Cory:
Unlock Your AI Assistant Now!
Structural deterioration of bioprosthetic heart valves, manifesting as stenosis and/or regurgitation, remains the primary factor limiting valve longevity. As patients undergoing valve replacement have increasingly longer life expectancies, planning lifelong management is essential1. This trend also highlights the need to balance surgical and transcatheter options in redo procedures, which is an evolving conversation in which transcatheter options may offer a less invasive alternative to surgery2. Here, we report a challenging case in the lifelong management of aortic valve disease of a 66-year-old female with significant comorbidities, including chronic kidney disease, end-stage liver disease, and a complex cardiac history.
The patient was initially treated at the age of 47 due to native aortic valve endocarditis, necessitating surgical aortic valve replacement (SAVR) with a 21 mm Carpentier-Edwards PERIMOUNT (Edwards Lifesciences). The procedure involved root enlargement and congenital ventricular septal defect repair, complicated by coagulopathy, leading to a prolonged hospital stay but a favourable overall outcome. Nine years later, at age 56, she underwent a transcatheter aortic valve-in-surgical aortic valve (TAV-in-SAV) procedure, owing to the risk of coronary obstruction and sinus sequestration secondary to high-risk root features (Figure 1A-Figure 1B-Figure 1C), with a 20 mm SAPIEN XT valve (Edwards Lifesciences) for a failed surgical bioprosthetic valve, utilising a standby “protected” left main approach. A decade later, at 66, she presented with symptoms of congestive heart failure due to severe transvalvular bioprosthetic regurgitation (ejection fraction [EF] 60%, mean gradient [MG] 29 mmHg) (Moving image 1, Figure 1F, Figure 1G). Given her comorbidities, the surgical risk was deemed exceedingly high. Moreover, computed tomography revealed a significant risk of coronary obstruction and/or sinus sequestration, and available transcatheter leaflet modification techniques were deemed insufficient to ensure coronary protection (Figure 1D, Figure 1E, Moving image 2). Consequently, it was decided to proceed with high-risk SAVR, using a 23 mm INSPIRIS RESILIA valve (Edwards Lifesciences) due to its expandable stent frame, potentially facilitating a future TAV-in-SAV procedure. The initially planned mini-sternotomy approach was converted to full sternotomy secondary to an iatrogenic aortic haematoma, resulting in an extended hospital stay but ultimately a good recovery. At the three-month follow-up, the patient was clinically well, with good function of the bioprosthetic aortic valve on transthoracic echocardiography (EF 60%, MG 9mmHg, no paravalvular regurgitation) and no hospitalisations (Figure 1H, Figure 1I).
This case highlights the real-world challenges in the lifelong management of aortic valve disease. The importance of optimising aortic valve implantation during the index procedure must be recognised to enhance redo options. Additionally, improvements in leaflet modification techniques and devices as well as consideration of potential changes in valve platforms are essential steps in facilitating valve-in-valve procedures and improving lifelong management outcomes.
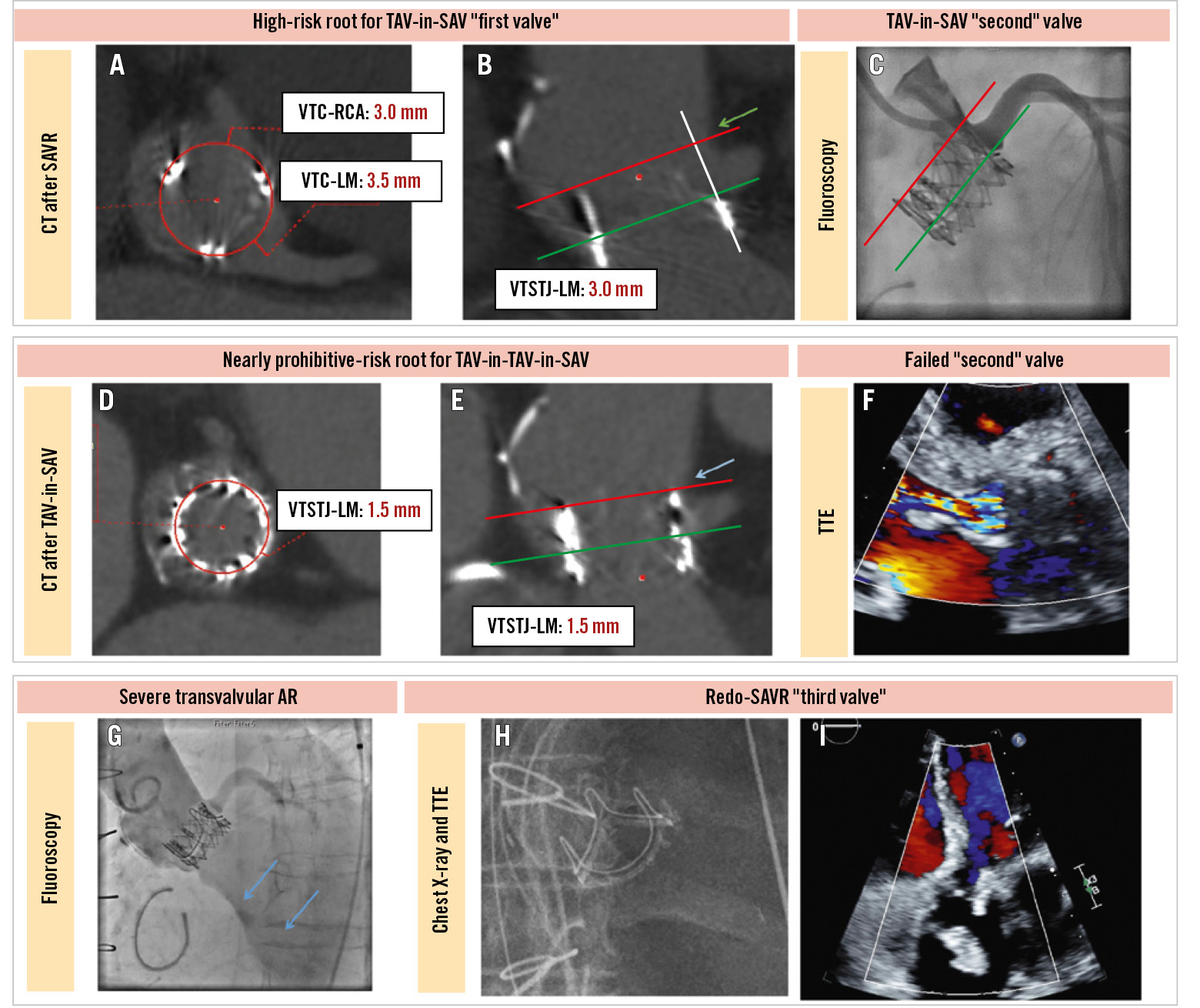
Figure 1. Management of bioprosthetic valve failure at 10 years after TAV-in-SAV. Borderline VTC-LM and VTSTJ-LM distances for TAV-in-SAV (A,B). SCA after TAV-in-SAV (C), utilising a protected LM approach demonstrates TIMI III flow in the LM. Green lines mark the coronary risk plane; red lines mark the stent posts of the SAV and TAV-in-SAV extending to the reconstructed STJ on the neo-LCC side.The green arrow points to the almost inexistent reconstructed STJ on the neo-LCC side following aortic root enlargement. The VTSTJ-LM distance after TAV-in-SAV in short-axis (D) and long-axis (E) views indicates a significant risk for sinus sequestration on the neo-LCC side. The red line shows the TAV-in-SAV frame extending to the reconstructed STJ on the neo-LCC side. Note the unusual anatomy of the aortic root following aortic root enlargement, with the green arrow pointing to an almost inexistent reconstructed STJ on the neo-LCC side. TTE (F) reveals a failed bioprosthetic aortic valve 10 years after TAV-in-SAV, showing severe transvalvular regurgitation. The aortic root angiogram (G) indicates severe aortic regurgitation, consistent with the TTE findings (blue arrows). The chest X-ray (H), taken after redo-SAVR, demonstrates the SAV frame. TTE (I) confirms good function of the SAV without evidence of paravalvular leak. AR: aortic regurgitation; CT: computed tomography; LCC: left coronary cusp; LM: left main; RCA: right coronary artery; SAV: surgical aortic valve; SAVR: surgical aortic valve replacement; SCA: selective coronary angiogram; STJ: sinotubular junction; TAV: transcatheter aortic valve; TIMI: Thrombolysis in Myocardial Infarction; TTE: transthoracic echocardiography; VTC: virtual valve-to-coronary; VTSTJ-LM: virtual valve-to-STJ-to-LM
Conflict of interest statement
D.A. Wood is a consultant to and has received research funding from Edwards Lifesciences and Abbott. J.G. Webb is a consultant for Edwards Lifesciences; and receives research funding from Edwards Lifesciences, Medtronic, and Boston Scientific. J. Jelisejevas has no relevant conflicts of interest to declare.
Supplementary data
To read the full content of this article, please download the PDF.
Moving image 1. Severe AR. Aortic root angiogram shows low reconstructed STJ height on the neo-LCC side, along with low LM height and severe transvalvular regurgitation 10 years after TAV-in-SAV.
Moving image 2. Annulus batch. TAV-in-SAV annulus batch demonstrates a high risk of sinus sequestration on the neo-LCC side, with the LM arising at 5 o’clock, secondary to an almost inexistent reconstructed STJ following aortic root enlargement.