Drug-coated balloon (DCB)-only angioplasty is a rapidly expanding area of both clinical interest and research in the field of coronary intervention. Randomised clinical trials (RCTs) and registries have shown the non-inferiority of DCB-only percutaneous coronary intervention (PCI), as compared with routine, standard-of-care drug-eluting stent (DES) implantation, in a number of clinical settings and lesion types. However, the most high-risk and possibly most complex angioplasty that is often done is in the setting of an acute coronary syndrome (ACS), particularly ST-elevation myocardial infarction (STEMI) primary PCI (PPCI) or out-of-hospital cardiac arrest (OOHCA) (Figure 1). There are limited data available for the use of DCBs in the setting of an ACS; we will review this along with the potential advantages and disadvantages of adopting a DCB approach.
There are a large number of case reports on the use of DCBs in ACS patients, as well as data from RCTs including subgroup analyses. The first studies, such as PAPPA or DEB-AMI, investigated the concept of combining DCBs with bare metal stents (BMS), a concept that has largely been abandoned today. The randomised PEPCAD NSTEMI trial showed non-inferiority with a DCB-only approach versus primary stent implantation (BMS or DES). During a follow-up of 9.2±0.7 months, DCB treatment was non-inferior to stent treatment, with a target lesion failure rate of 3.8% versus 6.6%. There was no significant difference between BMS and current-generation DES. The total major adverse cardiac event (MACE) rate was 6.7% for DCB treatment versus 14.2% for stent treatment (p=0.11), and 5.9% versus 14.4% in the per-protocol analysis (p=0.056), respectively1. For STEMI patients, a large propensity-matched cohort study in 1,139 patients also found non-inferiority during 3 years of follow-up compared with a cohort with standard-of-care DES implantation. There was no difference in mortality between DCBs and DES (10.8% vs 9.0%)2. The REVELATION RCT showed that a DCB-only strategy was non-inferior to DES in STEMI patients in terms of fractional flow reserve assessed at 9 months, with a mean fractional flow reserve of 0.92±0.05 in the DCB group and 0.91±0.06 in the DES group3. In a prespecified analysis of the BASKET-SMALL 2 RCT, a significant interaction between clinical presentation and treatment was seen at 1 year for cardiac death and non-fatal myocardial infarction, with lower rates in patients with ACS treated with DCBs. At 3 years, there were similar rates of MACE and all-cause mortality between DCBs and DES, irrespective of clinical presentation, but these were higher in patients with ACS compared with chronic coronary syndrome4.
The potential advantages of a DCB-only approach for any PCI will obviously apply in the setting of ACS. Firstly, a DCB-only strategy allows for simplification of the procedure, which may be very attractive in acutely unwell and possibly haemodynamically unstable patients. There is also the late advantage of endothelial healing, subsequent return of vasomotor function and late luminal enlargement. Very late stent failure rates will obviously be mitigated with no permanent implant, and current data suggest a lower long-term (5-10 year) event rate with a DCB-only approach.
Other possible advantages include that an extra, potentially thrombogenic, substrate is not required to be implanted into the artery (which obviously occurs with DES or scaffold deployment). In the setting of acutely unwell patients, dual antiplatelet therapy (DAPT) absorption may be impeded, particularly in those presenting with an OOHCA or very large thrombus burden. In the OOHCA group, the early stent thrombosis rate is high, and a DCB-only (or indeed balloon-only) approach to improve coronary flow and stabilise the patient may be sufficient in the short term. Similarly, in cases with a large thrombus burden, restoring flow whilst avoiding distal embolisation, and thus no-reflow, is appealing. An extrapolation of the DCB-only approach in these patients could be thrombectomy, when appropriate, flow restoration with minimal angioplasty, and then aggressive DAPT and glycoprotein IIb/IIIa therapy with an early staged, and hopefully much more simplified, completion of the PCI a few days later. High bleeding risk is always an issue in PCI patients and may be more difficult in the acute setting due to less prior knowledge of patient compliance, planned urgent prognostic surgery, bleeding problems and post-myocardial infarction complications, such as the development of atrial fibrillation or left ventricular thrombus formation. All of these concerns can be mitigated to some degree with the increased flexibility of a DCB-only approach.
Vessel sizing is always of concern in the setting of PPCI, and a DCB-only approach is perhaps slightly more forgiving bearing in mind the suggested vessel sizing of between 0.8 and 1.0 based on angiography. DES implantation, however, requires perfection as judged by both angiography and intravascular imaging, which in the setting of sick patients with considerable vasoconstriction and possible thrombus may be more difficult. There is a theoretical concern of increased distal embolisation during stent deployment and post-dilation optimisation, which may result in a higher incidence of no-reflow and a worse long-term outcome. The role of stenting in cases of plaque erosion is minimal luminal encroachment after resolution of the thrombus, and flow restoration is an area of research and debate; a DCB-only approach may be more appropriate in this setting if any PCI is required.
Potential disadvantages of a DCB-only approach include the relative paucity of data available, as outlined above. There are theoretical issues related to distal embolisation during DCB delivery which may exacerbate the no-reflow phenomenon in ACS PCI, and perhaps this should be considered in future RCTs comparing DCBs and DES in PPCI. However, the risk of thrombus embolisation caused by stent implantation may be much higher. A more likely disadvantage is the operator experience and the anxiety related to treating such patients, in whom flow is of paramount importance and vessel preparation can be difficult. In ACS cases, an optimal balloon angioplasty result is required without vessel threatening dissection or luminal compromise, but may be more challenging to achieve or accept for those operators more comfortable with DES results.
In conclusion, we have outlined the current data and our opinions on the use of DCB-only PCI in the setting of ACS. We acknowledge more data will be of benefit, but we currently see a role for DCB-only PCI in these complex patients and complex lesions.
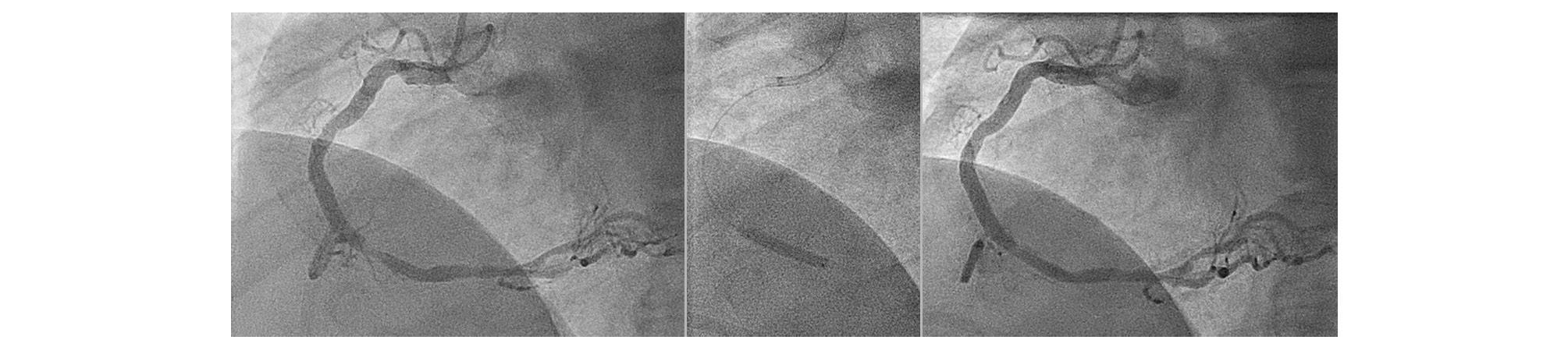
Figure 1. Thrombotic lesion in a right coronary artery in a patient after out-of-hospital cardiac arrest (OOHCA) and resuscitation. Lesion preparation with a scoring balloon followed by a 3.5x20 mm paclitaxel-coated balloon.
Conflict of interest statement
B. Scheller is a shareholder of InnoRa GmbH and received lecture fees and consulting honoraria from B.Braun and Medtronic. S. Eccleshall received research grants for investigator-initiated research and lecture honoraria from B. Braun. He also acts as a consultant for B. Braun, Medtronic, and MedAlliance.