Cory:
Unlock Your AI Assistant Now!
Transcatheter aortic valve implantation (TAVI) has emerged to become the preferred therapeutic approach for the treatment of symptomatic severe aortic stenosis (AS) across the spectrum of perioperative risk categories relative to surgical aortic valve replacement (SAVR)1. Against this background, research related to the durability of TAVI prostheses and sustainability of the treatment effect is a recognised priority, with the scope to derive incremental knowledge in order to refine bioengineering concepts and drive potential valve design modifications23.
In this issue of EuroIntervention, van den Dorpel and colleagues examine the prognostic value of invasive and echocardiography-derived transvalvular gradients before and after TAVI with two differing transcatheter heart valve (THV) designs, the intra-annular balloon-expandable (BEV) SAPIEN (Edwards Lifesciences) and the self-expanding (SEV) Evolut (Medtronic) valve, after propensity score matching in a retrospective cohort of 1,227 patients (436 SAPIEN 3 and Evolut matched pairs)4. All-cause mortality was significantly associated with invasive gradients but not with echocardiography-derived gradients from 30 days to 2 years post-TAVI. Using a spline curve regression analysis, the authors found an invasive gradient of >10 mmHg to best predict mortality. Mean gradients were consistently higher after TAVI using echocardiography compared to invasive measurements. When further substratified according to THV design, BEV consistently exhibited higher post-TAVI echocardiography-derived gradients than SEV, which were further amplified in the presence of smaller size THVs, higher ejection fraction, and higher stroke volume. Importantly, there were no differences in invasive gradients between THV types.
While most of these observations do not come as a surprise given the plethora of prior research on this topic56, the current study is the first to report a significant association between invasive gradients post-TAVI and mortality. This finding deserves further discussion as it suggests that attempts to decrease invasive pressure gradients prior to completion of the TAVI procedure may hold the potential to improve the clinical outcomes of our patients. To date, the only means to further decrease transvalvular TAVI gradients following implantation is to post-dilate the prosthesis using semi- or non-compliant balloons. It is of relevance to note that while prior studies assessing the routine post-dilatation of THVs were unable to provide evidence of decreased mortality, it may be argued that the absence of randomisation and the chance of achieving overall low gradients without routine post-dilatation in an unselected cohort of patients probably contributed to the lack of a treatment effect in this regard. In a previous study pooling data from the PARTNER I trial (cohorts A and B), patients randomised to TAVI and the non-randomised continued access cohort did not derive a benefit when post-dilatation was performed as compared to those not receiving post-dilatation after TAVI. As a matter of fact, post-dilatation was associated with a signal of harm, with a trend towards increased 1-year mortality7, thereby questioning the relationship between elevated invasive gradients and mortality that is suggested by the current study. On the other hand, the decision to post-dilate a THV is often made for a multitude of reasons, including THV underexpansion, the presence of relevant paravalvular regurgitation, or elevated gradients. Consequently, a consistent treatment effect derived from routine post-dilatation in an all-comers TAVI population may be difficult to ascertain in real-world practice given the multitude of confounding parameters impacting on mortality. In the current study by van den Dorpel et al, pre- and post-dilatation were more frequently performed in the SEV compared to BEV group (without reaching statistical significance), and there was no association with mortality, thus confirming the results of prior studies addressing this issue.
The most likely explanation for the significant discrepancy between echocardiography-derived and invasive transvalvular gradients, as reported in the study by van den Dorpel et al, is the presence of pressure recovery in patients with AS and, more so, following correction of the disease state by TAVI. Pressure recovery was reported to be a relevant explanation for the discrepancy between echocardiography-derived and invasive gradients in vitro8 and can be described as an increase of pressure downstream from a stenosis due to reconversion of kinetic into potential energy8910. Since continuous-wave Doppler measures the highest velocity across a stenosis, while invasive catheters derive the recovered pressure some distance away from the aortic valve, Doppler gradients are known to be higher than catheter gradients1112. While this phenomenon occurs in both native and diseased aortic valves, its magnitude may be amplified after correction of AS with THVs. More importantly, different THV designs may exhibit different degrees of pressure recovery and consequently exhibit a different delta of invasive and echocardiography-derived pressure gradients (Figure 1). While the scientific foundation of this phenomenon seems robust, its application in clinical practice may be intricate, and its contribution to the clinical performance of individual THV platforms difficult to distil. BEV and SEV are well known to exhibit differential haemodynamic valve functionality, where the supra-annular valve designs inherent to SEVs offer the advantage of lower echocardiography-derived transvalvular gradients after TAVI. The first randomised head-to-head comparison of BEV and SEV, the CHOICE trial13, previously reported significantly lower echocardiography-derived gradients in SEV relative to BEV, while invasively measured gradients were similar and negligible among groups, thus confirming the discrepancy reported in the study of van den Dorpel et al. Whether this advantage will manifest clinical benefits, such as lower rates of prosthesis-patient mismatch or structural valve deterioration/failure in the long term, or perhaps even lower mortality, is unproven. While the authors of the current study have contributed to our understanding of the impact of elevated invasive gradients after TAVI, the differential role of THV design in this regard remains debatable. Only long-term follow-up of THV-specific randomised clinical trials will help decipher individual valve performance.
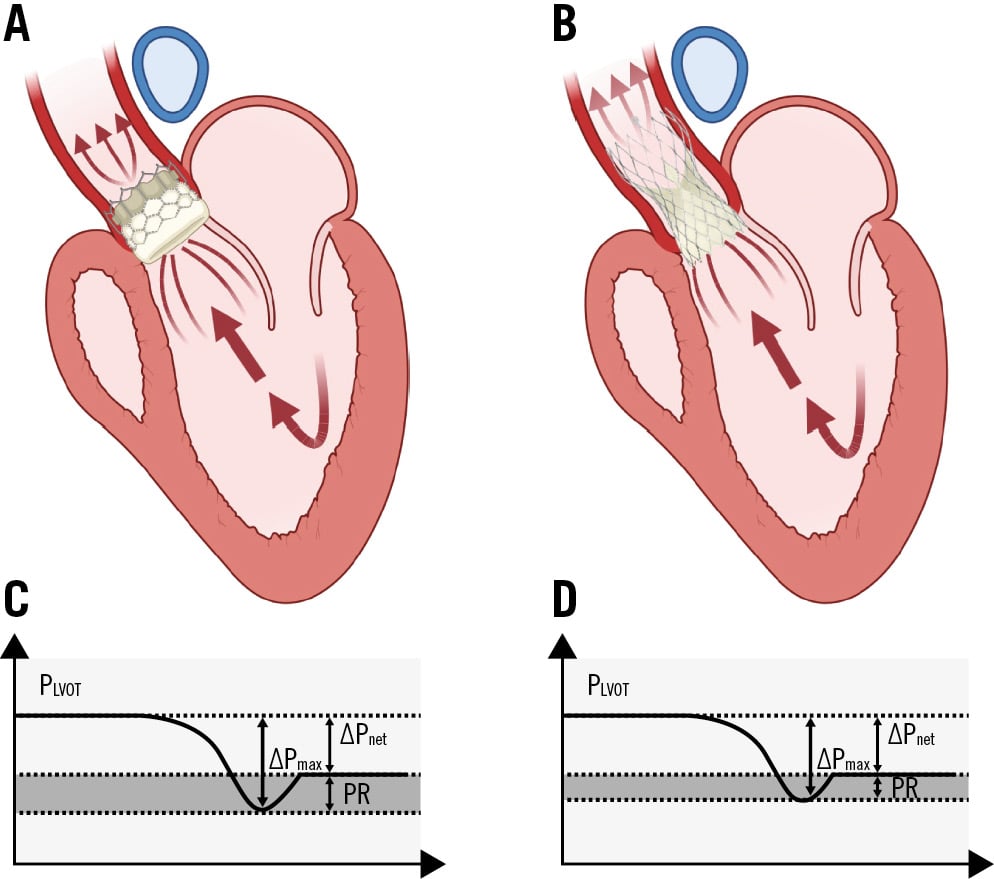
Figure 1. The pressure recovery phenomenon. Illustration of the pressure recovery phenomenon in balloon-expandable, intra-annular (A) and self-expanding, supra-annular (B) transcatheter heart valves. Note, greater pressure recovery is observed with balloon-expandable (C, shaded area) compared to self-expanding (D, shaded area) transcatheter heart valves, resulting in discrepancy between echocardiography-derived and invasively measured gradients. ΔPmax: maximum pressure gradient; ΔPnet: net pressure gradient; PLVOT: left ventricular outflow tract pressure; PR: pressure recovery
Conflict of interest statement
M. Joner reports personal fees from OrbusNeich, AstraZeneca, and Recor Medical; grants and personal fees from Biotronik, Boston Scientific, and Edwards Lifesciences; and grant support from Amgen outside the submitted work; and has received funding from the German Center for Cardiovascular Research: DZHK (FKZ 81Z0600502; FKZ 81X2600526) and from the Leducq Foundation (grant agreement number 18CVD02). D. Mylotte reports personal fees from Boston Scientific, Medtronic, and MicroPort; and institutional research grants from Boston Scientific.