Cory:
Unlock Your AI Assistant Now!
Patients with renovascular hypertension are at increased risk of cardiovascular events compared with the general population1. Several surgical and endovascular renal artery (RA) revascularisation options are available and have demonstrated improvement in blood pressure control for those with atherosclerotic RA stenosis, although the data have been mixed in other populations2. At present, RA stenting is infrequently utilised, likely based on conflicting data (several negative randomised control trials, but multiple positive observational studies and single-arm cohort trials)2. Few contemporary, large-scale studies have evaluated trends in this procedure in the United States or evaluated related events. Our objectives for this study were as follows: 1) to determine recent temporal trends of RA stenting in the USA, and 2) to describe cardiovascular and renal event rates among patients with severe renovascular hypertension requiring stenting.
We included all Medicare fee-for-service beneficiaries >65 years who underwent RA stent placement between 1 January 2016 and 31 December 2020. Subjects were identified in the Centers for Medicare and Medicaid Services’ (CMS) Medicare coverage database using procedural billing codes to identify inpatient and outpatient procedures. Patient demographics were ascertained at the time of index procedure from the chronic conditions file which uses algorithms to search the CMS database for 67 comorbidities. The primary outcomes were annual procedural utilisation and cardiovascular events (composite of stroke, myocardial infarction, and congestive heart failure hospitalisation). Secondary outcomes included repeat RA stenting, dialysis initiation, hospital admission for hypertensive crisis and all-cause mortality. Events were assessed annually after the index procedure. Survival methods were applied to estimate the cumulative incidence of events, taking into account the competing risk of death. For all-cause mortality, traditional Kaplan-Meier estimates of the cumulative incidence of death at each time point were reported. Statistical analyses were performed using SAS 9.4 statistical software (SAS Institute). A p-value<0.05 was considered statistically significant.
Of 31,359 subjects included, 55.7% were female, 6.6% were Black, and the mean age was 75.7±6.4 years. Among these, 75.9% had chronic kidney disease, 98.2% had hypertension, 80.9% had ischaemic heart disease, 70.1% had atherosclerotic RA disease, and 1.2% had fibromuscular dysplasia. The rate of RA stenting decreased annually during the study period from 27.3 per 100,000 Medicare beneficiaries to 15.9 per 100,000 Medicare beneficiaries (Central illustration). In this population, cardiovascular events occurred in 21.3% up to 1 year and in 46.1% up to 5 years. Repeat RA stenting occurred in 4.6% up to 1 year and 9.5% up to 5 years. Dialysis initiation occurred in 2.1% up to 1 year and 5.6% up to 5 years. Hospital admission for hypertensive crisis occurred in 4.6% up to 1 year and 13.4% up to 5 years. All-cause mortality was 8.3% up to 1 year and 37.6% up to 5 years.
This nationwide analysis of Medicare beneficiaries found that the annual incidence of RA stenting has decreased over the past several years and that these patients represent a high-risk group, with more than 1 in 5 experiencing a cardiovascular event by 1 year. Earlier studies have demonstrated a similar trend of decreasing RA interventions, likely attributable to uncertainty regarding the clinical efficacy of RA stenting3. Using RA stent placement as a proxy for disease severity, it is clear that these patients are at very high risk of morbidity and mortality with an almost 40% 5-year all-cause mortality rate, though, interestingly, the rate of adverse renal events was relatively low. Adverse event rates in this population were far higher than those described in the CORAL study which had reported just 15% all-cause mortality and 19% cardiovascular event rates by 3.5 years4. Our findings question the generalisability of some of the larger RA stenting trials given the substantial differences between population event rates. Patients with renovascular hypertension that is severe enough to have RA stenting should be considered for all potential treatments to reduce the risk of morbidity and mortality. This aligns with a recent American Heart Association (AHA) scientific statement endorsing the importance of renal revascularisation for high-risk populations5. These findings are not necessarily an endorsement for RA stenting but should draw attention to the significant morbidity within this population and the need for further investigation into therapies targeted for this high-risk group.
The limitations of our study include the use of administrative data, which can be subject to misclassification; lack of a control group (so event rates cannot be compared to medically managed patients); unavailability of follow-up creatine and blood pressure measures; and unavailability of medication information; thus, conclusions cannot be drawn about changes in antihypertensive medications following RA stenting.
Here we describe a declining rate of RA interventions in a population with severe renovascular hypertension and high morbidity and mortality. While continued use of RA revascularÂisation procedures may be important for treating high-risk populations, further investigation is needed. Future investigations should include populations with a higher burden of cardiovascular disease than prior studies to better assess the efficacy of therapies which utilise medications with or without revascularisation procedures.
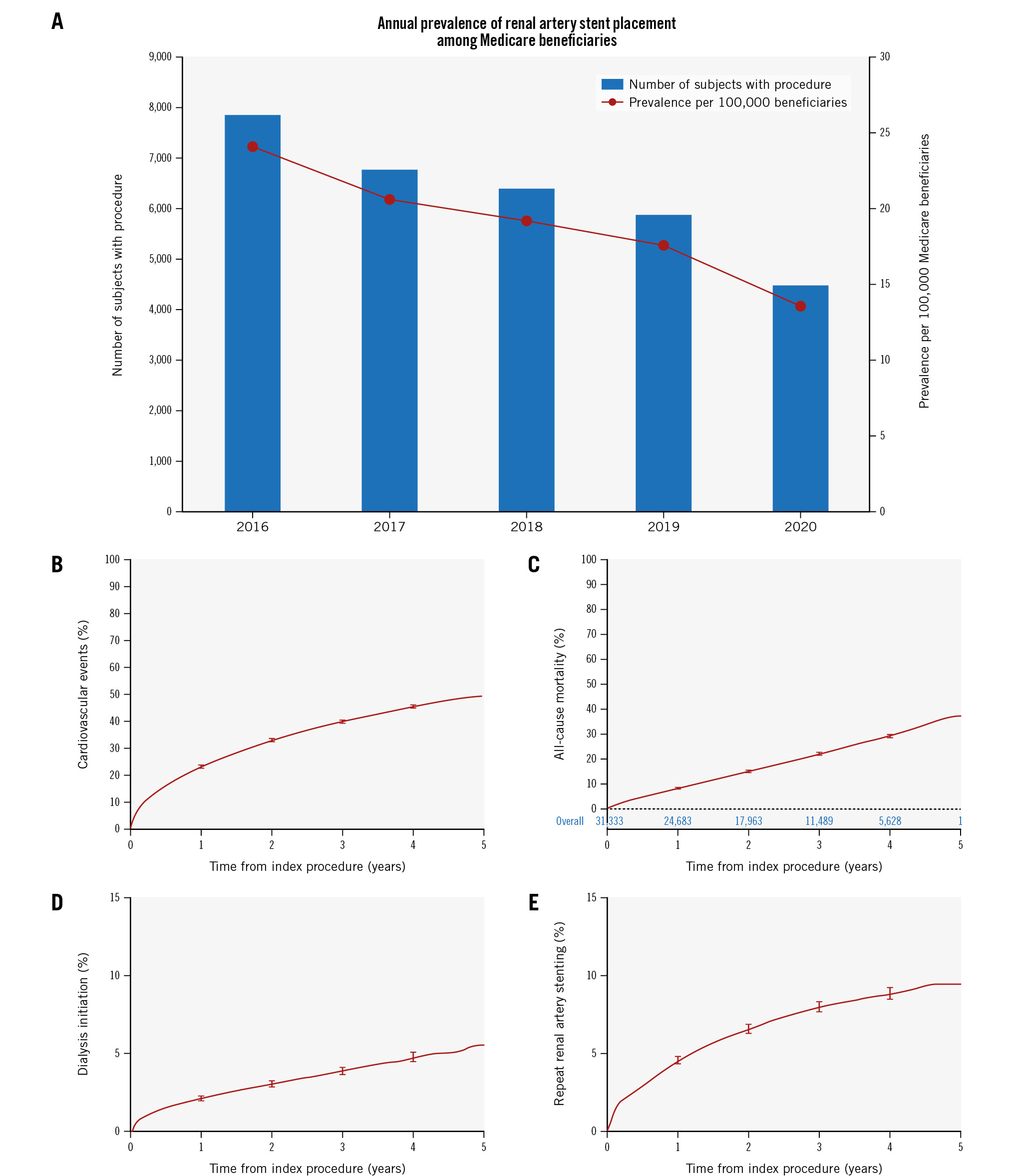
Central illustration. Renal artery stenting: annual prevalence and event rates. A) Annual prevalence of renal artery stent placement. The remaining graphs show the cumulative incidence of adverse events per year from index procedure: B) cardiovascular events (composite of hospitalisation for stroke, congestive heart failure and myocardial infarction); C) all-cause mortality; D) dialysis initiation; E) repeat renal artery stenting.
Conflict of interest statement
E.A. Secemsky is supported in part by NIH/NHLBI grant K23HL150290; and receives consulting fees from Abbott, Bayer, BD, Boston Scientific, Cook Medical, CSI, Medtronic, Philips, Shockwave Medical, and VentureMed. S.P. Juraschek is supported in part by NIH/NHLBI grant R01HL153191. M.L. Schermerhorn receives consulting fees from Abbott and Medtronic. H.D. Aronow participates on an advisory board for Philips. The other authors have no conflicts of interest to declare relevant to the contents of this paper.