Cory:
Unlock Your AI Assistant Now!
Intravascular brachytherapy (IVBT) was implemented in clinical practice in late 1990s, before the advent of drug-eluting stents (DES). The rationale for its use was the ability of radiation therapy to treat proliferative benign processes such as exuberant keloid scar formation or ocular pterygia, among others12. In-stent restenosis (ISR) was considered a prime target for IVBT, as it is mainly induced by an excess of neointimal proliferation. In this context, IVBT demonstrated an outstanding reduction in the rate of repeat revascularisation345. However, several limitations offset its initial benefit, such as late thrombosis, edge effect and late catch-up phenomenon6789. Further, the logistics and the regulatory process to implement IVBT in the cath lab were cumbersome, limiting its widespread adoption. Eventually, the subsequent development of DES sidelined the technique in most cath labs around the world.
In this issue of EuroIntervention, Tanner et al report the 3-year outcomes of patients with multilayer drug-eluting ISR treated with IVBT10. This was an observational retrospective study that comprised patients treated with and without IVBT between 2012 and 2019. From a total of 647 patients with multilayer ISR, 453 (70%) were treated with IVBT. After propensity-matched adjusted analysis, the rate of major adverse clinical events was significantly lower in patients treated with IVBT at 3 years, compared to those without. The results of this study must be considered within the context of several limitations. First, statistical adjustments cannot correct for the inherent bias regarding treatment selection, which remained entirely at the treating physician’s discretion. Further, none of the patients received drug-coated balloons (DCBs), which are the current standard of care outside the US. Finally, data on dual antiplatelet therapy regimens received and very late stent thrombosis rates are lacking. Despite these limitations, the results of the study are relevant. They highlight an unmet clinical need regarding the treatment of recurrent events after stent implantation.
Several metal-free strategies have been implemented to treat or prevent stent-related events (Figure 1). Plain balloon angioplasty was the first option to treat ISR. However, its results were surpassed by those of additional DES implantation, IVBT and recently, DCBs. Growing evidence supports the use of DCBs. Paclitaxel-eluting balloons have demonstrated efficacy in treating ISR. Furthermore, they have shown potential for treating de novo lesions in small vessels and side branches in true bifurcations. The use of DCBs in large de novo lesions is under investigation. This metal-free technology cannot be granted any class effect, and each DCB must show their own evidence. Polymer-based bioresorbable scaffolds were designed to avoid permanent metallic prostheses and restore coronary vasomotion. However, the results of randomised trials have shown an increase in late thrombotic events and a lack of effect on vasomotion. Currently, magnesium-based bioresorbable scaffolds with a potentially safer profile are being tested in a pivotal trial involving de novo coronary lesions. Multilayer ISR might represent the last remaining niche for IVBT in dedicated centres. However, given the complex logistics and the lack of global interest from industry and the medical community in designing large, randomised trials addressing this issue, a revival of this technique in the next years is unlikely.
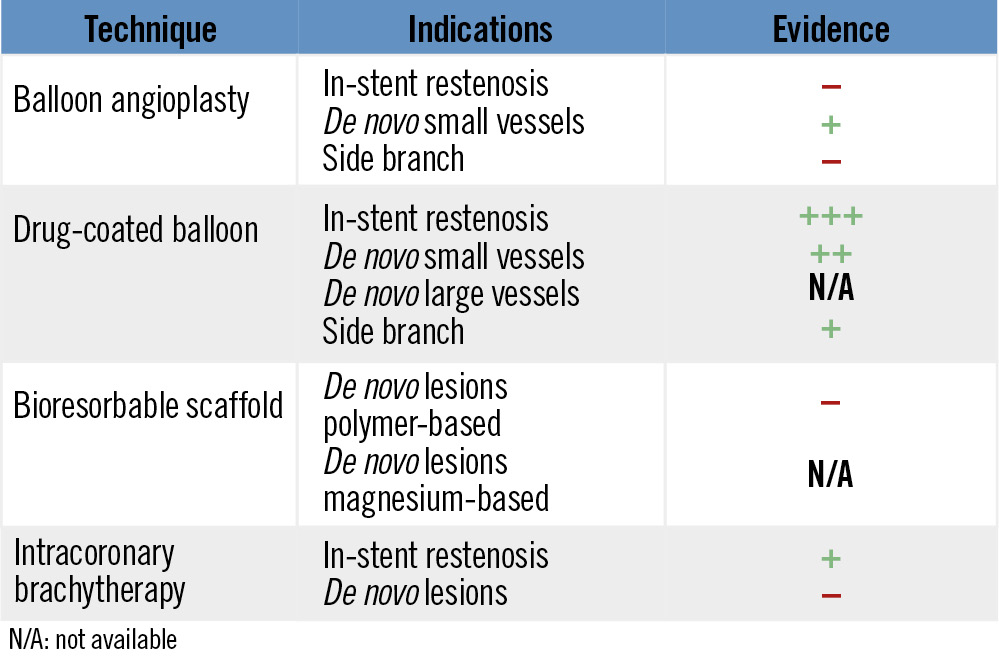
Figure 1. Metal-free strategies in interventional cardiology. N/A: not available
Conflict of interest statement
M. Sabaté reports consulting fees from iVascular and Abbott.