Cory:
Unlock Your AI Assistant Now!
The human heart possesses a complex innervation system of sympathetic and parasympathetic nerves mainly involved in regulating coronary blood flow, myocardial contractility, and overall cardiac function. The first systematic approach to understand the autonomic innervation of the human heart dates back to 1926, when Woollard and colleagues described the abundant autonomic innervation of the coronary circulation, emphasising its relevance for cardiac physiology1. In humans, it is known that proximal epicardial coronary arteries (internal diameter 0.8-2.0 mm) exhibit a relatively sparse distribution of nerve fibres, forming a loose network in the adventitia and at the adventitia-media border. Most nerve fibres represent sympathetic nerves, with only few parasympathetic and sensory nerves. In the distal coronary arteries (internal diameter <0.8 mm), nerve fibres are more densely distributed, and the number of sympathetic nerves increases with declining vessel diameter, while parasympathetic nerves remain sparsely distributed even in smaller-sized arteries.
In the current issue of EuroIntervention, Tokcan and colleagues aimed to quantitatively map the periarterial innervation of human coronary arteries to gain further insights into the detailed anatomy of their autonomic innervation2. They examined a total of 100 coronary arteries from 28 human body donors, which led to the characterisation of overall nerve distribution, identification of sympathetic nerve fibres and delineation of their spatial relationship to the major coronary arteries. Their findings confirmed earlier studies that found a decrease in nerve diameter and an increase in relative nerve density along the proximal-distal axis1. Through their meticulous work, they were able to further show that innervation patterns differ not only among major coronary arteries but also between the epicardial and myocardial localisation. While nerve density was highest along the right coronary artery (RCA) and lowest along the left anterior descending artery (LAD), nerve size was greatest along the left main coronary artery (LMCA), followed by the LAD, RCA and left circumflex artery (LCx). Interestingly, while nerve fibres were generally closest to the lumen along the LMCA and farthest from the lumen along the RCA, the distance from the nerve fibres to the lumen decreased along the proximal-distal axis for the LAD and RCA, while it increased for the LCx, which is opposite to observations made in renal arteries34. Concerning the epicardial area, nerves were larger and located closer to the lumen, whereas the myocardial area had a higher nerve density.
What does this insightful examination tell us, and how can we put this into perspective for the community of interventional cardiologists? As the coronary circulation is responsible for the determination of myocardial perfusion, its dysregulation may be highly relevant in the setting of microvascular dysfunction, where the functionality of small-sized coronary arteries is dependent on a multitude of humoral and neural impulses. One specific example might be the recently introduced concept of ischaemia with non-obstructive coronary arteries (INOCA), where abnormal vasoconstriction and/or impaired vasodilation of small-sized coronary arteries result in insufficient oxygen supply to the downstream myocardium leading to symptoms like angina and shortness of breath. Although this novel disease condition may be secondary to different underlying aetiological factors such as left ventricular hypertrophy, diabetes and many others, neural regulation of the microvasculature may be considered the key effector in its pathophysiology.
Another important finding in clinical practice relates to the occurrence of vasospasm of the major coronary arteries and its clinical manifestation of non-exertional angina. From clinical experience, vasospasm is frequently observed in younger patients and in response to emotional triggers567. Against this background, Tokcan and colleagues described abundant autonomic nerve density along the coronary arteries, suggesting a possible causal relationship. It is conceivable that emotional triggers might cause an exaggerated contractile response of smooth muscle cells within the media of the arteries resulting in abnormal vasoconstriction.
Another important disease state likely to be influenced by autonomic innervation is atherosclerosis and its different manifestations. In a recently published landmark study, Mohanta and colleagues were able to provide a scientific fundament for the observation of important neuroimmune interactions during the onset and progression of atherosclerosis8. Although atherosclerotic plaques are not directly innervated by nerve fibres, the authors were able to delineate increased axonal endings in distinct regions of the adventitia within atherosclerotic lesions, suggesting direct neural communication via artery-associated tertiary lymphoid organs (ATLOs). Since inflammation remains a well-established determinant of atherosclerotic lesions, the possibility of regulating periplaque inflammation via ATLOs represents an attractive explanation for the widely believed interaction between neural stimulation such as stress and anxiety and the rapid progression and clinical manifestation of atherosclerosis. Importantly, the authors were also able to demonstrate that mechanical or chemical disruption of this neuroimmune communication resulted in decreased atherosclerotic plaque size in apolipoprotein (apo) E-deficient mice. This study, for the first time, provided solid evidence for another so far under-recognised pillar related to the progression of atherosclerosis, which might open new avenues for diagnostic and therapeutic pathways (Figure 1).
The authors of the current manuscript need to be congratulated for providing further details concerning the anatomy of human autonomic nerve distribution along the coronary arteries and drawing our attention to a potentially ground-breaking ECG: electrocardiogram; INOCA: ischaemia with non-obstructive coronary arteries. Created with BioRender.com. association between neural innervation of the heart and various cardiac disease conditions. Future studies will need to focus on confirming these findings, given the large heterogeneity of sympathetic nerve distribution amongst individuals, and providing proof-of-principle that modulation of the autonomic innervation may impact the clinical course of our patients.
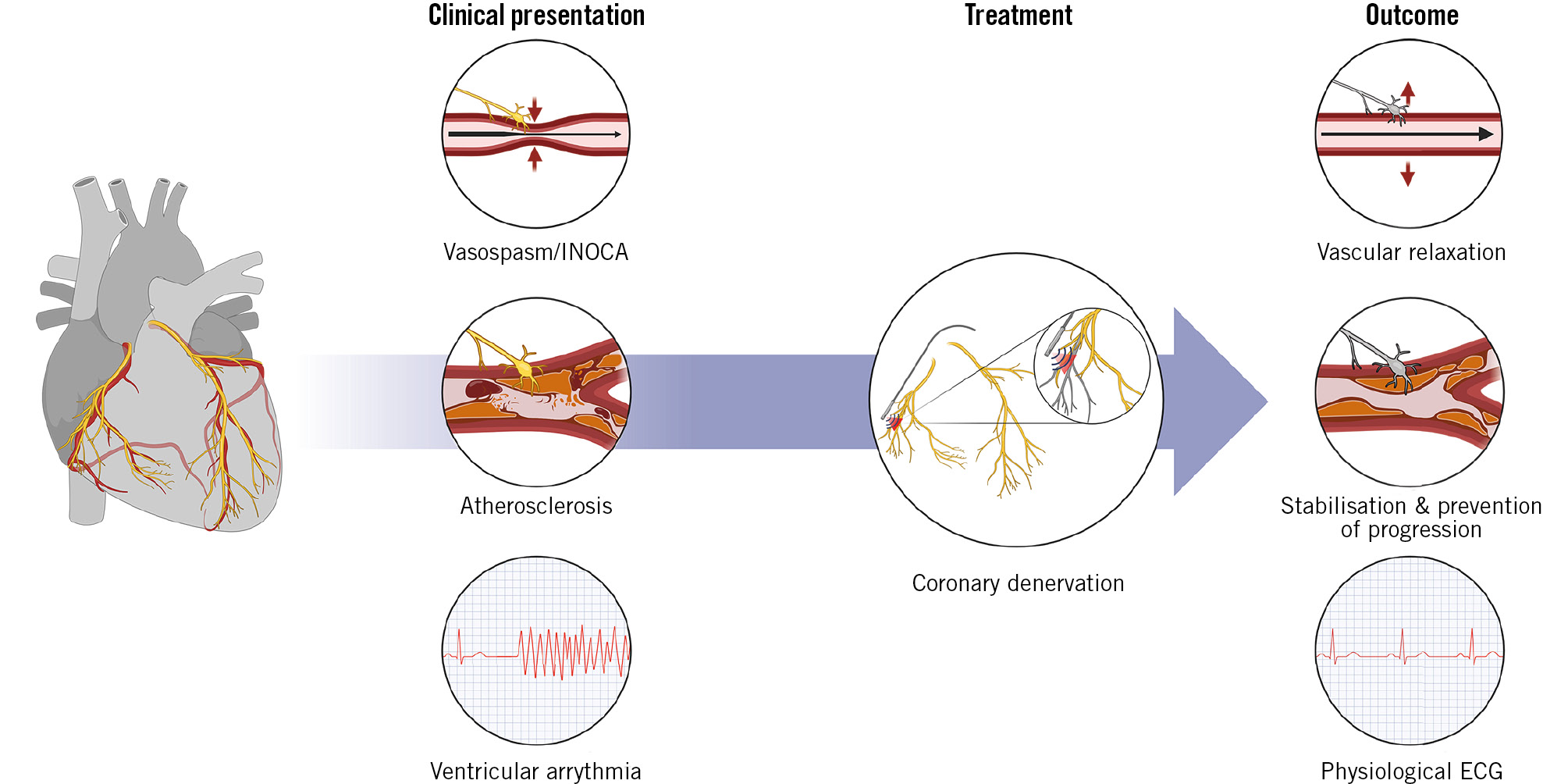
Figure 1. Potential application of coronary artery denervation. ECG: electrocardiogram; INOCA: ischaemia with non-obstructive coronary arteries. Created with BioRender.com.
Conflict of interest statement
M. Joner reports personal fees from AstraZeneca and ReCor Medical; and grants and personal fees from Biotronik, Boston Scientific, and Edwards Lifesciences outside the submitted work; he has received funding from the German Centre for Cardiovascular Research: DZHK (FKZ 81Z0600502; FKZ 81X2600526), and from the Leducq Foundation (grant agreement number: 18CVD02). A. Beele has no conflicts of interest to declare.