Cory:
Unlock Your AI Assistant Now!
Despite randomised clinical trial data, there has been long-standing controversy and debate about whether proton pump inhibitors (PPIs) raise ischaemic risk in the context of dual antiplatelet therapy. Some observational studies have suggested an association between PPI use and higher rates of ischaemic events, but these studies were all confounded by the fact that sicker patients were the ones being prescribed the PPIs. An insightful analysis from the Veterans Affairs Healthcare System showed the potential misclassification of angina as gastro-oesophageal reflux, with PPI use essentially serving as a proxy for undetected and untreated coronary artery disease in some cases1. The prior observational studies were, in part, undertaken because of the suggestion in platelet function studies of an interaction between clopidogrel and PPIs, in particular older PPIs such as omeprazole. However, these pharmacokinetic and pharmacodynamic interactions have not consistently been shown to predict cardiovascular outcomes2. In fact, the randomised COGENT trial in acute coronary syndrome and stented patients demonstrated no increase in ischaemic events during the critical 6 months after presentation in patients receiving both clopidogrel and omeprazole but, rather, showed a significant reduction in gastrointestinal events34. The COMPASS trial subsequently confirmed the reduction in gastroduodenal bleeding with prophylactic proton pump inhibition in patients receiving antithrombotic therapy56. Nevertheless, controversy has persisted.
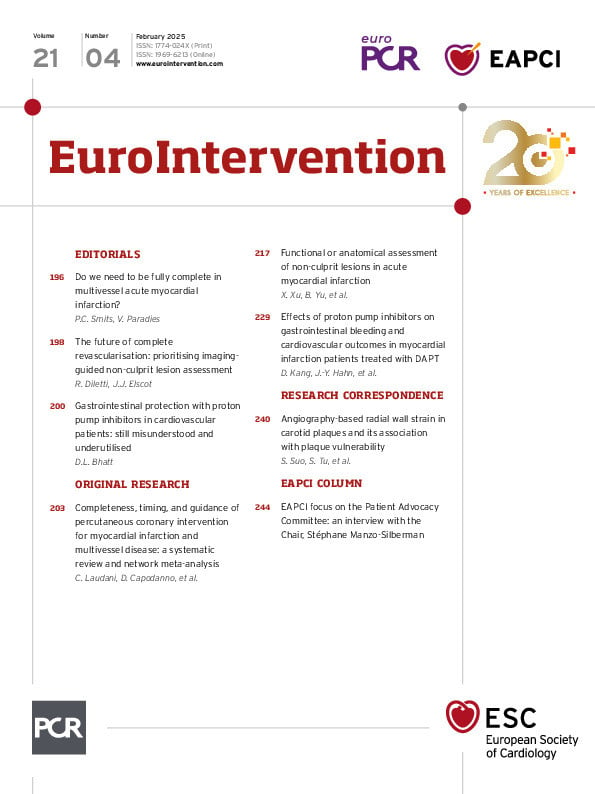
In this issue of EuroIntervention, Kang et al have carefully performed a large propensity-matched observational analysis that shows no relationship between PPI use, antiplatelet therapy, and an increase in ischaemic events7. Examining a nationwide Korean claims database, the authors studied patients with acute myocardial infarction undergoing percutaneous coronary intervention receiving dual antiplatelet therapy. Of these patients, 30% were receiving PPIs. Confirming what was seen in the COGENT trial, there was a significantly lower rate of major gastrointestinal bleeding with no increase in major adverse cardiac or cerebrovascular events. The same favourable patterns with respect to efficacy and safety were seen regardless of the specific PPI or antiplatelet agent. The gastrointestinal bleeding risk in this population was low, and there was still benefit, as was also the case in COGENT; in a population with a higher baseline bleeding risk, the absolute benefits would, of course, be expected to be even larger.
There is an inherent variability to clopidogrel response. Certain PPIs may affect this, but there are multiple other factors that likely dwarf the contribution to variability in clopidogrel response attributable to PPIs, such as smoking, genetic polymorphisms, diabetes, weight, and non-adherence28. For those physicians who remain worried about an omeprazole interaction with clopidogrel, any such pharmacokinetic and pharmacodynamic interaction is not really present with more contemporary PPIs which are also now available in generic form8. As well, prasugrel and ticagrelor do not seem to be subject to these interaction concerns.
The aspirin dose for chronic cardiovascular prevention has also been debated, but the majority of data support using 75 mg to 100 mg daily, which confers a slightly lower gastrointestinal bleeding risk compared with higher doses. However, the protective benefit of PPIs persists even with lower aspirin dosing9. Aspirin formulation is another consideration. In some parts of the world such as the United States, enteric-coated aspirin is the predominant form used in non-acute settings. Data exist that show greater antiplatelet variability in response to enteric-coated aspirin10. Most physicians seem unaware of the lack of quality data supporting a benefit of the enteric coating on gastrointestinal bleeding. On the other hand, avoidance of concomitant non-steroidal anti-inflammatory drugs (NSAIDs) is good advice for patients on antithrombotic therapy to further reduce gastrointestinal bleeding risks.
Prevention of gastrointestinal bleeding is indeed a worthwhile goal. While intracranial haemorrhage is the most feared bleeding complication, gastrointestinal bleeding is the most common manifestation of major bleeding with antithrombotic therapy. This risk is highest soon after initiating antithrombotic therapy but persists for the entire duration of antithrombotic use. PPIs can greatly reduce this risk. Beyond the obvious undesirability of the gastrointestinal bleeding event itself, there may be secondary harms. Major bleeding tends to prompt the body to shift to a prothrombotic state, which might then help precipitate ischaemic events. The bleeding episode may lead the treating physicians to withhold medications such as beta blockers, antihypertensive agents, or even statins, as well as some or all of the antithrombotic agents a patient is receiving. Some of these actions, perhaps appropriate in an acute setting, may inadvertently persist after the time of discharge, depriving patients of the cardiovascular protective effects these drugs may have had. Thus, gastrointestinal bleeding can set off a cascade of events that may increase the risk of ischaemic complications even beyond the resolution of an acute bleeding episode.
Cardiologists should routinely evaluate gastrointestinal bleeding risks. In patients who have had upper gastrointestinal bleeding, testing for H. pylori should be considered, most often in conjunction with referral to a gastroenterologist. Tobacco cessation is also important, as smoking does seem to be a risk factor. In suitable candidates, minimisation of the duration of dual antiplatelet therapy can help reduce bleeding risks. After dual antiplatelet therapy, de-escalation to clopidogrel monotherapy instead of aspirin monotherapy also decreases gastrointestinal bleeding. In patients with atrial fibrillation who require stenting, long-term full-dose triple antithrombotic therapy should be avoided. For those who develop gastrointestinal bleeding on ticagrelor – a reversible antiplatelet agent – a monoclonal antibody that reverses its antiplatelet effect is in development. Evaluation for PPI prophylaxis is an essential part of the overall strategy to decrease bleeding, with some evidence even suggesting there may be greater adherence to aspirin therapy due to less dyspepsia.
In conclusion, hopefully this study by Kang et al will put to rest the controversy regarding PPI interactions with antiplatelet therapy7. Multiple prior observational analyses, and likely future ones as well, do not appropriately control for the inherent confounding from PPI use in sicker patients. This has led to other spurious associations of PPI use with various side effects, in addition to the issue of antiplatelet therapy interactions. In appropriately selected patients, PPIs should be utilised and can provide substantial protection against gastrointestinal bleeding and its many potential consequences.
Conflict of interest statement
D.L. Bhatt discloses the following relationships - advisory board: Angiowave, Bayer, Boehringer Ingelheim, CellProthera, Cereno Scientific, Elsevier Practice Update Cardiology, E-Star Biotech, High Enroll, Janssen, Level Ex, McKinsey, Medscape Cardiology, Merck, MyoKardia, NirvaMed, Novo Nordisk, PhaseBio, PLx Pharma, Stasys, and Tourmaline Bio; board of directors: American Heart Association (New York City); Angiowave (stock options), Bristol-Myers Squibb (stock), DRS.LINQ (stock options), High Enroll (stock); consultant: Broadview Ventures, GlaxoSmithKline, Hims, SFJ, and Youngene; data monitoring committees: Acesion Pharma, Assistance Publique-Hôpitaux de Paris, Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute, for the PORTICO trial, funded by St. Jude Medical, now Abbott), Boston Scientific (Chair, PEITHO trial), Cleveland Clinic, Contego Medical (Chair, PERFORMANCE 2), Duke Clinical Research Institute, Mayo Clinic, Mount Sinai School of Medicine (for the ENVISAGE trial, funded by Daiichi Sankyo; for the ABILITY-DM trial, funded by Concept Medical; for ALLAY-HF, funded by Alleviant Medical), and Novartis, Population Health Research Institute, Rutgers University (for the NIH-funded MINT Trial); honoraria: American College of Cardiology (Senior Associate Editor, Clinical Trials and News, ACC.org; Chair, ACC Accreditation Oversight Committee), Arnold and Porter law firm (work related to Sanofi/Bristol-Myers Squibb clopidogrel litigation), Baim Institute for Clinical Research (formerly Harvard Clinical Research Institute; RE-DUAL PCI clinical trial steering committee funded by Boehringer Ingelheim; AEGIS-II executive committee funded by CSL Behring), Belvoir Publications (Editor-in-Chief, Harvard Heart Letter), Canadian Medical and Surgical Knowledge Translation Research Group (clinical trial steering committees), CSL Behring (AHA lecture), Cowen and Company, Duke Clinical Research Institute (clinical trial steering committees, including for the PRONOUNCE trial, funded by Ferring Pharmaceuticals), HMP Global (Editor-in-Chief, Journal of Invasive Cardiology), Journal of the American College of Cardiology (Guest Editor; Associate Editor), K2P (Co-Chair, interdisciplinary curriculum), Level Ex, Medtelligence/ReachMD (CME steering committees), MJH Life Sciences, Oakstone CME (Course Director, Comprehensive Review of Interventional Cardiology), Piper Sandler, Population Health Research Institute (for the COMPASS operations committee, publications committee, steering committee, and USA national co-leader, funded by Bayer), WebMD (CME steering committees), and Wiley (steering committee); other: Clinical Cardiology (Deputy Editor); patent: Sotagliflozin (named on a patent for sotagliflozin assigned to Brigham and Women’s Hospital who assigned to Lexicon; neither I nor Brigham and Women’s Hospital receive any income from this patent); research funding: Abbott, Acesion Pharma, Afimmune, Aker BioMarine, Alnylam, Amarin, Amgen, AstraZeneca, Bayer, Beren, Boehringer Ingelheim, Boston Scientific, Bristol-Myers Squibb, Cardax, CellProthera, Cereno Scientific, Chiesi, CinCor, Cleerly, CSL Behring, Eisai, Ethicon, Faraday Pharmaceuticals, Ferring Pharmaceuticals, Forest Laboratories, Fractyl, Garmin, HLS Therapeutics, Idorsia, Ironwood, Ischemix, Janssen, Javelin, Lexicon, Eli Lilly, Medtronic, Merck, Moderna, MyoKardia, NirvaMed, Novartis, Novo Nordisk, Otsuka, Owkin, Pfizer, PhaseBio, PLx Pharma, Recardio, Regeneron, Reid Hoffman Foundation, Roche, Sanofi, Stasys, Synaptic, The Medicines Company, Youngene, and 89Bio; royalties: Elsevier (Editor, Braunwald’s Heart Disease); site co-investigator: Abbott, Biotronik, Boston Scientific, CSI, Endotronix, St. Jude Medical (now Abbott), Philips, SpectraWAVE, Svelte, and Vascular Solutions; trustee: American College of Cardiology; and unfunded research: FlowCo.