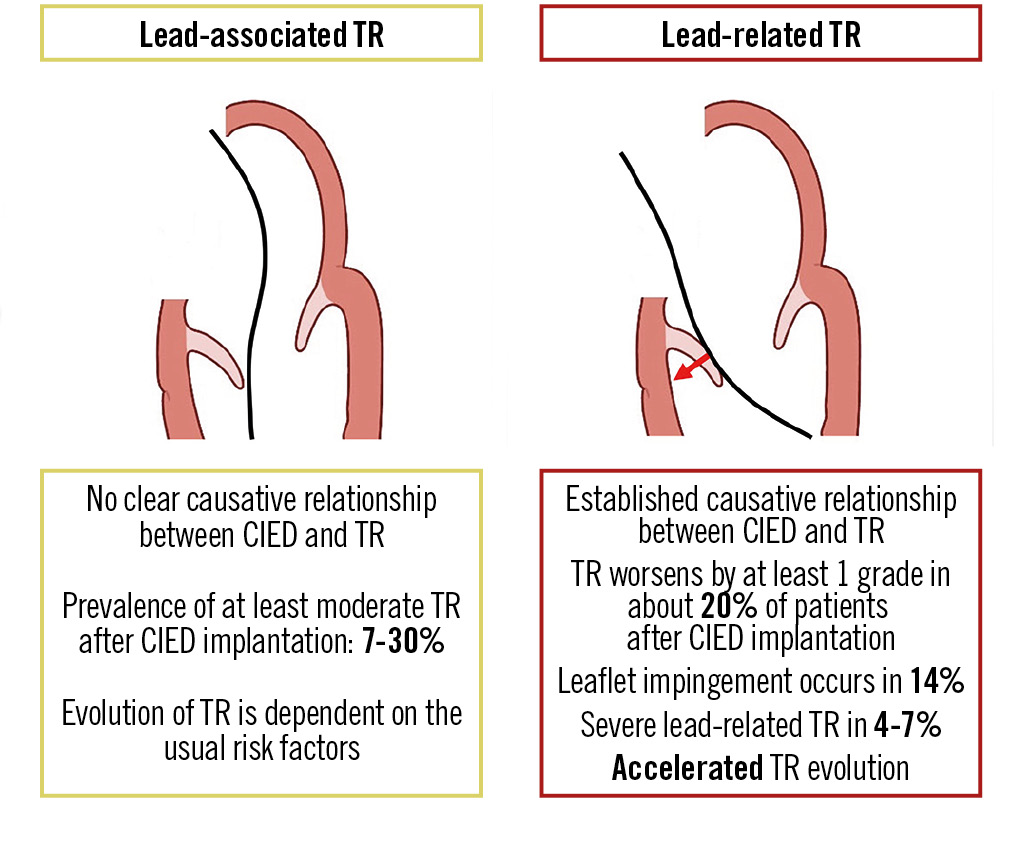
Figure 1. Features of lead-associated and lead-related tricuspid regurgitation. Reproduced from6. CIED: cardiac implantable electronic device; TR: tricuspid regurgitation
Preventing CIED-related TR
The high disease burden and the potential lethal consequences bring prevention of CIED-related TR to the focus of attention. It seems reasonable to perform an echocardiography prior to and early after CIED implantation. Importantly, early detection of TR enables direct surgical revision, thereby, preventing TR perpetuation by annular dilatation. Further, specific implantation techniques, like the prolapsing technique, or systems that avoid the tricuspid valve in high-risk patients are indicated6.
Treating CIED-related TR
While lead extraction may be an option early after CIED placement and in specific cases, risk assessment is important prior to indication, and worsening TR is more common than TR improvement. Hence, T-TEER might be the first-line therapy in intermediate- and high-risk patients with TR and CIED.
In this issue of EuroIntervention, this is underlined by the report of Goebel and colleagues, who present their subanalysis of the bRIGHT EU PAS7. Their results are highly relevant and reveal important knowledge for the treatment of CIED-related TR. The percentage of patients undergoing T-TEER with a CIED was 22%, and up to 80% of these patients suffered from lead-related tricuspid regurgitation. Importantly, treatment success in CIED patients was high and comparable to patients without a CIED, leading to a significant improvement in quality of life. Therefore, it seems likely that the use of T-TEER in patients with CIED-induced TR will significantly increase in the near future, also driven by the increasing interventional expertise with transcatheter tricuspid interventions. Furthermore, CIED patients with a wide coaptation gap or adverse anatomy will more liberally undergo TTVR, for which the understanding of prior CIED implantation during the screening process is rapidly increasing8.
Conclusions
In conclusion, treatment options for patients with CIED-related TR have rapidly improved in the last years. Expert centres with a dedicated Heart Team including electrophysiologist and imaging experts are required. Furthermore, surgical and interventional therapies and perioperative care require specific expertise and training. Optimisation of CIED implantation might reduce TR burden in the future.
Conflict of interest statement
M. Andreas is proctor/consultant/speaker for Edwards Lifesciences, Abbott, Medtronic, Boston Scientific, B. Braun, and Zoll; and received institutional research grants from Edwards Lifesciences, Abbott, Medtronic, and LSI. A. Zirlik is speaker/consultant for Edwards Lifesciences, Abbott, Medtronic, and Boston Scientific; and received institutional educational grants from Edwards Lifesciences. P.E. Bartko reports educational grants from Edwards Lifesciences and Abbott.

