To paraphrase Homer’s Odyssey, Book XII (c. 750 BCE), we are “steering between the Scylla of too-much and the Charybdis of not-enough”.
Since the first coronary artery balloon angioplasty by Andreas Grüntzig in 1977 and during the subsequent introduction of bare metal stents (BMS) in 1986 and drug-eluting stents (DES) in 1999, the Achilles’ heel of percutaneous coronary interventions (PCI) has been the delicate balance between increased risk of restenosis and increased risk of early and late stent thrombosis as well as the risk of bleeding due to the antiplatelet treatment required1. The introduction of BMS reduced the abrupt vessel closure after plain old balloon angioplasty by sealing the dissections and covering the ruptured plaques, but this introduced a risk of early stent thrombosis and a high rate of late in-stent restenosis1. DES have consistently reduced the risk of restenosis by the elution of antiproliferative drugs, but this benefit has come with the price of an increased and prolonged risk of stent thrombosis, probably due to delayed healing and re-endothelialisation of the stent struts12. This observed persistence of late events after both first- and second-generation permanent-polymer DES has driven the development of new stent designs with thinner struts, biodegradable polymers and the latest non-polymeric drug-eluting stents23 to increase stent re-endothelialisation and preferably lower the bleeding risk by reducing the intensity and the duration of antiplatelet therapy34. This strategy, however, has led to an increased risk of restenosis and subsequent target lesion revascularisation (TLR) as seen in the latest trials in the field evaluating the efficacy and safety of polymer-free drug-eluting stents23. The progress so far has reduced the risk of stent failure1, but the equipoise between risk of restenosis and risk of stent thrombosis has not yet been clearly identified.
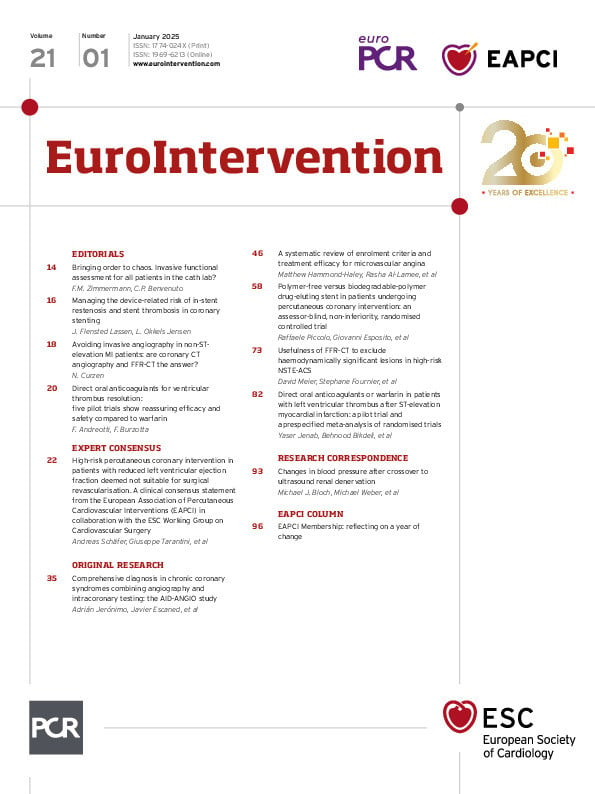
In this issue of EuroIntervention, Piccolo and colleagues present the latest study in this field addressing the balance between restenosis, stent thrombosis and antiplatelet therapy: the PARTHENOPE trial4, a randomised, non-inferiority trial comparing a polymer-free amphilimus (sirolimus)-eluting stent (AES) with a biodegradable-poymer everolimus-eluting stent (EES). The study elegantly addresses both the bleeding risk (duration of antiplatelet therapy) and the restenosis risk associated with the two devices. Two independent hypotheses were tested in a 2-by-2 factorial design: (1) the non-inferiority of the AES versus the EES at 1 year and (2) the superiority of a personalised duration of dual antiplatelet therapy (DAPT) versus standard DAPT for 12 months at 2-year follow-up2. In this issue, the authors present the primary endpoint (a device-oriented composite endpoint, consisting of cardiovascular death, target vessel myocardial infarction, or TLR). At 1 year, the endpoint was reached in 8.2% of patients assigned to AES and 7.2% of patients assigned to EES and, thus, met the non-inferiority criteria, but the result came with a price of significantly more definite and probable stent thrombosis among patients assigned to the polymer-free AES (1% vs 0.3%, hazard ratio 3.72; p=0.044). These results are in line with previous studies, but in this study, there is not a huge difference in the restenosis rate between a biodegradable-polymer stent and a polymer-free stent, leaving us with the remaining question of whether the increased risk of stent thrombosis can be reduced by individualised antiplatelet therapy. We may come closer to an answer on this when the PARTHENOPE trial presents the 2-year results of individualised antiplatelet therapy compared to standard care4.
In conclusion, the last four decades of continuous refinement of PCI and stent design and subsequent evaluation of the need for antiplatelet therapy have reduced stent thrombosis, restenosis and risk of bleeding to a level where the risk of stent failure is low. We have come a long way since the first angioplasty was performed by Andreas Grüntzig in 1977. There is, however, still a major clinical need for more personalised medicine and further studies of the delicate balance between the risk of restenosis and the risk of thrombosis and bleeding. The journey continues.
Conflict of interest statement
J.F. Lassen reports speakers honoraria for lectures from Medtronic, Abbott and Boston Scientific. L. Okkels Jensen reports unrestricted research grants to her institution from Biotronik, Biosensors and OrbusNeich.